Umbilical cord arterial lactate levels in newborns with and without acidosis
Aim. To investigate the role of measuring umbilical cord arterial lactate level in the diagnosis of hypoxia and prediction of neonatal complications.Prikhod'ko A.M., Romanov A.Yu., Baev O.R.
Materials and methods. A prospective study comprised 250 newborns, who were tested at birth for the acid-base balance (ABB) of arterial blood obtained from the umbilical cord. Of them, 202 (80.8%) had normal ABB and formed group 1; 48 (19.2%) patients with metabolic acidosis were enrolled in group 2.
Results. Umbilical cord arterial lactate levels were 5.4 (3.9 - 7.3) and 11.5 (8.5 - 14.0) mmol/L in groups 1 and 2, respectively, p=0.0001. At lactate levels above 8.5 mmol/L, the OR for metabolic acidosis was 34.6 (95% CI=13.6–87.8). Thirty-four (16.8%) newborns without metabolic acidosis had lactate levels above 8.5 mmol/
L. Of them, 24 (70.9%) experienced morbidities in the early neonatal period (low Apgar score, encephalopathy, infections, meconium aspiration, and DIC).
Conclusion. An increased concentration of lactate in arterial umbilical cord blood in newborns with low pH values, combined with a severe base deficit, an increase in pCO2, and a decrease in pO2 reflects the presence of metabolic acidosis. At the same time, an increased umbilical cord arterial lactate level in newborns without other signs of metabolic acidosis is suggestive of increased risk of complications in the early neonatal period.
Keywords
In recent years, there has been an increasing interest in markers of hypoxic brain injury in newborns [1]. Current literature provides evidence for a relationship between umbilical cord blood lactate, pH, and base deficit, as well as the causes for its increase, one of which may be fetal hypoxia in childbirth [2–6]. According to a systematic review by Allanson E.R. et al. (2017), umbilical cord blood lactate levels correlated with pH, base deficit, and Apgar scores at 5 minutes. The authors also reported that umbilical lactate had sensitivity and specificity for predicting neonatal neurological outcomes including hypoxic-ischemic encephalopathy of 69.7% (95% CI 23.8–94.4%) and 93% (95% CI 86.8–96.3%). According to Einikyte R. et al. (2017), umbilical cord arterial lactate and pH predicted early neonatal complications with similar accuracy [6].
However, the association between lactate levels and the development of acidosis remains poorly understood. Also, the influence of other factors on the level of its content cannot be ruled out. For example, a study by Zanardo V. et al. (2015) showed that cord arterial lactate levels and glucose concentration, reflecting the processes of fetal gluconeogenesis, were significantly and positively correlated. Also, glucose concentration was negatively correlated with pH and partial pressure of carbon dioxide (pCO2). The significance of increased lactate levels in the differentiating transitional and pathological conditions in the neonatal life and predicting its course remains unclear.
Based on the preceding, this study aimed to investigate the role of measuring umbilical cord arterial lactate level in the diagnosis of hypoxia and prediction of neonatal complications.
Materials and methods
A prospective study was conducted at the maternity ward of V.I. Kulakov NMRC for OG&P of Minzdrav of Russia in 2016-2018. The study comprised 250 full-term newborns. Immediately after birth, all the newborns included in the study were tested for the acidbase balance (ABB) of arterial blood obtained from the umbilical cord. Blood samples were taken by isolating the umbilical cord segment with three clamps. The cord was then cut between the 1st and 2nd clamps, and blood was drawn from the umbilical artery between the 2nd and 3rd clamps. The pH, lac, B.E., oxygen partial pressure (pO2) and pCO2 levels were measured using an ABL800 FLEX blood gas analyzer (Radiometer Medical ApS, Denmark). Group 1included 202 (80.8%) newborns without signs of metabolic acidosis (pH ≥ 7.12; BE ≥ 12.4 mmol/L); group 2 included 48 (19.2%) newborns with metabolic acidosis (pH <7.12 and / or BE <12.4 mmol/L). Thresholds for creating groups with and without metabolic acidosis were selected based on a previous study [7]. The study was approved by the ethics committee of the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 6 (GraphPad Software, USA). The distribution of continuous variables was tested for normality using the generalized D’Agostino-Pearson test. Quantitative variables showing normal distribution were expressed as means (standard deviation); t-test was used to compare them. Data with non-normal distribution were reported as the median (interquartile range). The Mann-Whitney U test was used to examine the significance of medians’ differences. Qualitative variables were summarized as counts and percentages. To assess the relationship between lactate level and the development of metabolic acidosis, an ROC analysis was performed, and the odds ratio was calculated. During the ROC analysis, the area under the ROC curve, the sensitivity, and specificity of the model were calculated. Differences were considered statistically significant at p <0.05.
Results
Eighty five (42.1%) and 21 (43.7%) neonates in groups 1 and 2, respectively, were born by spontaneous vaginal delivery. In groups 1 and 2, 20.8% (n = 42) and 29.2% (n = 14) women had vacuum-assisted delivery, 37.1% (n = 75) and 27.1% (n = 13) underwent cesarean section. One patient in group 1 and two patients in group 2 required the use of obstetric forceps.
Operative delivery rates did not differ between the study groups (p = 0.13 and p = 0.15 for cesarean section and vacuum extraction, respectively).
Newborns in group 2 had lower first- and fifth-minute Apgar scores. Lactate concentration in arterial umbilical cord blood was higher concurrently with a decrease in pO2, an increase in pCO2, and BE (Table).
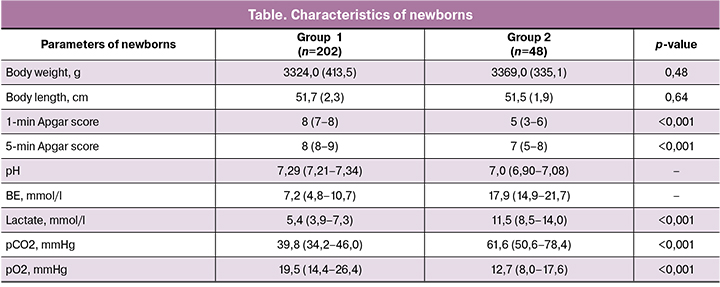
At the next stage of the study, we analyzed the relationship between the pH level and the umbilical cord arterial lactate (Figure). The predictive cut-off threshold for the presence of metabolic acidosis was a concentration of the umbilical cord arterial lactate of 8.5mmol/L. The area under the ROC curve was 90%; the sensitivity and specificity of the model were 88% and 83%, respectively.
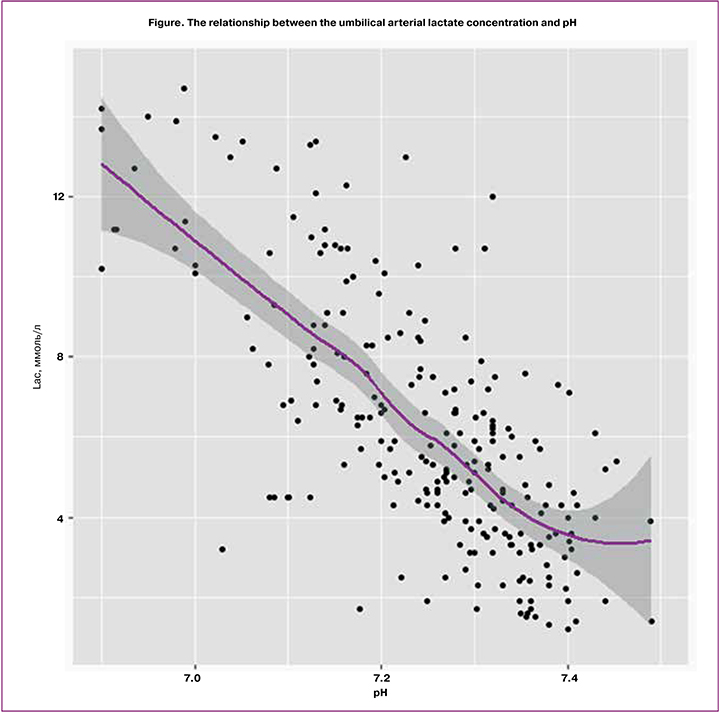
The odds ratio for the development of metabolic acidosis with an umbilical arterial lactate level of more than 8.5 mmol/L was 34.6 (95% CI = 13.6-87.8). It should be noted that in the group of newborns with metabolic acidosis, 6 (12.5%) newborns had normal umbilical arterial lactate levels (<8.5 mmol / L).
However, 34 (16.8%) neonates without metabolic acidosis also had increased umbilical arterial lactate level > 8.5 mmol/L. Of them, 24 (70.6%) had complicated early neonatal period including the Apgar score from 1 to 3 (n = 3; 12.5%), from 4 to 5 (n = 6; 25%). Five (20.8%) newborns subsequently were diagnosed with grade I and II encephalopathy and another five (20.8%) with congenital pneumonia. Two neonates (8.3%) had an infection specific to the perinatal period. Three (12.5%) neonates developed disseminated intravascular coagulation. Three (12.5%) infants had meconium aspiration syndrome. Therefore, despite normal pH values, an elevated umbilical arterial lactate level in 70.6% of cases co-occurred with neonatal complications, not associated with metabolic acidosis at the time of birth.
Discussion
According to the current literature, the mean level of umbilical arterial lactate ranges typically from 2.6 to 4.2 mmol/L, and the threshold for the diagnosis of hypoxia ranges from 3.2 to 7.0 mmol/L [2, 8–10]. These differences are mainly due to the use of different methods for lactate determination. In most studies, the umbilical arterial lactate concentration was measured using portable electrochemical lactometers. In contrast, this study used a more accurate gas analyzer, which is the “gold standard” for measuring the blood gas composition.
In patients with normal basic ABB and those with metabolic acidosis, mean levels of umbilical arterial lactate were 5.4 (3.9–7.3) and 11.5 (8.5–14.0) mmol/l, respectively. ROC analysis showed that the umbilical arterial lactate level of more than 8.5 mmol/L was predictive for perinatal hypoxia at birth with a sensitivity of 88% and a specificity of 83%. In this study, we evaluated the association of umbilical arterial lactate concentration with neonatal outcomes. Most (70.6%) neonates born with normal pH and an increased level of umbilical arterial lactate (>8.5 mmol/L) had early neonatal complications that were not associated with acidosis at birth. These results demonstrate the role of an increased level of umbilical arterial lactate, both in the diagnosis of fetal hypoxia and in predicting other early neonatal complications. At the same time, some newborns (29.4%) who had high umbilical arterial lactate and normal pH did not subsequently show clinical manifestations of any disease. This observation confirms the theory of “birth stress,” which explains the increase in the umbilical arterial lactate concentration in normal childbirth [11, 12].
Conclusion
An increased concentration of lactate in arterial umbilical cord blood in newborns with low pH values co-occurring with a severe base deficit, an increase in pCO2, and a decrease in pO2 reflects the presence of metabolic acidosis of the newborn. At the same time, an increased umbilical cord arterial lactate level in newborns without other signs of metabolic acidosis is suggestive of increased risk of complications in the early neonatal period.
References
- Приходько А.М., Киртбая А.Р., Романов А.Ю., Баев О.Р. Биомаркеры повреждения головного мозга у новорожденных. Неонатология. 2018; 7(1): 70-6. https://dx.doi.org/10.24411/2308-2402-2018-00009. [Prikhodko A.M., Kirtbaya A.R., Romanov A.Yu., Baev O.R. Biomarkers of neonatal brain damage. Neonatologiya (Neonatology) 2018; 7 (1): 70-6. (in Russian)].
- Приходько А.М., Баев О.Р., Евграфова А.В., Романов А.Ю., Дегтярев Д.Н. Показатели кислотно-основного состояния артериальной пуповинной крови при самопроизвольных родах и кесаревом сечении. Акушерство и гинекология. 2019; 2: 83–9. https://dx.doi.org/10.18565/aig.2019.12.83-89. [Prikhodko A.M., Baev O.R., Evgrafova A.V., Romanov A.Yu., Degtyarev D.N. Indicators of umbilical cord arterial blood acid-base status during spontaneous birth and cesarean section. Akusherstvo i Ginekologiya (Obstetrics and Gynecology). 2019 2: 83–9. (in Russian)].
- Allanson E.R., Waqar T., White C., Tunçalp Ö., Dickinson J.E. Umbilical lactate as a measure of acidosis and predictor of neonatal risk: a systematic review. BJOG. 2017; 124(4): 584-94. https://dx.doi.org/10.1111/1471-0528.14306.
- Mazouri A., Fallah R., Saboute M., Taherifard P., Dehghan M. The prognostic value of the level of lactate in umbilical cord blood in predicting complications of neonates with meconium aspiration syndrome. J. Matern. Fetal Neonatal Med . 2019; Jul 24: 1-7. https://dx.doi.org/110.1080/14767058.2019.1623195.
- Palanisamy A., Lopez J., Frolova A., Macones G., Cahill A.G. Association between uterine tachysystole during the last hour of labor and cord blood lactate in parturients at term gestation. Am. J. Perinatol. 2019; 36(11): 1171-8. https://dx.doi.org/110.1055/s-0038-1676492.
- Einikyte R., Snieckuviene V., Ramasauskaite D., Panaviene J., Paliulyte V., Opolskiene G. et al. The comparison of umbilical cord arterial blood lactate and pH values for predicting short-term neonatal outcomes. Taiwan. J. Obstet. Gynecol. 2017; 56(6): 745-9.
- Приходько А.М., Романов А.Ю., Шуклина Д.А., Баев О.Р. Показатели кислотно-основного равновесия и газовый состав артериальной и венозной пуповинной крови в норме и при гипоксии плода. Акушерство и гинекология. 2019; 2: 93-7. https://dx.doi.org/10.18565/aig.2019.2.93-97. [Prikhodko A.M., Romanov A.Yu., Shuklina D.A., Baev O.R. The indicators of acid-base balance and the gas composition of umbilical cord arterial and venous blood in health and fetal hypoxia. Akusherstvo i Ginekologiya (Obstetrics and Gynecology). 2019 2: 93-7 (in Russian)].
- Westgren M., Divon M., Horal M., Ingemarsson I., Kublickas M., Shimojo N., Nordström L. Routine measurements of umbilical artery lactate levels in the prediction of perinatal outcome. Am. J. Obstet. Gynecol. 1995; 173(5): 1416-22. https://dx.doi.org/110.1016/0002-9378(95)90627-4.
- Shirey T., St Pierre J., Winkelman J. Cord lactate, pH, and blood gases from healthy neonates. Gynecol. Obstet. Invest. 1996; 41(1): 15-9. https://dx.doi.org/110.1159/000292027.
- Gjerris A.C., Staer-Jensen J., Jørgensen J.S., Bergholt T., Nickelsen C. Umbilical cord blood lactate: a valuable tool in the assessment of fetal metabolic acidosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008; 139(1): 16-20. https://dx.doi.org/10.1016/j.ejogrb.2007.10.004.
- Nordström L., Achanna S., Naka K., Arulkumaran S. Fetal and maternal lactate increase during active second stage of labour. BJOG. 2001; 108(3): 263-8. https://dx.doi.org/10.1111/j.1471-0528.2001.00034.x.
- Dickson M.J., Zaklama M.S. Fetal and maternal lactate increase during active second stage of labour. BJOG. 2003; 110(1): 85; author reply 85. https://dx.doi.org/10.1046/j.1471-0528.2003.01023_1.x.
Received 26.12.2019
Accepted 07.02.2020
About the Authors
Andrey Yu. Romanov, Ph.D. Student, Specialist at the R&D Department, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia. Tel. +7(903)158-94-00.E-mail: romanov1553@yandex.ru. 4 Oparina str., Moscow, 117997, Russian Federation.
Andrey M. Prikhod’ko, Ph.D., Physician at the 1st Maternity Department, Teaching Assistant at the Department of Obstetrics and Gynecology, Researcher at the Department of Innovative Technologies, Institute of Obstetrics, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia. Tel.: +7(495)438-30-47. E-mail: a_prikhodko@oparina4.ru.
4 Oparina str., Moscow, 117997, Russian Federation.
Oleg R. Baev, Dr.Med.Sci., Professor, Head of the 1st Maternity Department, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia, Professor at the Department of Obstetrics, Gynecology, Perinatology and Reproductology, I.M. Sechenov First MSMU of Minzdrav of Russia (Sechenov University). Tel.: +7(495)438-11-88.
E-mail: o_baev@oparina4.ru. 4 Oparina str., Moscow, 117997, Russian Federation.
For citation: Prikhod’ko A.M., Romanov A.Yu., Baev O.R.
Umbilical cord arterial lactate levels in newborns with and without acidosis.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2020; 5: (In Russian):
https://dx.doi.org/10.18565/aig.2020.5.