Laparoscopic ovarian cystectomy in newborns
Objective: To perform a comparative analysis of treatment of newborn girls with complex and simple ovarian cysts.Mokrushina O.G., Chundokova M.A., Shumikhin V.S., Levitskaya M.V., Erokhina N.O., Nagornaya Yu.V., Smirnova S.V., Khalafov R.V.
Materials and methods: A retrospective analysis of treatment of 93 newborn girls with complex ovarian cysts and 32 newborn girls with simple ovarian cysts was performed within 13 years (2009–2021). The diagnosis was based on the results of diagnostic ultrasound examinations in the antenatal and postnatal periods. Analysis of cyst content and size was performed using ultrasound. Preoperative, intraoperative and postoperative evaluation was performed.
Results: Emergency laparoscopic surgery was performed in newborns with simple ovarian cysts about 10 cm in diameter in 37% of cases of all simple ovarian cysts, and in 9% of cases of complex ovarian cysts due to the symptoms of intestinal obstruction. The age of newborns in both groups was 6 days (p=0.880). Elective surgeries was performed at the age of 42 days in the group with complex cysts and 48 The operative time was 30 minutes (p=0.164).Adhesions were found more frequently in the group with complex cysts (p=0.049 in emergency surgeries; р=0.153 in elective surgeries). Ovariocystectomy was performed in all cases of complex cysts. In patients with simple cysts, ovarian tissue was preserved. In both groups, smooth postoperative period lasted 2 days (p=0.072).
Conclusion: Laparoscopy is a reliable and safe technique for treatment of ovarian cysts in newborns. However, it is necessary to define the best way to prevent torsion of ovarian cyst in utero. Puncture of fetal ovarian cyst can be one of the techniques.
Keywords
Antenatal screening of congenital malformations helps to detect developmental anomalies at any term of pregnancy. At the same time, various pathological conditions may manifest themselves even at the end of pregnancy. These diseases include ovarian cysts. Although pathophysiology of ovarian cysts is not fully understood, they can be usually defined as a benign functional anomaly resulting from excessive stimulation of fetal ovaries by placental and maternal hormones. Treatment of congenital ovarian cysts is controversial. It depends on the size of a cyst and complications that may occur during pregnancy or after childbirth [1]. The optimal terms for treatment of congenital ovarian cysts are not defined, and evolution of this anomaly is variable. Although spontaneous regression of most cysts may happen during pregnancy or after childbirth, torsion and hemorrhage may occur antenatally. This increases the risk of surgical intervention and loss of ovaries after birth [2]. The cysts less than 4 cm in size are less likely to be complicated by torsion, the current common recommendation is to monitor small cysts with serial ultrasound examinations until they involute [3]. Since the presented series studies are limited, any report on a large number of studied patients gives a possibility to get acknowledged with the patterns of treatment of newborns with this pathology.
Since 2009, N.F. Filatov Children’s City Clinical Hospital provides prenatal diagnosis. This makes it possible to detect ovarian cysts antenatally.
The purpose of our study was to perform a comparative analysis of treatment of newborn girls with complex and simple ovarian cysts.
Materials and methods
In 2009–2021, a total of 138 newborns were admitted to hospital. The patients, who had cystic masses 35 mm in diameter and even larger in the third trimester, as well as the patients with cystic ovarian mass greater than 40 mm, which was found after birth. 13 patients were excluded from the study due spontaneous regression of cystic masses at the time of birth or during the first month of life.
Thus, the study included 125 girls with ovarian cysts, who underwent surgery. Two groups were formed for comparative analysis. Antenatal torsion of ovarian cyst was a criterion to split the patients into groups. Nussbaum's ultrasound criteria for cysts classification were used, which helped to determine management strategy and indications for surgical treatment of ovarian cysts in newborns. According to this classification, ultrasound features of ovarian cysts classify them into simple cysts (completely anechoic), or not harmful, and complex cysts (the presence of fluid, wall thickening, sludge-like substance). Unfortunately, it is difficult to predict cystic morphology in performing antenatal or postnatal ultrasound examination. For this reason, the Nussbaum classification is convenient for practicing pediatric surgeons.
Group I (complex cysts) consisted of 93 patients. Cyst torsion in uterus with necrosis of ovarian tissue on the damaged side was found intraoperatively in these patients. Group 2 (simple cysts) consisted of 32 patients. Ovarian cyst torsion was not found intraoperatively in this group of patients.
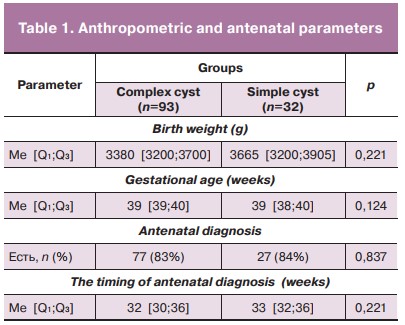
In our case series study, cystic masses were found antenatally in vast majority of cases in both groups. The timing for detection of cystic changes in fetal ovaries in both groups was comparable and conformed with the third ultrasound screening. At the same time, there was no statistical difference between the timing of diagnosis of complex and simple cysts (table 1).
Monitoring of ovarian cyst status was carried out using ultrasound data. US examination was performed on days 1–2 after birth. Cyst size and content were assessed. A round, thin-walled cyst with anechoic content was categorized as a simple cyst. A heterogeneous hyperechoic cystic content or sludge-like substance in cyst lumen was visualized in cases of a complex cyst. This status of ovarian cyst was assessed as intrauterine torsion.
In our series studies the following parameters were assessed: cyst size, the affected side of the ovary, the age of patients, who underwent surgical intervention and clinical manifestations in the abdominal cavity before surgery; intraoperative changes – adhesions, apoplexy, changes in other organs, duration of surgery; the course of postoperative period and the number of days of hospital stay.
Statistical analysis
Statistical analysis was performed using statistical software StatTech v. 2.1.0. The Kolmogorov–Smirnov test was used to compare the quantitative parameters with normal distribution. The quantitative parameters, which had normal distribution, were described using arithmetic mean values (M) and standard deviation (SD), 95% confidence interval (95% CI), and in the absence of normal distribution using median (Me) and lower and upper quartiles (Q1–Q3). The categorical data were presented by absolute values and proportion. The quantitative parameters with normal distribution were compared in two groups using Student’s t-test. Comparison of proportions for the four-field contingency tables was performed using Fisher's exact test, and Pearson's chi-square (χ2) test was used for multi-way contingency tables.
Results
Most of cystic formations had no clinical manifestations in the abdominal cavity. For this reason, ultrasound was a major diagnostic technique for this pathology. In the absence of any symptoms in the organs of the abdominal cavity, the child was discharged from maternity hospital with the subsequent appointment to see a pediatrician in the consultative and diagnostic center at our hospital. The age of newborns for the first examination in the outpatient setting was 14–18 days. The major criteria for selection of patients for elective inpatient admission were the size of cystic formation greater than 40 mm and intrauterine torsion manifested in US. In the absence of complications of the cyst, ambulatory monitoring was continued during the first month of life. Thus, in our study, there were 2 causes for hospitalization: urgent hospital admission in cases of clinical manifestation of intestinal obstruction and elective hospital admission in asymptomatic cases.
Regardless from where the newborn girls were admitted to hospital, they underwent a control ultrasound examination of the abdominal cavity on the 1st day of hospitalization to verify the location of cystic lesion, measure the cyst size and detect the signs of intrauterine torsion.
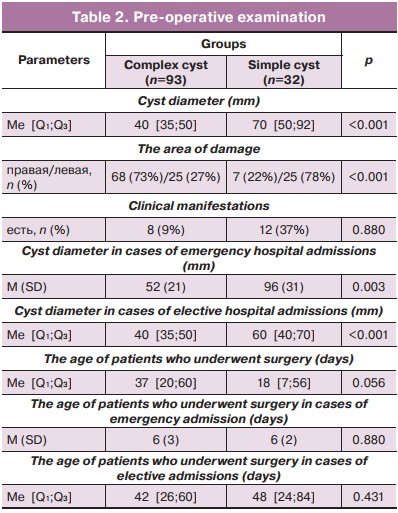
In our case series study, complex ovarian cysts were on average 2 times larger in size than in the group with torsion of ovarian cysts and most often related to the left ovary. A large diameter of the cystic mass was often a cause for partial intestinal obstruction. This was the reason for early transfer of the child from maternity hospital. The predominant localization of a complex cyst on the right side was apparently associated with a free space in the right iliac region versus the left one, where the sigmoid colon is located limiting the mobility of the cystic formation of the left ovary.
20/125 (16%) patients were admitted to hospital on the first week of life due to clinical manifestations of partial intestinal obstruction. The characteristic symptoms of functional bowel disorders were abdominal pain, food intolerance and bloating. The girls with simple cysts were admitted to hospital for urgent indications 4 times more often due to the size of the cystic mass. The simple cysts for emergency admissions were about 10 cm in diameter, while the complex cysts were about 5 cm in diameter. The difference between the groups was statistically significant (p=0.003).
Elective admissions included the remaining 105 patients. Ultrasound examination showed increasing cyst size in the group with simple cysts 1.5 times more compared to the group with complex cysts.
Indications for surgical treatment of a simple cyst was a large diameter with the signs of partial intestinal obstruction and absent regression in dynamic monitoring. In these cases, cystectomy was performed with ovarian tissue preservation. The patients with diagnosis of intrauterine torsion underwent ovarian cystectomy due to necrotic fetal cyst and ovarian tissue in the area of damage. In this study, the results of analysis showed that in the group with complex cysts, the mean age of patients who underwent surgical intervention was 37 days versus 19 days in the group with simple cysts. However, the difference was not statistically significant (p=0.056). Also, no statistically significance difference was between the groups in the age of patients who underwent surgery according to the type of hospital admissions. In both groups, the mean age in cases of emergency admissions was 6 days (p=0.880). In cases of elective admissions, the mean age in the group with complex cysts was 42 days versus 48 in the group with simple cysts (p=0.431) (Table 2).
Laparoscopic surgery was performed in all cases. The patients were placed in the supine position on the operating table. The surgeon stood on the right or left of the patient (depending on lesion location), and the assistant stood on the opposite side. The monitor was placed at the patient's feet. The anesthesiologist was at the head end of the table. Two or three optical trocars (4.7 mm in diameter), surgical instruments (3 mm in diameter) were used to perform surgery. Carbon dioxide (СО2) was maintained at 8–10 mm, СО2 flow rate was 2–3 l/min. Trocars were placed in the following way: infraumbilical incision was performed to insert endoscope; the instruments were inserted along the right and/or left midclavicular line 1.0 cm above the umbilical region. The initial procedure of surgical intervention was evaluation of topography of the organs. Then pelvic organs were examined visualizing uterus, fallopian tubes, ovaries and cystic formations. Further surgical tactics depended on the type of cyst.
Two trocars were often used in case of a complex cyst. At the same time, after visualization of cystic changes and absence of abdominal adhesion, the optical trocar was moved to the working trocar, and a clamp was inserted through the infraumbilical trocar to capture the cyst wall. The next maneuver was to move the captured cyst to the extended infraumbilical access, and a part of the cyst eviscerated. Then puncture from the outside was performed, and cyst content was aspirated. After that, the cyst wall was removed through the same incision. When adhesions were detected in complex cysts, the third trocar was inserted, the adhesions were divided, the cysts were separated, and subsequently removed from the abdominal cavity through the infraumbilical extended incision, and the content was aspirated. Also, in case of auto-amputated ovary, the presence or absence of fallopian tube atresia in the form of a strand was commonly discovered on the side of torsion due to impaired uterine arterial blood flow and presented either in the form of a strand.
In cases of diagnosed simple cyst of a large size, initially the intra-abdominal puncture and evacuation of the cyst content were performed. The internal organs were examined. Also, in cases of a large diameter of cysts, the extra-abdominal cyst wall resection and removal through the extended infraumbilical incision were performed. In cases when the cyst diameter was about 5 cm, the puncture of cyst and aspiration of its content were performed. Then after cyst cavity opening intra-abdominal removal of the cyst wall was performed with preservation of ovarian tissue.
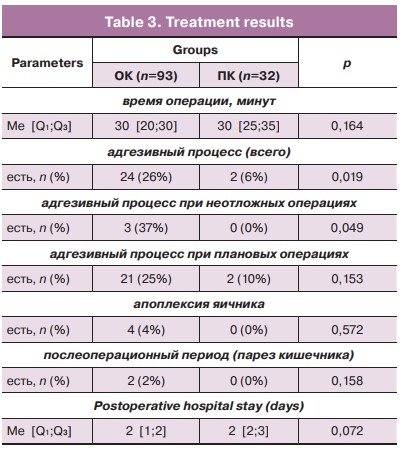
The analysis of surgical interventions showed that in our series study no cases of conversion occurred. Surgery lasted approximately 0.5 hour (р=0.164), and there was no significant difference between the groups in the operative time. Adhesions in the abdominal cavity occurred 4 times more often in the group with complex cysts and reached 26% versus 6% вin the group with simple cysts. In 3 of 8 cases, adhesions in the group of patients with complex cysts were an indication for emergency surgery due to the symptoms of intestinal obstruction. Since complex cysts were predominantly located in the right iliac region, the appendage was often involved in the pathological process in addition to small bowel loops and the omentum. In one case after division of adhesions, the changes in the appendage were irreversible and required appendectomy. Our observations showed that adhesions retain in asymptomatic cysts and can potentially cause an acute process in the abdominal cavity. So, in elective surgeries, adhesive process in the group with complex cysts was observed 2.5 more often versus the group of simple cysts. Although, there was no statistically significant difference in this parameters between the groups (р=0.153). Another type intraoperative complication was cyst wall rupture and outflow of the cyst contents into the abdominal cavity. In our series study, this occurred in 4 cases (4%). All cases of cyst apoplexy occurred in the group with complex cysts. The difference between the values was not statistically significant (р=0.153).
The postoperative period was smooth in both groups. Enteral loading was started three hours after the child was transferred to the department with subsequent gradual increase in feeding volume, which was age-appropriate and adequate to daily intake. Аntibiotic therapy was carried out within one postoperative day. When postoperative course was favorable, the patients were discharged from hospital. In our series study, gastroparesis persisted for two postoperative days only in 2 patients with complex cysts. Both patients were admitted to hospital with the symptoms of intestinal obstruction on the background of intrauterine adhesions. Spontaneous resolution of gastroparesis was in both cases. Enteral loading was started 3 days after surgery. A day later, the children were discharged home. Complication rate in the postoperative period was 2% in the group with cyst torsion versus 0% in the group with simple cysts. These values were no statistically significant (р=0.158). In general, the duration of postoperative hospital stay in both groups was 2 days, and the difference was not statistically significant (р=0.072).
After hospital discharge, all patients had ambulatory follow-up by pediatric surgeon, pediatric and adolescent obstetrician-gynecologist in the consultative and diagnostic center in N.F. Filatov Children’s City Hospital. In our case series study, there were no cases of cyst recurrence or intestinal obstruction in the postoperative period. The results are shown in Table 3.
Discussion
Ovarian cysts are the most common cystic anomalies of the abdominal cavity, which are diagnosed prenatally.Fetal ovarian cysts occur as a response of the fetal ovaries to maternal and placental estrogens and gonadotropins. Prenatal diagnosis and postnatal treatment of fetal ovarian cysts is a complex task [4]. The size and appearance of the cyst are the major factors that determine perinatal outcome, and are associated with increased risk of ovarian torsion, intracystic hemorrhage and the need to perform ovariectomy [2, 5]. Although the size of the cyst, which increases the risk of torsion or frequency of surgical interventions is not clearly defined, some data showed increased need for surgery. Torsion or inability for spontaneous regression is typical for the cyst size 40 mm and larger. [5]. In this study, we performed surgical intervention only in cases, when the cyst sizes were larger than 40 mm. In our case series study, 84% of girls had no clinical manifestation of cysts in the neonatal period. The similar situation is described in girls at later age. The question of the variety of clinical course of ovarian formations in girls and adolescents remains debatable, and timely diagnosis presents significant difficulties even at later age [6]. However, in some cases, the presence of adhesive process may be the cause of intestinal obstruction. The cause of adhesions can be torsion of the cyst with necrosis of the cyst wall, ovarian tissue and sterile inflammation around affected organ. In our case series studies, 16% of patients had the signs of intestinal obstruction. Other authors reported a higher rate of complications in the cause of the disease. So, in one of the studies, the symptoms of complex cysts were detected in 28% of patients [2]. It was described that pulmonary hypoplasia or polyhydramnios develop with giant cysts as a result of compression of the small intestine, which prevents the mechanism of fetal swallowing [1]. It should be noted, that we could not find publications, which describe laparotomy – the open access technique for cyst excision. Our study showed that laparoscopy in newborns is a safe and reliable surgical technique. In all cases of complex cysts, ovarian cystectomy was performed due to ovarian tissue necrosis, and in cases of simple cyst, organ-sparing surgery – cystectomy is performed [2, 3, 5]. Ovary removal is inevitable in occurrence of torsion of fetal ovarian cyst in utero or postnatally. To date, there are a limited number of procedures that could prevent this complication. One of the methods that influence the development of complications is a fetal cyst puncture. Some authors reported that cyst puncture was not associated with neither reduced number of neonatal interventions or increased incidence of preterm births. However, this was associated with a reduced rate of ovariectomy [2, 7]. One of the studies showed encouraging results in using prenatal aspiration and significant reduction in the risk of torsion. The risk reduced in 85% of cyst torsions (cyst size 50 mm or larger) without aspiration, and up to 14% with aspiration [5]. Another method of simple ovarian cysts treatment is postnatal percutaneous puncture. However, these manipulations are rare in frequency, and only single cases have been described. For this reason, the level of evidence is not high [5].
Conclusion
Therefore, we suggest that multidisciplinary approach to antenatal consultation and development of protocol for antenatal management of pregnant women with fetal ovarian cysts, can be a good premise for reduction in the frequency of complications of the studied pathology. In the postnatal period, ultrasound examination of abdominal organs in newborn girls and surgeon's consultation should be mandatory with purpose of individual approach to treatment of ovarian cyst formations.
References
-
Wróblewska-Seniuk K., Jarząbek-Bielecka G., Kędzia W. Gynecological problems in newborns and infants. J. Clin. Med. 2021; 10(5): 1071.
https://dx.doi.org/10.3390/jcm10051071.
- Bascietto F., Liberati M., Marrone L., KhalilA., Pagani G., Gustapane S. et al. Outcome of fetal ovarian cysts diagnosed on prenatal ultrasound examination: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2017; 50(1): 20-31. https://dx.doi.org/10.1002/uog.16002.
- Rialon K.L., Akinkuotu A., Fahy A.S., Shelmerdine S., Traubici J., Priscilla Ch. Management of ovarian lesions diagnosed during infancy. Pediatr. Surg. 2019; 54: 955-8. https://dx.doi.org/10.1016/j.jpedsurg.2019.01.027.
- Ivanitskaya O.N., Odegova N.O., Andreeva E.N. Ovarian cysts in fetuses – features of prenatal diagnosis and postnatal outcome. Russian Bulletin of Obstetrician-Gynecologist. 2020; 20(1): 73-80. (in Russian). https://dx.doi.org/10.17116/rosakush20202001173.
- Tyraskis A., Bakalis S., Scala C. et al. A retrospective multicenter study of the natural history of fetal ovarian cysts. Pediatr. Surg. 2018; 53(10): 2019-22. https://dx.doi.org/10.1016/j.jpedsurg.2018.02.049.
- Adamyan L.V., Koltunov I.E., Sibirskaya E.V., Sharkov S.M., Korotkova S.A., Moksyakova E.G., Movsesyan E.Kh. Features of the differential diagnosis of ovarian tumors in girls (observation from the practice). Detskaya Khirurgya (Russian Journal of Pediatric Surgery). 2018; 22(3): 160-2. (in Russian). https://dx.doi.org/10.18821/1560-9510-2018-22-3-160-162.
- Diguisto C., N Winer N., Benoist G., Laurichesse-Delmas H., Potin , Binet A. et al. In-utero aspiration vs expectant management of anechoic fetal ovarian cysts: open randomized controlled trial. Ultrasound Obstet. Gynecol. 2018; 52(2): 159-64. https://dx.doi.org/10.1002/uog.18973.
Received 03.06.2022
Accepted 07.09.2022
About the Authors
Olga G. Mokrushina, Dr. Med. Sci., Vice Medical Director, N.F. Filatov Children’s City Hospital of Moscow Health Department; Professor at Pediatric Surgery Department, Pirogov Russian National Research Medical University, +7(916)523-11-38, mokrushina@yandex.ru, https://orcid.org/0000-0003-4444-6103, 103001, Russia, Moscow,Sadovaya-Kudrinskaya str., 15.
Madina A. Chundokova, pediatric surgeon at the Abdominal Department, N.F. Filatov Children’s City Hospital of Moscow Health Department; Professor at the Pediatric Surgery Department, Pirogov Russian National Research Medical University, https://orcid.org/0000-0002-5080-4838, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Vasily S. Shumikhin, Head of the Department of Neonatal Surgery, N.F. Filatov Children’s City Hospital of Moscow Health Department; Associate Professor at the Pediatric Surgery Department, Pirogov Russian National Research Medical University, https://orcid.org/0000-0001-9477-8785, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Marina V. Levitskaya, PhD, pediatric surgeon at the Neonatal Department, N.F. Filatov Children’s City Hospital of Moscow Health Department,
https://orcid.org/0000-0002-9838-9493, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Nadezhda O. Erokhina, pediatric surgeon at the Neonatal Department, N.F. Filatov Children’s City Hospital of Moscow Health Department,
https://orcid.org/0000-0003-05-19-7220, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Yulia V. Nagornaya, pediatric surgeon at the Neonatal Department, N.F. Filatov Children’s City Hospital of Moscow Health Department; Teaching assistant at the Pediatric Surgery Department, Pirogov Russian National Research Medical University, https://orcid.org/0000-0002-1702-7811, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Svetlana V. Smirnova, pediatric surgeon at the Neonatal Department, N.F. Filatov Children’s City Hospital of Moscow Health Department; Teaching assistant at the Pediatric Surgery Department, Pirogov Russian National Research Medical University, https://orcid.org/0000-0001-9158-4571, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Rashid V. Khalafov, pediatric surgeon at the Neonatal Department, N.F. Filatov Children’s City Hospital of Moscow Health Department; Teaching assistant at the Pediatric Surgery Department, Pirogov Russian National Research Medical University, https://orcid.org/0000-0001-7998-5639, 103001, Russia, Moscow, Sadovaya-Kudrinskaya str., 15.
Corresponding author: Olga G. Mokrushina, +7(916)523-11-39, mokrushina@yandex.ru
Authors’ contributions: Mokrushina O.G., Levitskaya M.V. – the concept and design of the study; Shumikhin V.S.,
Nagornaya Yu.V., Erokhina N.O. – material collection and processing; Smirnova S.V., Khalafov R.V. – statistical data processing; Mokrushina O.G. – article writing; Chundokova M.A. – article editing.
Conflicts of interest: The authors declare that they have no conflicts of interest regarding this publication.
Funding: No external financial support has been provided for this work.
Ethical Approval: The study was approved by the local Ethics Committee of N.F. Filatov Children’s City Clinical Hospital of Moscow Healthcare Department.
Patient Consent for Publication: The mothers of newborns provided informed consent for the publication of the data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Mokrushina O.G., Chundokova M.A., Shumikhin V.S., Levitskaya M.V., Erokhina N.O., Nagornaya Yu.V., Smirnova S.V., Khalafov R.V.
Laparoscopic ovarian cystectomy in newborns.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 9: 129-134 (in Russian)
https://dx.doi.org/10.18565/aig.2022.9.129-134