Послеродовые кровотечения (ПРК) являются достаточно распространенным осложнением послеродового периода и могут возникать даже у пациенток без предрасполагающих факторов риска, являясь одной из основных причин материнской заболеваемости, в том числе в развитых странах [1]. Считается, что большинство случаев материнской смертности, связанной с кровотечением, можно предотвратить [2]. Частота ПРК в мире составляет около 5% и не имеет тенденции к снижению. Большинство пациенток адекватно реагируют на лечение ПРК первой линии, которое включает утеротоники, массаж матки и транексамовую кислоту. Однако 10–20% этих пациенток в конечном итоге не реагируют на вмешательства первой линии. Эта подгруппа рефрактерных случаев ПРК составляет большую часть заболеваемости и смертности, связанных с ПРК. Рефрактерное ПРК – это кровотечение, требующее использования вмешательств второй линии [3]. При возникновении массивных рефрактерных ПРК нередко выполняется экстренная гистерэктомия, которая приводит к потере репродуктивной и менструальной функций, сопровождается значительными нарушениями в гипоталамо-гипофизарно-яичниковой системе [4]. Гистерэктомия до настоящего времени остается неотложным оперативным вмешательством, которое направлено на спасение жизни родильницы при неконтролируемом кровотечении [5]. Кроме того, для уменьшения операционной кровопотери и достижения надежного гемостаза в настоящее время предложено множество различных альтернативных методов, включая методы компрессионного гемостаза, т.е. методы, основанные на компрессии (сдавлении) матки и/или магистральных сосудов.
Liu L.Y. et al. к мероприятиям второй линии при рефрактерных ПРК относят компрессионные мероприятия (компрессию аорты или бимануальную компрессию матки), внутриматочную баллонную тампонаду и применение непневматической противошоковой одежды при необходимости транспортировки [3].
Наружные компрессионные методы
Использование бимануальной компрессии матки или внешней компрессии брюшного отдела аорты для лечения ПРК вследствие атонии матки после вагинальных родов в качестве меры временного гемостаза на этапе транспортировки в операционную или на период ожидания квалифицированной помощи рекомендуется ВОЗ (2021) и FIGO (2022) [6, 7], а также профессиональными медицинскими сообществами Великобритании (Британский Королевский колледж акушеров-гинекологов, RCOG (2017)), России (Российское общество акушеров-гинекологов, РОАГ (2021)), Германии (Немецкое общество гинекологии и акушерства, DGGG (2018)) [8–10].
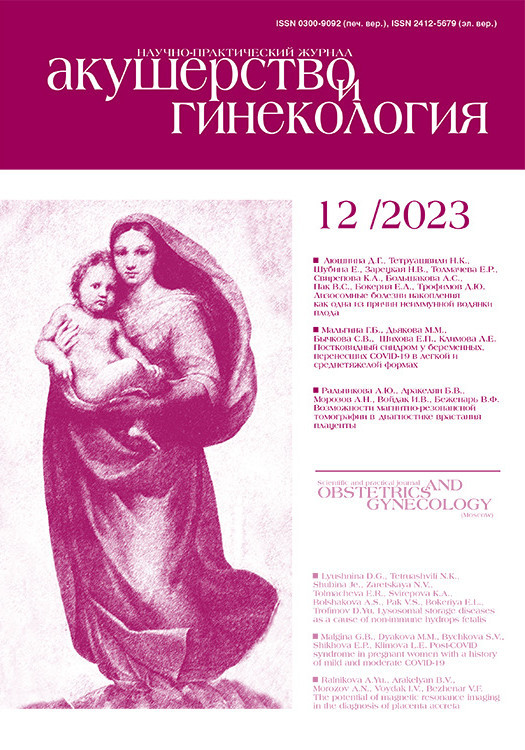
Идея компрессионного гемостаза при ПРК принадлежала ранее профессору Г.А. Ушаковой (Кемерово); в своей кандидатской диссертации на тему «Метрогемостат в профилактике и лечении ранних послеродовых кровотечений» (1966) она доказала эффективность комбинированного использования метрогемостата (алюминиевая чаша с фиксирующими резинками), который накладывался на переднюю брюшную стенку, и внутриматочной тампонады марлевым тампоном в профилактике у пациенток высокого риска и лечении ПРК. На рисунке 1 представлено фото родильницы в раннем послеродовом периоде с метрогемостатом, наложенным на переднюю брюшную стенку (фото из архива проф. Г.А. Ушаковой, 1966 г.).
Компрессионный гемостаз c применением эластичного бинта, предложенный Palacios-Jaraquemada J. [11] и Kimmich N. [12], до настоящего времени не регламентирован в Российской Федерации, поскольку описание его эффективного применения имеется только у небольшого количества пациенток. Palacios-Jaraquemada J. et al. у 10 пациенток с массивным ПРК после применения наружной компрессии аорты, лапаротомии и определения источника кровотечения накладывали компрессионные швы и вводили внутриматочно фибриновый клей с последующим наложением наружной эластичной повязки на матку для ее сдавления. После остановки кровотечения, через 45 минут, повязку снимали и зашивали матку и брюшную полость [11].
Kimmich N. et al. представили результаты применения методики компрессии матки путем обматывания ее эластичным бинтом у трех пациенток с атонией матки при операции кесарева сечения [12].
В Российской Федерации Михайловым А.В. и соавт. (2018) запатентован способ лечения ПРК путем наложения эластичного бинта по направлению от дна матки к нижнему сегменту, не доходя до раны, обеспечивая максимальное сжатие тела матки до нижнего сегмента не менее чем на 30 минут. Эффективное применение данной методики описано у трех пациенток [13].
РОАГ (2021) рекомендует при ПРК использование следующих органосберегающих технологий, основанных на компрессии: компрессия брюшного отдела аорты, бимануальная компрессия матки, деваскуляризация, компрессионный шов на матку, управляемая баллонная тампонада (УБТ) [8].
При этом каждый из методов имеет показания, противопоказания, условия, ограничения, осложнения и эффективность.
Общепризнано, что выбор метода гемостаза зависит от предпочтений хирурга и оснащения клиник. Каждый из этих методов может применяться как самостоятельно, так и в комплексе с другими методами [14]. Однако следует подчеркнуть, консервативные меры по сохранению матки допустимы только в том случае, если пациентка гемодинамически стабилизирована и не имеет опасного для жизни кровотечения [5].
Методы деваскуляризации
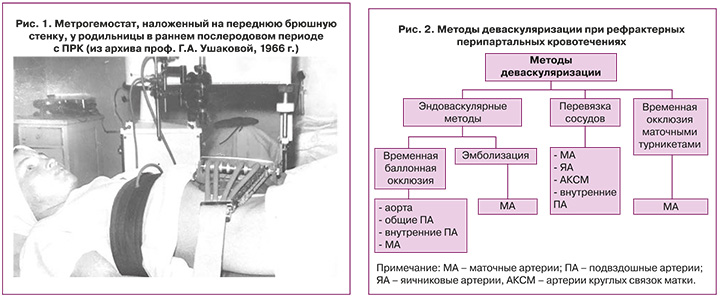
К методам деваскуляризации, которые могут применяться для управления рефрактерными перипартальными кровотечениями, относятся эндоваскулярные методы (временная баллонная окклюзия и эмболизация), перевязка магистральных сосудов и окклюзия с применением турникетных жгутов. На рисунке 2 представлены методы деваскуляризации, которые могут применяться при рефрактерных перипартальных кровотечениях.
Метод комплексного компрессионного гемостаза был предложен при выполнении органосохраняющего оперативного родоразрешения у пациенток с врастанием плаценты Шмаковым Р.Г. и соавт. (2017) [15]. Далее эта методика продолжала активно изучаться у пациенток с различными степенями патологического прикрепления плаценты как изолированно, так и в сочетании с другими методами деваскуляризации [16–18].
Шмаковым Р.Г. и соавт. (2019) был представлен пятилетний опыт применения методики наложения турникетных жгутов билатерально на основание широких связок с захватом маточной трубы, мезосальпинкса, собственной связки яичника и шеечно-перешеечной области матки в проекции деления маточной артерии на восходящую и нисходящую ветвь у 98 беременных с врастанием плаценты. Кровопотеря закономерно была больше, гистерэктомия требовалась чаще у пациенток с более выраженной степенью врастания плаценты: 9,4% против 33,3% (p=0,038) [18].
В англоязычной литературе для обозначения альтернативных методов лечения перипартальных гипотонических кровотечений, основанных на компрессии, чаще применяется термин «механический гемостаз» [19].
Понятие «комплексный компрессионный гемостаз» впервые в Российской Федерации регламентировано в 2023 г. в клинических рекомендациях у пациенток с врастанием плаценты [14]. В этом документе комплексный компрессионный гемостаз представлен наряду с другими органосберегающими альтернативными подходами, такими как эндоваскулярные методы (эмболизация маточных артерий (ЭМА), баллонирование внутренних или общих подвздошных артерий, аорты), деваскуляризация матки (перевязка маточных артерий, перевязка/временная окклюзия внутренних подвздошных артерий/окклюзия общих подвздошных артерий).
Перевязка сосудов
Считается, что впервые в эксперименте перевязку маточных и яичниковых артерий у беременных собак произвел А.А. Муратов (1879). Технология перевязки маточных сосудов при маточных кровотечениях была подробно описана в дальнейшем в трудах российских ученых в начале XX в. (Снегирев В.Ф., Алтухов Н., 1907; Никольский A.M., 1912; Губарев А.П., 1928). Waters (1952) описал перевязку маточных артерий с хорошими результатами при 8 случаях серьезных кровотечений в послеродовом периоде [20]. Цирюльниковым М.С. в 1979 г. были описаны техника (тройное нисходящее лигирование) и результаты двусторонней перевязки круглой связки, маточно-яичниковой и маточной артерий при обильном кровотечении в третьем периоде родов. Автор выполнил эту процедуру сначала у 9 обезьян, затем у 24 женщин [21]. Перевязка маточных артерий является высокоэффективной и в настоящее время наиболее часто выполняемой хирургической операцией при ПРК. Однако, блокируя кровоснабжение тела матки, возможно уменьшение кровотока в яичниковых артериях, что может вызвать серьезные нарушения функции яичников [22].
Liu W. et al. проводили сравнительную оценку эффективности и безопасности перевязки маточных артерий (n=50) и ЭМА (n=50) у пациенток с ПРК после операции кесарева сечения. После обеих процедур восстановление кровотока и гормональной функции яичников происходило одинаково, восстановление менструального цикла зарегистрировано через 41–42 недели. Однако при перевязке маточных артерий регистрировалась статистически значимо меньшая кровопотеря, чем при ЭМА, соответственно 1627±403,62 и 1778±429,16 мл (р=0,039). При ЭМА объем кровопотери был больше за счет более длительного периода подготовки. Однако продолжительность самого вмешательства была больше при перевязке маточных артерий, чем при ЭМА, – 60,46±13,70 и 44,49±7,43 минут (р=0,032) [23].
Пошаговая деваскуляризация матки более четко регламентирована рекомендациями RCOG (2017), в которых описана последовательная перевязка первоначально одной маточной артерии, далее – обеих маточных артерий, затем – нисходящей ветви маточных артерий, далее – одной яичниковой артерии и в завершение – обеих яичниковых артерий [9]. DGGG (2018) также определяют возможность, помимо перевязки маточной артерии, для гемостаза использование ступенчатой деваскуляризации матки, техника которой предполагает 5 последовательных этапов лигирования восходящих и нисходящих ветвей маточных артерий и коллатеральных ветвей яичниковых артерий [10].
Эмболизация маточных артерий
ЭМА, по мнению FIGO (2022), может быть одной из консервативных мер лечения ПРК, если для ее использования доступны технические условия и квалифицированные человеческие ресурсы [7]. Возможность проведения этой интервенции при ПРК регламентирована также и другими профессиональными медицинскими сообществами [9, 10].
Селективная ЭМА при ПРК применяется с 1979 г. Осложнения при выполнении этой процедуры встречаются, по данным Cheong J.Y. (2014), в 14,5% случаев, в 10,3% случаев это осложнения, связанные с кровотечением (острая почечная, печеночная недостаточность, отек легких), а в 6% – осложнения, связанные непосредственно с ЭМА: лихорадка, гематома, некроз матки, требующий гистерэктомии (в 2,7% случаев) [24].
По данным Zhang X.Q. et al., частота осложнений ЭМА достигает 22,8%; при этом постэмболизационный синдром диагностируется у 13,2%, нарушения менструального цикла выявляются у 22,8%, массивный некроз – у 4,9%, невропатия – у 9,38%, гематома – у 2,91%, осложнения самой процедуры – у 3%. При этом гистерэктомия в связи с возникшими осложнениями выполняется у 5,6%, а гистерэктомия при последующей беременности – у 22,7% женщин. При этом так называемая техническая эффективность зарегистрирована у 99,3%, а клиническая эффективность – у 99,5% женщин [25].
По данным Kosai S. et al., эффективность ЭМА при ПРК составляет 87,2%, а основным фактором риска неудачной попытки ЭМА является анатомическая особенность – сужение маточной артерии при цифровой ангиографии, поэтому процедура ЭМА должна проводиться после устранения вазоспазма [26].
Несмотря на то что ЭМА является высокоэффективной процедурой, сохраняющей фертильность, и даже описан случай успешных родов после четырех процедур ЭМА, имеются сведения о возможных плацентарных нарушениях, рецидивах ПРК и увеличении частоты невынашивания беременности после этой процедуры, что требует проведения дальнейших исследований [27].
Временная баллонная окклюзия магистральных сосудов
Временная баллонная окклюзия магистральных сосудов в настоящее время изучена достаточно хорошо; имеются данные по ее эффективности и безопасности у большого количества пациентов. В настоящее время считается, что наибольшая эффективность достигается при временной окклюзии брюшного отдела аорты [28–30].
Цхай В.Б. и соавт. провели анализ эффективности различных методов хирургического гемостаза у пациенток с врастанием плаценты. Авторами продемонстрировано, что идеального метода деваскуляризации при врастании плаценты до настоящего времени не существует; однако наибольшую эффективность демонстрируют метод временной баллонной окклюзии брюшной аорты и отечественный метод дистального компрессионного гемостаза [28].
Эффективность временной баллонной окклюзии аорты, внутренней и общей подвздошной артерий для профилактики ПРК, по данных различных авторов, представлена в таблице.

Курцер М.А и соавт. продемонстрировали эффективность временной баллонной окклюзии общей подвздошной артерии у 69 (98,6%) беременных женщин с врастанием плаценты в рубец на матке. При этом эндоваскулярные осложнения зарегистрированы у 4 (5,7%) рожениц: диссекция сосуда и формирование дефекта контрастирования артерии. У 2 (6,5%) пациенток в отдаленном периоде менструальная функция так и не восстановилась [45].
В 2010 г. специалисты из Великобритании (университетская клиника Святого Георгия, Лондон) предложили методику Triple-P как альтернативу перипартальной гистерэктомии при placenta percreta. Этот метод предполагал проведение периоперационной локализации верхнего края плаценты, деваскуляризации органов малого таза (временная баллонная окклюзия внутренней подвздошной артерии) и отделение плаценты с иссечением миометрия и последующим устранением дефекта миометрия (метропластика) [46].
В ретроспективном исследовании Pinas-Carrillo А. et al., основанном на результатах 50 пациенток c врастанием плаценты, которые прошли процедуру Triple-P с сентября 2010 г. по май 2017 г. в родильном отделении клиники Святого Георгия, средняя интраоперационная кровопотеря составила 2318 мл (диапазон: 400–7300 мл), а средняя продолжительность пребывания в больнице – 4 дня (диапазон: 2–8 дней). У 3 женщин (6,0%) развился артериальный тромбоз без каких-либо долгосрочных осложнений, гистерэктомия не проводилась [47].
В настоящее время считается, что, поскольку в 14% случаев установка баллона происходит до рождения плода, необходимы дальнейшие исследования для определения безопасности окклюзии аорты до родоразрешения [48].
Компрессионные швы на матку
В 1997 г. B-Lynch были впервые применены компрессионные швы на матку при ПРК. С тех пор разработано большое количество различных компрессионных швов на матку. До настоящего времени не было продемонстрировано доказательств высокого уровня, что какой-либо компрессионный шов имеет преимущества и обеспечивает лучший и более безопасный гемостаз при ПРК [49].
Выбор шва определяется клинической ситуацией и опытом хирурга. Так, по мнению Moleiro M.L. et al. (2019), при гипотоническом кровотечении приемлем любой вариант компрессионного шва, тогда как при placenta previa имеет преимущества шов по Cho или Hayman, а при placenta accreta – шов по Cho [50]. Тем не менее наиболее изученным является именно шов по B-Lynch; по данным метаанализа Nalini N. et al. (2022), который включал 30 исследований и 1270 пациенток, частота контролируемых кровотечений при применении этого шва составила 94%, частота гистерэктомий – 7%, совокупная частота хирургических осложнений – также 7% [51].
Позднее были предложены различные модификации продольного шва по Хайману, Нельсону, Берчу, Мансору, Матсубару, Сантра; поперечные швы по Хакеталу, Куабу; комбинированные продольно-
поперечные швы по Перейру; шов Радзинского–Рымашевского; шов Курцера; стандартный многогранный шов в нижнем маточном сегменте по Менгу; компрессионный шов с параллельной петлей; П-образный шов по Чо; сборочный компрессионный шов по Станоевику и т.д. [52–55].
В целом все компрессионные швы на матку имеют как преимущества, так и недостатки. Так, по мнению Бодыкова Г.Ж. и соавт. (2021), к их преимуществам относятся быстрота применения, эффективность до 90%, отсутствие необходимости специального инструментария, отсутствие влияния на репродуктивную и менструальную функции. Недостатками компрессионных швов являются риск прорезывания швов матки, повреждение мочеточников, облитерация цервикального канала, образование пиометры, синехий и гематомы в области воронко-тазовых связок [52].
По данным Kwong L.T., частота осложнений при наложении компрессионных швов на матку (по Б-Линчу/Хайману/Чо) и компрессионных швов в сочетании с дополнительными методами (перевязкой маточных артерий или ЭМА) была сопоставима и составила для вторичного кровотечения 14,8 и 11,9%, для эндометрита – 14,8 и 14,3%, для задержки продуктов зачатия – 3,7 и 9,5% соответственно [53].
Кроме того, разработаны различные варианты надплацентарного сборочного шва, например, по Баринову С.В. (2017) [56]; нами была предложена модификация надплацентарного шва – двусторонний кисетный шов на нижний сегмент матки, который в сочетании с перевязкой нисходящей ветви маточной артерии и УБТ продемонстрировал эффективность при предлежании плаценты и несостоятельности рубца на матке после иссечения [57].
Управляемая баллонная тампонада
В соответствии с рекомендациями ВОЗ (2021), FIGO (2022), РОАГ (2021), RCOG (2017), DGGG (2018) использование баллонной тампонады матки рекомендуется как эффективный нехирургический метод, который потенциально может улучшить выживание женщин с ПРК вследствие атонии матки после исключения задержки продуктов зачатия или разрыва матки как способствующего фактора [6–10]. УБТ является одной из современных технологий для контроля ПРК и предотвращения гистерэктомии и должна применяться при отсутствии эффекта от утеротонической терапии при ПРК как вмешательство первой линии для большинства женщин, у которых гипотония матки является единственной или главной причиной кровотечения [58]. Российские и немецкие клинические рекомендации регламентируют возможность применения при рефрактерных кровотечениях УБТ совместно с наложением гемостатических компрессионных швов [8, 10].
Сравнительное исследование, проведенное Ramler P.I. et al., показало одинаковую эффективность внутриматочной баллонной тампонады (n=50) и ЭМА (n=50) при лечении персистирующих ПРК. Гистерэктомия была проведена в 5 случаях в обеих группах, у 1 пациентки в группе ЭМА произошло тромбоэмболическое осложнение [59].
Систематический обзор и метаанализ Suarez S. et al., который включал 91 исследование, 4729 женщин (6 РКИ, 1 кластерное рандомизированное исследование, 15 нерандомизированных исследований и 69 серий случаев), продемонстрировал эффективность УБТ в 85,9% (ДИ 83,9–87,9%), в том числе при родоразрешении операцией кесарева сечения – в 81,7%, при вагинальных родах – в 87,0%. Авторами показано, что УБТ наиболее эффективна при атонии матки (87,1%) и предлежании плаценты (86,8%) и, напротив, наименее эффективна при врастании плаценты (66,7%) и задержке продуктов зачатия (76,8%) [60].
Краткосрочные осложнения при УБТ регистрировались значительно реже, чем при использовании компрессионных швов и методов деваскуляризации (перевязке сосудов, ЭМА), а на долгосрочные последствия (фертильность, частота живорождения, менструальный цикл) УБТ влияния не оказывала. Инфекционные осложнения регистрировались у 2,3–6,5% женщин после применения УБТ, разрывы шейки матки – в 1,7%, разрывы влагалища – в 4,8%, разрывы разреза на матке – в 1,9%, острая псевдообструкция толстой кишки – в 2,0%, перфорация матки – в 2,0% случаев [60].
Многие профессиональные сообщества в настоящее время рекомендуют использование двухбаллонной маточно-влагалищной системы, поскольку она дает дополнительные преимущества в виде компрессии сосудов нижнего сегмента матки [10].
Исследования последних лет продемонстрировали эффективность терапии рефрактерных ПРК при помощи внутриматочного устройства (система Jada). По сравнению с баллонной тампонадой матки, при которой для лечения атонии матки применяется внешнее давление на стенки матки, система Jada создает внутриматочный вакуум, вызывающий сужение кровеносных сосудов миометрия для гемостаза. Вакуум обычно применяется в течение как минимум часа после остановки кровотечения, чтобы предотвратить рецидив кровотечения. Эффективность данного устройства, по данным проведенных исследований, составила от 86 до 100% [3, 61].
Заключение
Анализ литературных данных показал, что в настоящее время проблема управления рефрактерными ПРК продолжает оставаться актуальной. Одобрены различные методы компрессионного гемостаза, которые успешно применяются как изолированно, так и в сочетании друг с другом. Однако данных о наиболее рациональной их последовательности, комбинации между собой и с другими методами недостаточно. Необходимы дальнейшие исследования в этом направлении.