Lypidome analysis of cervicovaginal fluid (CVF) in patients with vulvovaginal atrophy under exposure to dynamic quadripolar radiofrequency
Objective: To study specific features of cervicovaginal fluid lipidome in patients with vulvovaginal atrophy (VVA) in postmenopause under exposure to dynamic quadripolar radiofrequency (DQRF).Kazakova S.N., Apolokhina I.A., Chagovets V.V., Frankevich V.E., Teterina T.A., Tokareva A.O.
Materials and methods: The study included 60 patients aged 46–65 years (the mean age 54.8 (5.1) years) with the symptoms of VVA. All patients underwent treatment: dynamic quadripolar radiofrequency was used in the area of vulva and vagina in group 1 (4 procedures with 2-week intervals); DQRF with radioporation technique with application of cream containing 0.5 mg estriol was used in group 2 (4 procedures with 2-week intervals); and local hormonal treatment with cream containing 0.5 mg estriol was used in group 3 (8 weeks of treatment). Lipid extraction from cervicovaginal fluid was performed using modified Folch method at two-time points – before and 1 month after treatment.
Results: Lipidome analysis compared 3 groups of samples of cervicovaginal fluid– in 40 patients before and after exposure to DQRF and in 20 patients before and after treatment with local estrogens according to treatment regimen. 6 compounds were isolated. Their levels were statistically significantly higher in the group of patients who were exposed only to radiofrequency – Anandamide (18:2, n-6), DG 18:0/18:0/0:0, DG 18:0/16: 0/0:0, LTB4-dimethylamide, N-hydroxy arachidonoilamine, Virodhamin. The levels of Anandamide (18:2, n-6), LTB4-dimethylamide, N-hydroxy arachidonoilamine and Virodhamin were statistically significantly lower in patients who were exposed to radiofrequency in combination with estrogens for treatment of VVA in postmenopause.
Conclusion: This article describes an innovative approach to alternative treatment of women with VVA in postmenopause using DQRF. The results of lipidome analysis of cervicovaginal fluid after exposture to DQRF are published for the first time. Further study and research in the field of high energy methods for VVA treatment are necessary to assess the effectiveness and safety of long term radio wave exposure.
Keywords
Vulvovaginal atrophy (VVA) is one of the most well-known and widespread physiological processes of reproductive aging. Estrogen deficiency that occurs during the menopause can lead to changes and loss of elasticity of the vaginal wall along with decreased cervical secretions and thinning of the vaginal epithelium [1]. Urogenital atrophy symptoms including vaginal dryness, itching, discomfort, burning worsen with the decreased estrogen levels [2]. VVA is accompanied by painful intercourse and leads to the symptoms and conditions, such as urinary incontinence, urinary urgency, atrophic cystourethritis. Among the patients with VVA, urogenital infections [3], dyspareunia and vaginal bleeding during sexual intercourse are most common, and significantly reduce quality of life for socially active category of women.
VVA is most common in postmenopausal women. Given the fact that the number of women of this age is steadily increasing in modern society, especially in the developed countries, there is a reason to assume that the issue of treatment of VVA will become more and more relevant over time.
According to the study in North America, most women spend approximately 30% of their lives in menopause [4], but there is still no a clear awareness of patients about feasibility and treatment effects of this condition.
It is known that estrogens are the main regulators of physiological processes in the vagina. It is believed that loss of estrogens induces connective tissue proliferation, fragmentation of elastic fibers, hyalinization of collagen fibers leading to manifestation of VVA symptoms. [5].
Thus, collagen content as a part of the connective tissue in the vaginal wall and estrogen-sensitive structure, decreases as estrogen deficiency progresses, which is part of the connective tissue of the vaginal wall and is an estrogen-sensitive structure, decreases with increasing estrogen deficiency.
In the study by Vicariotto et al. (2016), 25 patients in two groups (with vaginal relaxation syndrome and VVA/the genitourinary syndrome of menopause (GSM)), respectively, underwent radiofrequency (RF) treatment – 5 and 4 sessions of RF lifting every 14 days. Working temperature in target tissues in the vagina during the procedure was 42°C – (temperature range 40°C–43°C) (in patients with vaginal relaxation syndrome); 40°C (temperature range 40°C–42°C) (in patients with VVA/GSM) [6]. In both groups of patients, disturbing symptoms decreased, including dysuria/urinary incontinence, and quality of sexual life improved. At the same time, the results maintained during 12 months of follow-up [7].
In 2020, North American Menopaus Society (NAMS) published recommendations for GSM treatment, where energy therapies were reported for the first time, including the effects of radiofrequency radiation exposure (level of evidence: grade C) [5].
One of the promising methods of RF energy-based treatment of VVA/GSM is radiofrequency therapy (RF lifting), which has been used quite successfully in aesthetic surgery and cosmetology for rather a long time to repair skin defects on face and body [8].
Radio frequency device supplies electromagnetic waves, heat is transferred through them and cause indirect heating of tissues in the appropriate area. The therapeutic effect occurs due to reactivated function of fibroblasts and connective tissue and regeneration of collagen and elastin fibers in the subepithelial layers of vaginal vestibule and vaginal wall [9]. Electromagnetic waves have effect mainly on the dermis and submucosa, which are composed of cells and a matrix containing 60–70% water. In adults, about 70% of extracellular fluid is associated with connective tissue proteins (collagen, elastin and another proteins). One of essential characteristics of collagen is that it contains a large amount of water. Collagen provides superior hydration, has electric and piesoelectric properties. It has been established that water plays a significant role in the mechanism of self-assembly of collagen molecules, fibril formation, as well as in the mechanisms of biochemical activity and functioning of collagen in the extracellular space. The biological effect of electromagnetic waves occurs due to water molecules in the molecules of collagen and elastin, where the proteins make transition from functional passive to functional active state. As a result of intramolecular changes, hydrating water is activated, that in turn, causes conformational structural changes in collagen molecules, and collagen becomes more hydrated. These molecular processes lead to increase of metabolism in skin and mucous cells, including fibroblasts [10].
Radiofrequency therapy has been used for a long time in women with stress urinary incontinence (SUI) and helps to achieve good and stable clinical results [11]. Relief of SUI was accompanied by positive histological changes and disappearance of VVA/GSM symptoms in 70% of patients [12].
The study, that was carried out in Brazil in 2019, reported that 55 women received radiofrequency (RF) treatment of CCA/GSM. The average age of women was 59.8 ± 4.2 years, and menopause lasted on average 15.4±4.5 years. After treatment, the percentage of Lactobacillus spp. increased. Also, vaginal pH balance gradually decreased and the scores of vaginal health index (VHI) became higher: the mean values of VHI before and after treatment were 13.2±5.6 and 22.5±3.7 points, respectively [13].
The procedures of radio wave exposure were performed using dynamic quadripolar radiofrequency (DQRF) device EVA (Novavision, Italy). Radio wave radiation frequency of the device was 1–1.3 MHz. For treatment of VVA, two sensors were used for vaginal exposure and external exposure to the vulva.
RF radiation was delivered to the tissue through 4 ring-shaped electrodes, which were automatically configured for circulation of radio frequency current flows between the electrodes. They alternately emited and received radio waves, dynamically changing their configuration every 5 seconds, depending on the selected software for EVA device.
In modern medicine, a possibility of targeted drug delivery to the lesion is of particular interest. Embedded system of Ultra-pulsed Radioporation (UPR) provides the function of frequency adaptation of radio waves to open water channels in the cells, facilitates transmucosal and transdermal permeation of drugs. UPR is used to enhance the therapeutic effect of the procedure with using the drugs (for example, cream containing estriol for treatment of VVA/GSMS, cream containing glucocorticosteroids for treatment of vulvar lichen sclerosus and other conditions) [14].
Due to the use of special software for controlled temperature regulation during DQRF exposure, the procedure did not cause burns and other undesirable outcomes.
In our study we suggested that DQRF exposure to the vaginal and vulvar mucosa could change the vaginal metabolome in postmenopausal women with VVA.
The purpose of the study was to investigate specific features of cervicovaginal fluid (CVF) lipidome in postmenopausal patients with VVA under e dynamic quadripolar radiofrequency (DQRF) exposure.
Materials and methods
This prospective interventional study included 60 women.
Inclusion criteria were: the age of women from 45 to 65 years (the average age 54±4.2 years), the length of the time spent in menopause more than 1 year. Exclusion criteria were: unsatisfactory state of the skin and mucosa after previous procedures with laser, pulsed and low-frequency and RF devices used for treatment of fibrosis, thinning skin (parchment-like skin), systemic diseases of the connective tissue, urogenital infections, skin and mucosal injuries in the affected area, current oncological diseases or in the past medical history, precancerous conditions of the vulva, the use of cardiac pacemaker, taking painkillers on the day of the procedure.
The patients with the symptoms of VVA were recruited upon referral to the Department of Aesthetic Gynecology and Rehabilitation of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of Russia (further referred to as “the Center”) from September 2019 to August 2021. All patients have signed informed consent to participate in the study. The approval of the Ethics Committee for Biomedical Research of the Center was obtained before starting the study.
The women were divided into three groups divided into three groups using spreadsheets of random numbers:
Group 1 received treatment using DQRF exposure to the area of vulva and vagina (4 procedures with 2-week intervals);
Group 2 received treatment using DQRF and Ultra-pulsed Radioporation and application of cream containing 0.5 mg estriol (4 procedures with 2-week intervals);
Group 3 received local hormonal treatment with cream containing 1mg/1g estriol. Dose regimen was vaginal administration of 0.5 mg estriol every other day during 2 weeks (up to 8 weeks).
The patients participating in the study underwent clinical laboratory testing in total test volume.
CVF samples were obtained from all patients before commencing the study and one month after completion of treatment.
Lipids extraction from CVF was performed with modified Folch method: 1000 µL of CHCl3/MeOH 2/1 v/v was added to 200 μl of CVF and kept in ultrasonic bath for 10 minutes. The sample was mixed by Vortex for 10 seconds, then centrifuged for 5 minutes at 15000 rpm. The bottom organic layer (100 μl) was transferred to a separate vial. CHCl3/MeOH 2/1(500 μl) was added to the remaining mixture and centrifuged for 5 minutes at 15000 rpm. The bottom organic layer (100 μl) was transferred to the previosly selected layer and dried by blowing a stream of nitrogen, then redissolved in 200 μl IPA/ACN 1/1 v/v. The purity of chemicals used for extraction was evaluated by LC-MS (Sigma Aldrich, USA).
Lipid extracts were analyzed by using liquid chromatography Dionex UltiMate 3000 (Thermo Scientific, Germany) system, which was connected to Maxis Impact qTOF mass analyzer with an ESI ion source (Bruker Daltonics, Germany). The samples were separated by reversed-phase high performance liquid chromatography using Zorbax SB-C18 column (150×2.1 mm, 5 µm, Agilent, USA) with a linear gradient from 30% to 90% eluent B (solution of acetonitrile/isopropanol/water, 90/8/ 2 o/o /o, with adding 0.1% formic acid and 10 mmol/L ammonium formate) for 20 minutes. Solution of acetonitrile/water (60:40, v:v) with adding 0.1% formic acid and 10 mmol/L ammonium formate were used as eluent A. Eluent flow rate was 40 μL/min, injection volume was 3 μL. Mass spectra were obtained in n positive ion mode (m/z in the range of 100-1700 uma) with the following settings : 4.1 kV capillary voltage in positive ion mode spray gas pressure 0.7 bar, drying gas flow rate 6 L/min, drying gas temperature 200°C.
Statistical analysis
Data processing was carried out using software MzMine 3.1 with lipid identification was performed using LIPID MAPS Structure |Database (LMSD). Comparison between the lipid profile by one and two time points using the Wilcoxon test. Comparison of changes in lipid levels after treatment in each group was performed using Mann-Whitney U test. The threshold value for statistical significance was 0.05. Median (Me) and quartiles Q1 and Q3 (Q1; Q3) were used to describe lipid levels, where Me was a median value, Q1 – the value of the first quartile, Q3 – the value of the third quartile. Statistical data processing was performed using R 4.3.1 for Windows (R: A Language and Environment for Statistical Computing) with a set of tools Rstudio (R Studio: Integrated Development for R).
Results
The age of patients included in the study varied from 46 to 65 years and on average was 54.8 (5.1) years. The duration of menopause in patients was from 1 to 18 years and on average was 5.4 (3.3) years. The clinical and anamnestic data of patients is shown in Table 1.
The use of Dynamic Quadripolar Radiofrequency (DQRF) exposure (group 1), the differences in the level of PG 12:0/18:4(6Z,9Z,12Z,15Z) were found in positive ion mode (Table 2).
With combination of DQRF and Ultra-Pulsed Radioporation (UPR) with extragens (group 2), the differences were in the levels of 4 lipids: Anandamide (18:2, n-6), LTB4 dimethylamide, N-hydroxy arachidonylamine, Virodamine) in positive ion mode (Table 4).
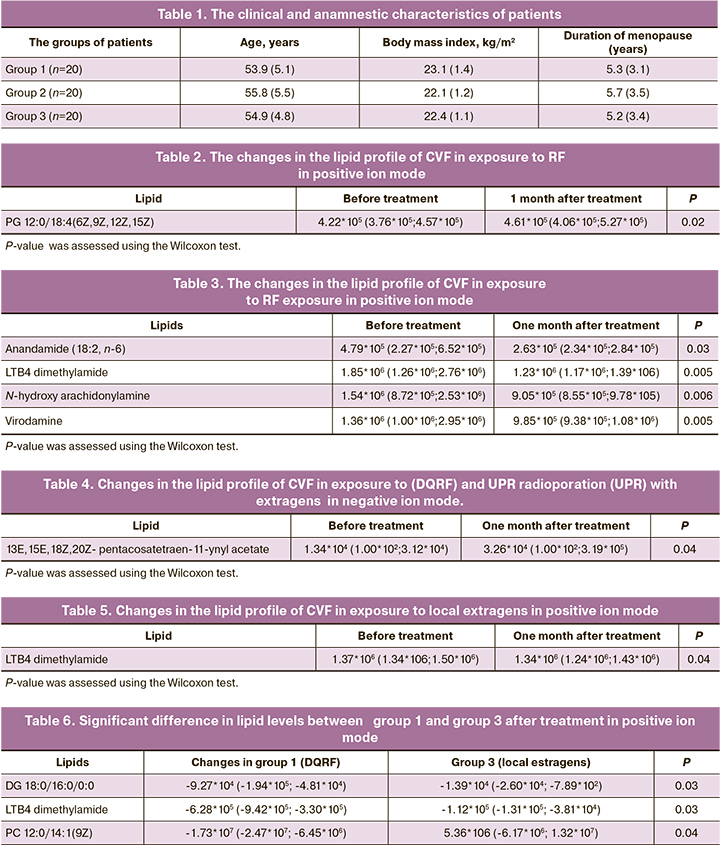
At the same time, in group 3, which was exposed only to extrogens, the differences were in the levels of LTB4 dimethylamide. Also, reduced level of LTB4 dimethylamide was in group 2 (Table 5).
Comparison of treatment results in women in group 1 (DQRF) and group 3 (local estrogens) showed that 3 lipids (DG 18:0/16:0/0:0; LTB4- LTB4 dimethylamid; PC 12:0/14:1(9Z)) were identified in positive ion mode. In group 3, their levels did not change significantly (Table 6). At the same time, the level of PC 12:0/14:1(9Z) changed significantly in group 3 versus group 1.
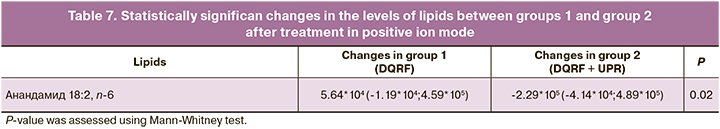
Comparison of treatment results between group 1 and group 2 showed that 1 lipid – Anandamide (18:2, n-6) was identified in positive ion mode (Table 7), the level of which increased after treatment in group 1.
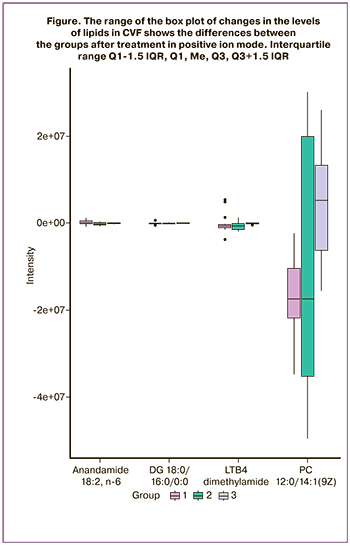
The boxplot (Fig.) shows that the metabolomic profile after treatment in group 1 differed from the profiles in group 2 and group 3.
Duscussion
In this study, the differences in the lipid composition of cervicocaginal fluid in women with VVA, who underwent DQRF treatment we found and described for the first time.
Anandamide and virodamine in the lipid profile are of special interest. Significantly increased levels of these lipid were found in patients in patient in group 1, who received DQRF treatment as monotherapy. These substances are derivatives of arachidonic acid, endogenous cannabinoid neurotransmitters, biologically active lipids that activate cannabinoid receptors CB1, CB2.
The cannabinoid-1 receptor (CB1) was primarily indentified in 1990 г., then the cannabinoid-2 receptor 2 (CB2) was identified in 1993 г. The first isolated endocannabinoid was ethanolamide of arachidonic acid, also known as anandamide or arachidonoylethanolamine (AEA), (the word formed from the word "ananda", a Sanskrit word meaning "bliss"). Current data show that the cannabinoid receptors are expressed in cells of the reproductive system, including endometrial stromal cells, vaginal epithelium, ovaries, and spermatozoa. [15]. Intracellular signaling from interaction with the cannabinoid CB1 and CB2 receptors subsequently lead to the regulation of cell growth, proliferation and/or tissue differentiation. Thus, we suggest that improvement of vaginal tissue trophism and increased sexual satisfaction in women, who underwent treatment on the background of reduced incidence of VVA symptoms, among other things, are associated with activation of the CB1 and CB2 receptors. Interesting is the fact that this effect was lower in the groups with the use of local estrogens (estriol).
With the development of evidence-based medicine, it has become clear that the efficacy and safety of systemic hormonal therapy for VVA /GSM is overestimated. First of all, such therapy is not indicated for a number of categories of patients, for example, the patients with hormone-dependent cancer of the reproductive system and breast cancer (including in anamnesis), with normal estrogen levels at high risk of thrombosis, acute or chronic liver failure, myocardial infarction in history and other conditions [16].
Conclusion
The therapy for GSM/VVA by exposure of DQRF is an effective and safe treatment option for women, when hormone therapy cannot be used for one reason or another. Currently, the study is ongoing to assess the safety and duration of the achieved clinical effect.
References
- Тихомирова Е.В., Балан В.Е., Фомина-Нилова О.С. Методы лечения генитоуринарного синдрома на современном этапе. Медицинский совет. 2020; 13: 91-6. https://dx.doi.org/10.21518/2079-701x-2020-13-91-96. [Tikhomirova E.V., Balan V.E., Fomina-Nilova O.S. Current treatment options for genitourinary syndrome. Medical Council. 2020;(13):91-96. (in Russian)]. https://dx.doi.org/10.21518/2079-701x-2020-13-91-96.
- Bachmann G., Cheng R.J., Rovner E. Vulvovaginal complaints. In: Lobo R.A., ed. Treatment of the postmenopausal woman: basic and clinical aspects. 3rd ed. Burlington, MA: Academic Press; 2007: 263-70.
- Palma F., Volpe A., Villa P., Cagnacci A.; Writing group of AGATA study. Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: The AGATA study. Maturitas. 2016; 83: 40-4.https://dx.doi.org/10.1016/j.maturitas.2015.09.001.
- Palacios S., Henderson V.W., Siseles N., Tan D., Villaseca P. Age of menopause and impact of climacteric symptoms by geographical region. Climacteric. 2010; 13(5): 419-28. https://dx.doi.org/10.3109/13697137.2010.507886.
- The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause. 2020; 27(9): 976-92.https://dx.doi.org/10.1097/GME.0000000000001609.
- Vicariotto F., Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016; 68(3): 225-36.
- Vicariotto F., De Seta F., Faoro V., Raichi M. Dynamic quadripolar radiofrequency treatment of vaginal laxity/menopausal vulvo-vaginal atrophy: 12-month efficacy and safety. Minerva Ginecol. 2017;69(4): 342-9.
- Sadick N.S., Malerich S.A., Nassar A.H., Dorizas A.S. Radiofrequency: an update on latest innovations. J. Drugs Dermatol. 2014; 13(11): 1331-5.
- Sekiguchi Y., Utsugisawa Y., Azekosi Y., Kinjo M., Song M., Kubota Y. et al. Laxity of the vaginal introitus after childbirth: nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfaction using low-energy radiofrequency thermal therapy. J. Womens Health (Larchmt) 2013; 22(9): 775-81. https://dx.doi.org/10.1089/jwh.2012.4123.
- Казакова С.Н., Аполихина И.А., Тетерина Т.А., Паузина О.А. Применение терапевтического радиочастотного воздействия в гинекологии. Акушерство и гинекология. 2020; 9: 192-8. https://dx.doi.org/10.18565/aig.2020.9.192-198. [Kazakova S.N., Apolikhina I.A., Teterina T.A., Pauzina O.A. Use of therapeutic radiofrequency exposure in gynecology. Obstetrics and Gynecology. 2020; 9: 192-8. (in Russian)].https://dx.doi.org/10.18565/aig.2020.9.192-198.
- Dillon B., Dmochowski R. Radiofrequency for the treatment of stress urinary incontinence in women. Curr. Urol. Rep. 2009; 10(5): 369-74.https://dx.doi.org/10.1007/s11934-009-0058-z.
- Leibaschoff G., Izasa P.G., Cardona J.L., Miklos J.R., Moore R.D. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg. Technol. Int. 2016; 29: 149-59.
- Sarmento A.C., Fernandes F.S., Marconi C., Giraldo P.C., Eleutério-Júnior J., Crispim J.C., Gonçalves A.K. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020; 75: e1750. https://dx.doi.org/10.6061/clinics/2020/e1750.
- Tranchini R., Raichi M. Ultra-pulsed radioporation further enhances the efficacy of dynamic Quadripolar RadioFrequency in women with post-menopausal vulvo-vaginal atrophy. Clin. Obstet. Gynecol. Reprod. Med. 2018; 4(3): 1-5. https://dx.doi.org/10.15761/COGRM.1000221.
- Walker O.S., Holloway A.C., Raha S. The role of the endocannabinoid system in female reproductive tissues. J. Ovarian Res. 2019; 12(1): 3.https://dx.doi.org/10.1186/s13048-018-0478-9.
- Paszkowski T., Bińkowska M., Dębski R., Krzyczkowska-Sendrakowska M., Skrzypulec-Plinta V., Zgliczyński W. Menopausal hormone therapy in questions and answers - a manual for physicians of various specialties. Prz Menopauzalny. 2019; 18(1): 1-8. https://dx.doi.org/10.5114/pm.2019.84150.
Received 22.10.2022
Accepted 05.12.2022
About the Authors
Svetlana N. Kazakova, postgraduate student at the Department of Obstetrics, Gynecology, Perinatology and Reproductology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, s-juice@mail.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.Inna A. Apolikhina, Dr. Med. Sci., Professor, Head of the Department of Aesthetic Gynecology and Rehabilitation, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia; Professor at the Department of Obstetrics, Gynecology, Perinatology and Reproductology, Institute of Professional Education, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University), i_apolikhina@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Vitaliy V. Chagovets, PhD, Head of the Laboratory of Metabolomics and Bioinformatics, Department of Systems Biology in Reproductive Medicine of the Institute of Translational Medicine, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, v_chagovets@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Vladimir E. Frankevich, Dr. Sci. (Physics and Mathematics), Deputy Director for Research – Head of the Department of Systems Biology in Reproduction, Institute
of Translational Medicine, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, v_frankevich@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Tatiana A. Teterina, PhD, Obstetrician-gynecologist, Department of Aesthetic Gynecology and Rehabilitation, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, t_teterina@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Alisa O. Tokareva, specialist at the Laboratory of Clinical Proteomics, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, alisa.tokareva@phystech.edu, 117997, Russia, Moscow, Ac. Oparina str., 4
Authors’ contributions: Kazakova S.N., Apolikhina I.A. – the concept and design of the study; Kazakova S.N., Teterina T.A., Tokareva O.A. – material collection and processing, writing the article; Frankevich V.E., Chagovets V.V., Tokareva A.O. – performance of laboratory tests, statistical analysis; Apolikhina I.A. – article editing.
Conflicts of interest: The authors declare that they have no conflict of interests.
Funding: The study was carried out without any sponsorship.
Ethical Approval: The study was approved by the decision of the Commission on the Ethics of Biomedical Researches of V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia.
Patients’ Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citing: Kazakova S.N., Apolokhina I.A., Chagovets V.V., Frankevich V.E., Teterina T.A., Tokareva A.O. Lypidome analysis of cervicovaginal fluid (CVF) in patients with vulvovaginal atrophy under exposure to dynamic quadripolar radiofrequency.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 12: 132-138 (in Russian)
https://dx.doi.org/10.18565/aig.2022.251