Достижения современной науки, расширяя возможности врачей, постоянно улучшают перинатальные показатели. Серьезными темпами снижается перинатальная заболеваемость и смертность. Мы научились выхаживать детей в тех ситуациях, о которых еще двадцать лет назад могли только мечтать. Современные методики реанимации недоношенных, в том числе применение экзогенного сурфактанта, позволили значительно увеличить их выживаемость. Помогает также доказано эффективная методика профилактики респираторного дистресс-синдрома плода глюкокортикоидами. Однако в некоторых областях улучшения показателей не происходит. В первую очередь это касается частоты преждевременных родов. Казалось бы, появился эффективный метод снижения частоты преждевременных родов в группах высокого риска при помощи препаратов прогестерона. Однако широчайшее применение этих средств не снизило популяционную частоту преждевременных родов [1, 2]. Попробуем разобраться, в чем дело. По данным Российского демографического ежегодника [3], в 1990 году частота преждевременных родов составила приблизительно 4,0%, а в 2013 – 4,2%. С учетом того, что с 2012 года Российская Федерация перешла на рекомендованные ВОЗ критерии живорождения, существенного роста не произошло. При этом за тот же период времени существенно изменилась частота многоплодных родов. Это очень важно, ведь многоплодие является важнейшим независимым фактором риска недонашивания беременности [4]. Если в 1990 году доля многоплодных родов составила приблизительно 0,67%, то в 2013 году уже 1,1% (рис. 1).
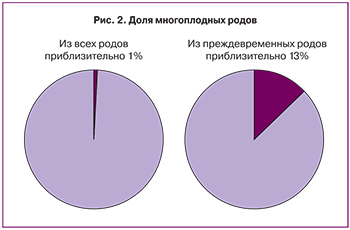
 Попробуем проанализировать эти цифры. Зная, что двойни рождаются преждевременно приблизительно в половине случаев, а многоплодные беременности более высокого порядка заканчиваются раньше срока практически всегда [5] и сопоставив имеющиеся в нашем распоряжении статистические данные, приходим к выводу, что если в 1990 г. из всех преждевременных родов на долю многоплодных приходилось приблизительно 8%, то в 2013 году – уже более 13% это при том, что из всех родов на долю многоплодных приходится лишь 1% (рис. 2). Учитывая, что детей при многоплодных родах рождается больше, доля детей из двоен и троен в общей массе недоношенных составляет приблизительно 23%.
Попробуем проанализировать эти цифры. Зная, что двойни рождаются преждевременно приблизительно в половине случаев, а многоплодные беременности более высокого порядка заканчиваются раньше срока практически всегда [5] и сопоставив имеющиеся в нашем распоряжении статистические данные, приходим к выводу, что если в 1990 г. из всех преждевременных родов на долю многоплодных приходилось приблизительно 8%, то в 2013 году – уже более 13% это при том, что из всех родов на долю многоплодных приходится лишь 1% (рис. 2). Учитывая, что детей при многоплодных родах рождается больше, доля детей из двоен и троен в общей массе недоношенных составляет приблизительно 23%.
Становится понятно, что многоплодные роды играют важнейшую роль в частоте преждевременных родов. Первый вывод, который напрашивается: необходимо снизить частоту многоплодных беременностей. Наиболее очевидный шаг в этом направлении – ограничение количества эмбрионов, переносимых в полость матки в ходе процедуры ЭКО [6]. Переход на перенос одного эмбриона возможен лишь в случае законодательного ограничения. Центры по лечению бесплодия самостоятельно на это вряд ли решатся [7].
Можем ли мы снизить частоту преждевременных родов при уже наступившей многоплодной беременности? Попытаемся рассмотреть основные методики. Не будем в данной статье останавливаться на применении прогестерона. Его эффективность в настоящее время масштабно изучается, и в ближайшее время мы должны получить убедительные данные о его эффективности при многоплодии. Однозначно не снижают частоту преждевременных родов постельный режим и мониторинг маточной активности [8–10].
Проанализируем имеющиеся данные о применении механических методов сохранения беременности.
 По всей видимости, при многоплодии одним из важнейших факторов недонашивания является механическое перерастяжение [11, 12]. Косвенным подтверждением этому являются описанные случаи сохранения беременности после рождения первого плода из многоплодной беременности. То есть устранение фактора перерастяжения в отдельных случаях останавливает даже уже запущенный процесс родов! Фактор избыточной массы в полости матки может вызвать активацию простагландинового каскада или за счет высокого давления способствовать раскрытию шейки матки. Вот в этой ситуации и могут оказаться эффективными швы на шейке матки и пессарии [13].
По всей видимости, при многоплодии одним из важнейших факторов недонашивания является механическое перерастяжение [11, 12]. Косвенным подтверждением этому являются описанные случаи сохранения беременности после рождения первого плода из многоплодной беременности. То есть устранение фактора перерастяжения в отдельных случаях останавливает даже уже запущенный процесс родов! Фактор избыточной массы в полости матки может вызвать активацию простагландинового каскада или за счет высокого давления способствовать раскрытию шейки матки. Вот в этой ситуации и могут оказаться эффективными швы на шейке матки и пессарии [13].
Наиболее точно прогнозировать преждевременные роды и оценить риск недонашивания позволяет измерение длины шейки матки при помощи трансвагинального ультразвукового сканирования. Однократная оценка шейки матки у двоен в сроке 20–24 недели позволяет выделить группу риска. Пороговой отсечкой следует считать 25 мм, как и для одноплодной беременности. При длине шейки матки более 25 мм вероятность родить в срок более 37 недель составляет 65%, а ранних преждевременных родов (до 28 недель) лишь 2% [14]. Fox и соавт. при оценке ассоциации между длиной шейки матки по данным ультразвукового исследования и вероятностью преждевременных родов показали, что наиболее высокую прогностическую ценность имеет ультразвуковое исследование, выполненное в сроке 22–23+6 недель. При этом длина шейки матки в сроке 16–17+6 вообще не коррелирует ни с вероятностью преждевременных родов, ни со сроком гестации на момент родов [15].
Наложение швов на шейку матки
Безусловно, оценка риска преждевременных родов интересует нас не сама по себе, а в качестве инструмента по отбору пациенток высокого риска для проведения дополнительных вмешательств (наложение швов на шейку матки, установка пессария, назначение прогестерона).
В ходе рандомизированого проспективного исследования было проведено сравнение двух групп беременных с двойнями. Основной группе (63 пациентки) ежемесячно, начиная с 16 недель беременности, проводили влагалищное исследование и трансвагинальное ультразвуковое исследование для оценки состояния шейки маки и отбора пациенток для проведения серкляжа. В группе контроля (n=62) проводили только влагалищные исследования в том же режиме, но не измеряли длину шейки матки. Средний срок на момент родов составил 35,7 недель в основной группе (95% доверительный интервал (ДИ) 35,2–36,2), а в контрольной группе – 35,5 недель (95% ДИ 34,7–36,4). При расчете частоты преждевременных родов по кривым Каплана–Мейера достоверных различий между группами также выявлено не было [16].
Однако то, что трансвагинальное ультразвуковое исследование не помогает снизить частоту преждевременных родов при двойне, не означает, что серкляж не будет эффективен в этой группе совсем. Рассмотрим основные результаты крупных исследований на эту тему.
В настоящее время применяется несколько видов серкляжа. В различных центрах используют П-образные или циркулярные швы. В качестве шовного материала используют не рассасывающиеся нити или ленты. Эффективность различных методик серкляжа, по всей видимости, сопоставима. Результаты опубликованных к настоящему времени работ свидетельствуют о том, что тип шовного материала и методики наложения не влияют на эффективность методики [17, 18]. Возможно, ответить на вопрос о наиболее эффективном типе шва поможет многоцентровое сравнительное исследование, протокол которого был опубликован в 2014 году [19].
Обратим внимание на эффективность швов при многоплодной беременности в целом. В 2014 году опубликован Кокрейновский обзор, проведенный с целью оценки эффективности и безопасности серкляжа при многоплодной беременности в следующих случаях:
Швы на шейку матки накладывали всем пациенткам с многоплодной беременностью.
Швы накладывали с учетом анамнестических данных о невынашивании во втором триместре беременности.
Показанием к наложению швов было укорочение шейки матки по данным трансвагинального ультразвукового исследования.
Показания к наложению швов определяли по результатам влагалищного исследования.
Первичными конечными точками анализа были: перинатальная смертность и серьезная неонатальная заболеваемость. В анализ были включены исследования, в ходе которых сравнивали группы с наложением швов с группой без швов при многоплодной беременности. Суммарно из пяти исследований, включенных в обзор, были получены данные по 128 беременным с многоплодием (122 двойни и 6 троен). По первичным конечным точкам статистически значимой разницы между группами со швами и без швов выявлено не было: перинатальная смертность составила 19,2 и 9,5% соответственно (отношение рисков (ОР) 1,74, 95% доверительный интервал (ДИ) 0,92–3,28), серьезная неонатальная заболеваемость – 15,8 и 13,6% (ОР 0,96, 95% ДИ 0,13–7,1). Также не было выявлено достоверных различий и во вторичных показателях: преждевременные роды, ранние преждевременные роды, респираторный дистресс-синдром, частота кесарева сечения и материнских осложнений [20]. То есть результаты этого обзора не свидетельствуют об эффективности серкляжа при многоплодной беременности, однако такие данные могут быть следствием чрезвычайно малой выборки и гетерогенности групп в плане показаний к серкляжу. Кроме того, для анализа Кокрейновские эксперты традиционно отбирают только проспективные сравнительные исследования.
В то же время американским ученым при ретроспективном анализе даже небольшой выборки удалось показать, что швы все же могут быть эффективными при многоплодии. В 7 центрах ретроспективно проанализировали случаи расширения цервикального канала по данным ультразвукового исследования более 1 см в сроках 16–24 недели при многоплодной беременности. 38 пациенткам были наложены швы на шейку матки, у других 38 выбрали выжидательную тактику. При анализе проводили корректировку по применению прогестерона. В группе швов период с момента обнаружения расширения цервикального канала до родов составил 10,46±5,6 недель, в группе без швов – 3,7±3,2 недели. Помимо этого, в группе швов значительно ниже была частота преждевременных родов до 34 недель (52,6% по сравнению с 94,7% в группе выжидательной тактики, отношение рисков 0,06), до 28 недель (31,6% по сравнению с 89,4%, отношение рисков 0,05), а также до 24 недель (13,1% по сравнению с 47,3%, отношение рисков 0,17). Также в группе швов существенно ниже была перинатальная смертность (27,6% по сравнению с 59,2%) и частота госпитализации в отделение реанимации и интенсивной терапии (75,9% по сравнению с 97,6) [21].
В ходе другого ретроспективного анализа Roman и соавт. оценивали эффективность швов при укорочении шейки матки по данным ультразвукового исследования. Оказалось, что наложение швов при длине шейки матки менее 25 мм существенно не снижает частоту преждевременных родов и перинатальную смертность. Однако при анализе подгруппы с длиной шейки матки ≤15 мм оказалось, что наложение швов сопровождается значительным увеличением периода до начала родов до 12,5±4,5 недели (по сравнению с 8,8±4,6 недель в контрольной группе (P<0,001)), а также существенным снижением частоты родов до 34 недель с 79,5 до 50% [22].
Интересно, что, несмотря на сомнения в эффективности серкляжа при многоплодии, в США многоплодная беременность является основным фактором, ассоциированным с наложением швов. При одноплодной беременности швы на шейку матки накладывают приблизительно в 0,3%, при двойнях в 1,3%, при тройнях в 7,9%, а при многоплодии более высокого порядка – в 18%, то есть врачи все же верят в эффективность данного метода [23].
При опросе специалистов перинатальной медицины в Канаде оказалось, что практически никто из них не рекомендует своим пациенткам с многоплодием находиться на постельном режиме. 82% проводят рутинную регулярную оценку длины шейки матки по данным ультразвукового исследования с частотой от 1 раз в 2 недели (53,3%) до 1 раза в месяц (23,3%). 28% проводят своим пациенткам рутинную профилактику респираторного дистресс-синдрома глюкокортикоидами. Не рекомендуют рутинное наложение швов, но 71% производят серкляж при наличии преждевременных родов в анамнезе или при укорочении шейки матки [24].
Пессарии
Теперь рассмотрим информацию об эффективности пессариев, переживающих второе рождение в начале XXI века. В сравнении с наложением швов процедура гораздо более простая, безопасная, не требует анестезии и может проводиться в амбулаторных условиях. После появления новых модификаций пессариев, выполненных из современных материалов, их популярность продолжает расти.
Начнем вновь с Кокрейновского обзора, опубликованного в 2013 году. Эксперты смогли выявить лишь одно рандомизированное проспективное исследование, соответствовавшее критериям. В него были включены как одноплодные, так и многоплодные беременности и в целом была продемонстрирована высокая эффективность пессариев. Но выводов относительно их эффективности в группе многоплодных беременностей не удалось сделать в силу малого их количества [25]. В конце 2013 года были опубликованы результаты крупного многоцентрового рандомизированного исследования ProTWIN (Нидерланды) (Pessaries in multiple pregnancy as a prevention of preterm birth – пессарии при многоплодной беременности для предотвращения преждевременных родов), которое сделало большой шаг в выяснении роли пессариев в профилактике преждевременных родов при многоплодии (401 пациентка в группе пессариев, 407 – в контрольной группе). Первые выводы из исследования, опубликованные в 2013 году, свидетельствовали о том, что установка пессариев всем беременным с многоплодием не снижает ни частоту преждевременных родов, ни частоту неблагоприятных перинатальных исходов [26]. Следующим этапом проводился анализ в подгруппах. Оказалось, что при отборе только пациенток с длиной шейки матки менее 25‰ (38 мм) установка пессария существенно снижает частоту преждевременных родов до 32 недель и неблагоприятных перинатальных исходов. Кроме того, в подгруппе беременных с многоплодием и длиной шейки матки менее 38 мм установка пессария была и экономически эффективной [27].
Многофакторный анализ результатов данного исследования показал, что наиболее эффективным может оказаться постановка пессария при многоплодии у пациенток с короткой шейкой матки, монохориальной двойней и нерожавших пациенток. При тройне же пессарий не только не улучшает исход, но и, вероятно, ухудшает его [28].
Анализ результатов при учете только пациенток, закончивших протокол исследования (per protocol analysis), показал, что при исключении из массива данных пациенток, кому так и не был установлен пессарий, хотя они были рандомизированы в основную группу, и пациенток, которым пессарий был удален до 36 недель беременности, но роды у них в течение 7 дней не начались, эффективность пессариев у беременных с многоплодием и короткой шейкой матки возрастает еще больше [29]. Эти результаты свидетельствуют о том, что удалять пессарий до 36 недель нужно только при развитии регулярной родовой деятельности.
Очевидно, что анализ в подгруппах большого исследования, в ходе которого пессарии ставили всем беременным с двойнями, не может считаться достоверным. Необходимы дополнительные исследования, в которые отбирали бы только пациенток с укорочением шейки матки. И два таких исследования уже проведены. Результаты их, однако, противоречивы. M. Di Tommaso и соавт. на когорте 80 пациенток (40 в основной группе и 40 в конт-рольной) с многоплодной беременностью с длиной шейки матки менее 25 мм в сроках 21–31 неделя показали, что установка пессариев позволяет увеличить срок гестации на момент родов (35 по сравнению с 33 неделями в контрольной группе, р=0,02), снизить частоту родов до 36 и до 34 недель (р<0,05), но не родов до 32 недель. Интервал с момента выявления укорочения шейки матки до родов был значительно больше у пациенток, которым поставили пессарий [30]. Результаты исследования M.J. Monfrance и соавт. свидетельствовали об отсутствии эффективности пессариев при многоплодной беременности и укорочении шейки матки. В основной группе было 63 пациентки, группу контроля составили 56 беременных. Но данное исследование не было проспективным (для сравнения использовали ретроспективную группу), пороговым значением укорочения шейки матки считали 38 мм [31]. Таким образом, данных в пользу установки пессариев в группе беременных с многоплодием и укорочением шейки матки все же больше, чем против.
В настоящее время проводится сразу несколько проспективных рандомизированных исследований с целью оценки эффективности швов и пессариев при многоплодной беременности, но уже сейчас на основании проанализированного нами массива знаний можно сделать определенные выводы.
Выводы
- Не следует накладывать швы или устанавливать пессарии всем пациенткам с многоплодием. Такая мера однозначно не даст ожидаемого результата.
- Нет необходимости в оценке длины шейки матки при многоплодии в ходе ультразвукового исследования в сроке 16–17 недель. Оптимальным сроком является 18 недель с повторением исследования в 20, 22 и 24 недели.
- При укорочении шейки матки в сроке до 22 недель менее 15 мм однозначно показаны швы на шейку матки, также следует рассмотреть возможность проведения серкляжа при длине шейки матки 15–25 мм, но вторым вариантом лечения в этой подгруппе является акушерский пессарий.
- Пессарий, вероятно, целесообразно устанавливать при укорочении шейки матки менее 25 мм в сроках до 30 недель беременности.