Clinical and morphological characteristics of the endometrium in intrauterine synechiae: evaluation of the expression of estrogen and progesterone receptors
Khirieva P.M., Martynov S.A., Ezhova L.S., Adamyan L.V.
Objective. To evaluate the expression of estrogen receptors (ER) and progesterone receptors (PR) in the nuclei of the glandular epithelium and endometrial stroma, and intrauterine synechiae in reproductive-aged women. Subjects and methods. Endometrial samples from 30 patients with intrauterine synechiae and from 10 control group patients, who had been operated on at the Department of Gynecology, V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, were examined during a prospective study. Endometrial tissue samples were taken using pipelle biopsy and then morphologically studied by the standard procedure. Histological findings could reveal 3 grades of intrauterine synechiae. Immunohistochemical examination was made using monoclonal antibodies against PR (clone 636, Dako, Denmark) and ER (clone 1D5, Dako, Denmark); the Dako REAL EnVision system (Dako, Denmark) served as secondary antibodies. After immunohistochemical reactions, the sections were contrasted with hematoxylin and eosin and placed into the Shandon mount TM medium (USA). The degree of nuclear staining intensity was determined by a semiquantitative assay. Results. The immunohistochemical examination showed that the ER expression in the glandular epithelium and endometrial stroma was significantly higher in the women with moderate and medium intrauterine synechiae than that in the apparently healthy women; that the PR expression in the glandular epithelium and endometrial stroma was lower in the women with all grades of the adhesive process than that in the endometrium of the apparently healthy women. Conclusion. The found increased ER expression in the epithelium and stroma of intrauterine synechiae and surrounding endometrium in the proliferative phase of the menstrual cycle in reproductive-aged women with grades I and II intrauterine synechiae, as well as the decreased ER expression in all grades of the process are a prerequisite for a differentiated approach to prescribing hormone therapy after surgical adhesiolysis.
Keywords
Intrauterine adhesions, first described by Heinrich Fritz in 1894, are still a problem of women’s reproductive health. Characterized by partial or complete obliteration of the uterine cavity with fibrous tissue, intrauterine adhesions can cause menstrual dysfunction, habitual pregnancy loss, infertility. Hysteroscopic adhesiolysis is the main method of treatment of this pathology. However, the high recurrence rate, reaching 62.5%, requires the search for new methods of treatment and prevention [1, 2]. According to most authors, endometrial trauma is considered to be the main cause of the formation of intrauterine adhesions, but the role of other factors such as infections, increased cytokine expression, hypoxia, and decreased vascularization is not excluded [3]. In addition, there are cases of the formation of intrauterine adhesions without prior injury of the endometrium [4].
The functional layer of the endometrium is a tissue with high regenerative properties, subjected to growth, differentiation and rejection throughout the menstrual cycle of the woman of reproductive age. Fluctuations in circulating estrogen and progesterone levels support this state of “endometrial remodeling” [5]. It is known that even with a relatively small injury, the endometrium can become immune to steroid hormones, which leads to the disorder of menstrual and reproductive function, in particular with intrauterine adhesions [2, 6].
In this regard, we conducted a study to assess the expression of estrogen (ER) and progesterone (PgR) receptors in the nuclei of glandular epithelium and stroma of the endometrium and intrauterine adhesions in women of reproductive age.
Materials and methods
This was a prospective study of 30 patients of reproductive age with intrauterine adhesions and 10 patients of the comparison group who applied for the selection of contraception, and who underwent a full clinical and laboratory examination and treatment in the Gynecology Department and Department of Pathology of the National Medical Research Center of Obstetrics, Gynecology and Perinatology (NMRC of OGP) named after Academician V. I. Kulakov of the Ministry of Health of Russia in 2015-2016. All patients before being included in the study signed an informed consent. The study was approved by the ethics Committee of NMRC of OGP named after Academician V.I.Kulakov Ministry of Health of Russia.
According the American Fertility Society classifications (1988) based on hysteroscopy the patients were divided into four groups for immunohistochemical studies. The 1st group included patients with intrauterine adhesions, I degree (n=10), the 2nd group included patients with intrauterine adhesions, II degree (n=10), the 3rd group included patients with intrauterine adhesions, III degree (n=10), the 4th group was the comparison group, it included healthy patients (n=10).
The inclusion criteria in the main groups were the age of patients from 18 to 45 years, the presence of intrauterine adhesions, identified by hysteroscopy and confirmed by histological examination, proliferative phase of the menstrual cycle. The criteria for exclusion from the study were the age of patients less than 18 and more than 45 years, patients taking hormonal drugs at the time of treatment, severe concomitant somatic pathology, malignant tumors in the history, acute pelvic inflammatory diseases. The hysteroscopic stage was performed according to the standard procedure in the Gynecology Department under the conditions of appropriate anesthetic support.
Endometrial samples and intrauterine adhesions obtained during hysteroscopy and endometrial biopsy were used as the material for the study. The material was fixed in 10% neutral formalin with phosphate buffer, processed in Shandon apparatus and poured into paraffin. The total time of fixing, wiring and pouring did not exceed 48 hours. Paraffin sections 4-5 microns thick were stained with hematoxilin and eosin.
For immunohistochemical studies, 4 µm thick sections were applied to highly adhesive slides and dried for 18 hours at a temperature of 37°C. After removing the paraffin from the sections, they were rehydrated in an alcohol battery of 95, 80, 70, incubating in each solution for 2 minutes. Recovery of antigenic activity was performed in a PT Link (“Dako”) in the buffer EnVision pH of 9.0 for 20 minutes at a temperature of 97°C. The cooled glasses were placed in wet chambers (to prevent the sections from drying out) and incubated in a 3% solution of hydrogen peroxide for 15 minutes to block the endogenous peroxidase. The reaction with primary antibodies was carried out for 30 minutes at room temperature. Monoclonal antibodies to ER (clone 1D5, RTU, Dako, Denmark) and PgR (clone PgR636, RTU, Dako, Denmark) were used in the study. To visualize the binding sites of antibodies with antigens, the oxidation reaction of the substrate 3.3-diaminobenzidine (DAB) with horseradish peroxidase in the presence of hydrogen peroxide to form a water-insoluble brown end product of the EnVision system (“Dako Cytomation”) was used. For the correct formulation of immunohistochemical reactions put positive and negative controls. As negative controls, samples of the studied sections were taken, which were subjected to the standard procedure of immunohistochemical reaction, but without the addition of primary antibodies. Positive controls for each antibody were selected according to the specifications of the manufacture. After immunohistochemical reactions, the sections were contrasted with hematoxilin and enclosed in a synthetic medium “Shandon mount TM” (USA). In assessing the results of immunohistochemical reactions, nuclear staining of cells was taken into account and a semi-quantitative H – Score method was used according to the formula S=1a+2b+3c, where a is percentage of weakly colored nuclei, b is percentage of moderately colored nuclei, c is percentage of strongly colored nuclei. The intensity of the brown color from the pale-colored kernels to intensely colored kernels was estimated according to the recommendations of the McClelland [7]. The diagnosis of “intrauterine adhesions” was made according to WHO recommendations.
Statistical data processing was performed using software package SPSS Statistics 17.0. Differences were considered statistically significant at p<0.05.
Research Results
The average age of women in the 1st group amounted to 34.5±7.45 years, in the 2nd group – 30.6±6.06 year, in the 3rd group - 33.9±4.8 years, in the 4th group - 32.00±5.14 years. The average age of menarche was 12.8±1.07 years in the 1st group; 12.2±1.16 years – in the 2nd group; and 13.3±1.2 years – in the 3rd group; and 12.5±1.3 years – in the 4th group. The duration of menstruation is 3 to 5 days, on average 5.76±1.43 days in the 1st group, 4.80±0.77 days – in the 2nd group, 5.5±1.3 days – in the 3rd group, and 5.2±1.4 days in 4th group. The duration of the menstrual cycle varied from 26 to 30 days, averaging 28.35±0.70, 29.87±4.42, 30.5±2.0, 30.5±3.1 days, respectively.
The analysis of the past operative interventions revealed a high frequency of diagnostic curettage of the uterine mucous in the history of patients from the main group: 6 (60%) patients of the 1st group, 7 (70%) patients of the 2nd group, 10 (100%) patients of the 3rd group.
Endometrial morphological examination of 30 patients from groups 1-3 revealed chronic endometritis in 25 (83.3%) cases, which was represented by scattered and small-focal lymphoid infiltration around the glands and small vessels. The composition of the lymphoid infiltrate included plasma cells and macrophages. In some areas there were marked fibrous changes in the stroma and signs of neoangiogenesis. In addition, it should be noted that hyperplasia of the basal layer of the endometrium was revealed in groups 1-3: 11 (6.7%), 2 (5%), 2 (4.7%) cases, respectively.
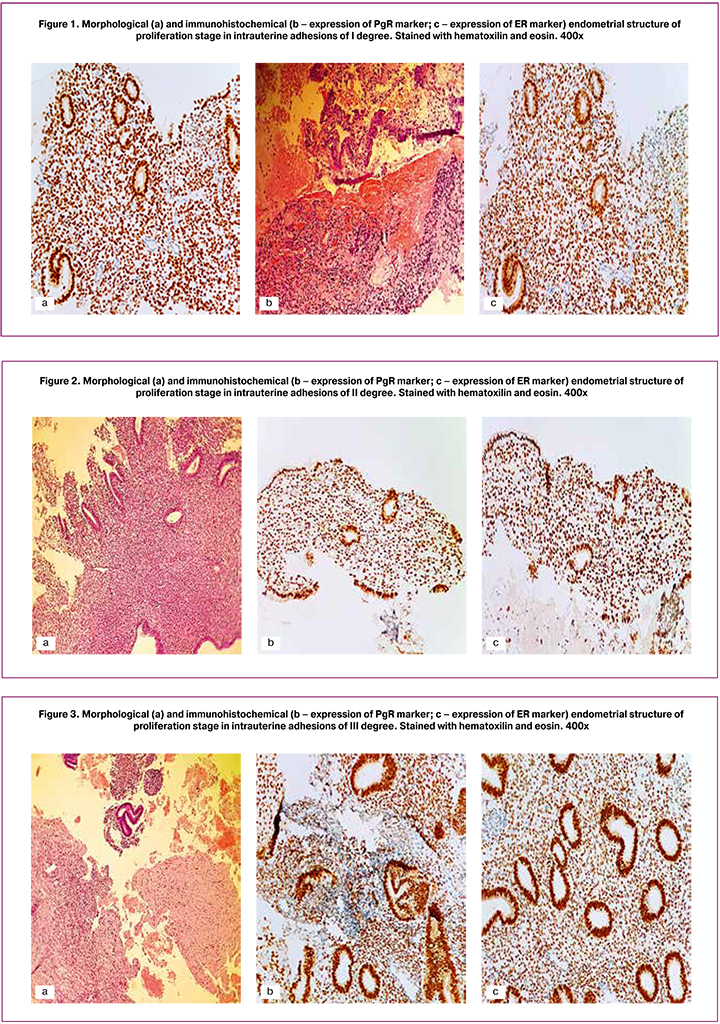
Synechiae with I degree of severity (group 1) were represented by fragments of thin connective tissue covered with the endometrium, with single glandular structures of different shapes and sizes, distributed unevenly, individual glands with cystic dilation (Fig. 1A). Synechiae with II degree (group 2) were represented by fibrous tissue with single glandular structures, sclerosed blood vessels, with the inclusion of areas of muscle tissue, often with hyalinosis, covered with the endometrium (Fig. 1B). Synechiae with III degree (group 3) were represented by coarse fibrous tissue, often devoid of glandular component, with circulatory disorder and decay, sclerosed vessels (Fig. 1B).
The results of immunohistochemical studies are presented in Table 1.
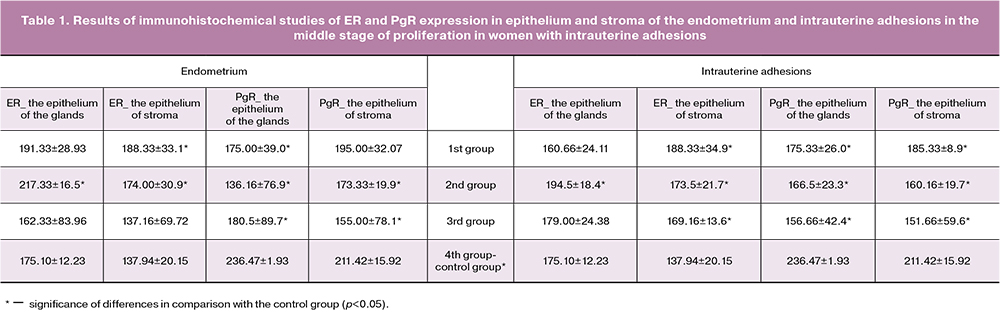
The ratio of expression of PgR and ER in the glands of the endometrium in the 1st group was 0.91 (p>0.05), in the 2nd group of 0.62 (p<0.05) in the 3rd group of 1.11 (p>0.05); the ratio of expression of PgR and ER in the stroma of the endometrium in the 1st group was 1.03 (p>0.05), in the 2nd group – 0,99 (p<0.05), in the 3rd group it was 1.13 (p>0.05); at a rate from 2 to 4.
The ratio of expression of PgR and ER in the glands of intrauterine adhesions in the 1st group consisted of 1.09 (p>0.05), in the 2nd group - 0.85 (p<0.05), in the 3rd group - 0.87 (p>0.05); the ratio of expression of PgR and ER in the stroma in the 1st group amounted to 0.98 (p<0.05), in the 2nd group – 0.92 (p<0.05), in the 3rd group – 0.89 (p<0.05); at a rate from 2 to 4.
Thus, the study revealed an increase in the expression of ER in the endometrium and intrauterine adhesions in the proliferative phase of the menstrual cycle at mild and moderate severity of the process, as well as a decrease in PgR expression with all degrees of severity of the process.
Discussion
The obtained anamnestic and clinical data showed the relative homogeneity of the studied groups and were comparable with the results of other authors [4, 8]. The study of patients’ history in our research revealed a high frequency of intrauterine interventions in the uterine cavity in the main group, which confirms the role of iatrogenic factor in the formation of intrauterine adhesions [2, 4].
Morphological characteristics of intrauterine adhesions on the basis of comparison of hysteroscopic data revealed a significant replacement of the endometrium with fibrous tissue in patients of group 3 compared to patients of group 1.
The concept of “receptivity of the endometrium” has been widely used in the scientific literature since the 50s of the last century. Different levels of regulation of this process – genetic, proteomic, histological – suggest its versatility and confirm the need for a comprehensive assessment of the parameters of the endometrium, taking into account the influence of pathological processes on fine-tuning mechanisms [9-11].
ER and PgR, widely represented on the mucous membrane of the uterus, play an important role in the regulation of the reproductive system. After binding the receptors to estrogen and progesterone, signaling pathways are activated to initiate cell differentiation processes necessary for the normal functioning of the endometrium [12]. Our study revealed statistically significant changes in endometrial receptivity in women with intrauterine adhesions of group 1 and 2, manifested in an increase in the level of ER expression, which is consistent with the data of Gan and et al. [13], and reduction of PgR expression in the nuclei of glandular epithelium and stroma. Higher ER expression in the epithelium of the endometrium in women with intrauterine adhesions suggests a higher sensitivity of these structures to estrogen, which evolved compensatorily. At the same time, higher expression of ER receptors in the endometrial stroma of women with intrauterine adhesions, compared with the endometrial stroma of healthy women, justifies trophic paracrine interaction between stroma and epithelial cells [7].
Low PgR expression in the epithelium and stroma of intrauterine adhesions and in the endometrium of women with intrauterine adhesions compared to the endometrium of healthy women explains the low sensitivity to gestagens. At the same time, our study revealed a significant decrease in the expression of PgR in the epithelium of the glands and stroma of the endometrium in women with intrauterine adhesions at all degrees of severity compared to the control group, which can be explained by the replacement of the endometrium with coarse fibrous tissue, which is less active compared to the endometrium of women in the comparison group.
Intrauterine adhesions have been noted to be combined most frequently with chronic endometritis; it was revealed in 83.3% of cases. According to A. V. Shurshalina [9], in chronic endometritis there was an increase of more than 2 times of ER and PgR expression in the nuclei of glandular epithelium cells compared to the control group (p<0.05); the tendency to increase the expression of receptors was also noted in stroma cells (p>0.05). These data contradict the results of A. R. Kotikov [14], according to which the low sensitivity of the endometrium to progesterone in chronic endometritis is a consequence of a decrease in PgR and to a lesser extent ER in response to chronic inflammation in the cells of the glands and stroma.
At the same time, V. K. Tabolova’s study [15] revealed no statistically significant differences between ER and PgR expression in the stroma and glands in patients of the main and control groups in the study of the receptor status of endometrium in patients with chronic endometritis. Such heterogeneity of the obtained data can be explained by different blood flow in the vessels of the endometrium, which was confirmed in B.I. Zheleznov’s works [16]. Focal stroma fibrosis, common sclerotic changes in the walls of blood vessels make the endometrium inactive, defective for binding steroid hormones with specific receptors. Due to such gross structural and dystrophic changes in the mucous membrane of the uterine cavity, mainly in the stroma, secretory transformation of the endometrium as the development of an inferior stage of secretion does not occurin each fifth patient with chronic endometritis.. In confirmation of this, in E.B. Rudakova’s work of [17], a direct weighted average relationship between the preserved blood flow in the endometrial vessels and the intensity of ER and PgR distribution in the glands and stroma was revealed. In addition, it should also be pointed out that different ER and PgR expression in the cells of the glands and stroma may reflect different stages of the pathological process and indirectly characterize the compensatory capabilities of the endometrium.
It should be noted that changes in the receptivity of intrauterine adhesions, first identified in our study separately from the surrounding endometrium, allowed us to talk about the phenomenon of “mimicry” - synechium epithelium performs the function of residual endometrium, which is manifested by almost similar levels of expression, both ER and PgR.
Taking into account the results of previous studies and the data obtained by us, it can be concluded that significant changes in the receptivity of the endometrium and intrauterine adhesions with I and II degrees of severity of the process, consisting in the increase of ER expression, are associated with a changed ratio of stromal and glandular components, due to their compensatory reaction in the areas of the preserved endometrium. A significant decrease in PgR expression in the endometrium and intrauterine adhesions with all degrees of severity of the adhesive process is a consequence of inhibition of stromal and epithelial cells, which is associated with the replacement of healthy endometrial fibrous tissue.
Thus, the revealed changes in receptivity can serve as a prerequisite for a differentiated approach to hormonal therapy in patients with intrauterine adhesions after surgical adhesiolysis. In particular, the immunohistochemical data obtained by us explain the absence of the need for hormonal therapy in patients of group 1 (with normal ER expression). A significant increase in ER expression in the 2nd group demonstrates the need for hormone therapy, namely for patients with moderate severity degree process using higher doses of estrogens. A less pronounced increase in ER expression in group 3 (only in the stroma of the synechiae themselves) is due to decompensation of reparative processes combined with the replacement of a significant part of the endometrium with coarse connective tissue and explains the lower efficiency of the treatment and a higher recurrence rate.
Conclusion
- Endometrial receptivity disorders were found in all degrees of severity of intrauterine adhesions; the severity of these disorders rises with increasing severity of the process.
- Receptivity disorders are manifested by an increase in ER expression and a decrease in PgR expression, both in the endometrium and in the intrauterine synechiae.
- In I and II degrees of severity of the process the epithelium of adhesions functions as the epithelium of the endometrium (the phenomenon of “mimicry”), thereby fulfilling a compensatory function.
- A significant increase in ER expression was revealed in group 2 (with moderate severity). A less pronounced increase in ER expression in group 3 (only in the stroma of synechiae) is due to decompensation of reparative processes combined with the replacement of a significant part of the endometrium with coarse connective tissue and explains the lower efficiency of the treatment and a higher recurrence rate.
References
- Khirieva P.M., Adamyan L.V., Martynov S.A. Modern methods of prevention and treatment of intrauterine synechia (literature review). Ginekologiya. 2016; 18(5): 32-6. (in Russian)
- Khirieva P.M., Adamyan L.V. Clinical and anamnestic data and treatment outcomes for women with intrauterine synechia. Reproduction problems. 2017; 23(6): 39-44. (in Russian)
- Xue X., Chen Q., Zhao G., Zhao J.Y., Duan Z., Zheng P.S. The overexpression of TGF-β and CCN2 in intrauterine adhesions involves the NF-κB signaling pathway. PLoS One. 2015; 10(12): e0146159.
- March C.M. Asherman's syndrome. Semin. Reprod. Med. 2011; 29(2): 83-94.
- Gargett C.E., Nguyen H.P., Ye L. Endometrial regeneration and endometrial stem/progenitor cells. Rev. Endocr. Metab. Disord. 2012; 13(4): 235-51.
- Johary J., Xue M., Zhu X., Xu D., Velu P.P. Efficacy of estrogen therapy in patients with intrauterine adhesions: systematic review. J. Minim. Invasive Gynecol. 2014; 21(1): 44-54.
- Kogan E.A., Sattarov Sh.N., Sarkisov S.E., Boiko M.A., Mamikonyan I.O. The receptor status of endometrial polyps in postmenopausal women. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2014; (2): 60-6. (in Russian)
- Adesiyun A.G., Zayyan M.S., Eka А., Williams I.O., Ojabo A. Clinical and investigative correlates of etiologic risk factors on treatment outcome of intrauterine adhesion in women with infertility: A descriptive study. Open J. Obstet. Gynecol. 2014; 4: 95-9.
- Shurshalina A.V., Demura T.A. Morphofunctional rearrangements of the endometrium during the implantation window. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2011; (7-2): 9-13. (in Russian)
- Niauri D.A., Gzgzyan A.M., Kvetnoy I.M., Kogan I.Yu., Dzhemlikhanova L.Kh., Krikheli I.O., Fedorova I.D., Lesik E.A., Sharfi Yu.N., Krylova Yu.S., Shilnikova E.M. Immunohistochemical characteristics of endometrial receptivity in IVF cycles. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2014; (9): 44-50. (in Russian)
- Khirieva P.M., Kuznetsova M.V., Bystritsky A.A., Martynov S.A., Burmenskaya O.V., Trofimov D.Yu., Adamyan L.V. Investigation of the gene mRNA level in the endometrial tissue of reproductive-aged women with intrauterine synechiae. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (2): 56-64. (in Russian) https://dx.doi.org/10.18565/aig.2018.2.56-64
- Wang J., Ju B., Pan C., Gu Y., Zhang Y., Sun L. et al. Application of bone marrow-derived mesenchymal stem cells in the treatment of intrauterine adhesions in rats. Cell. Physiol. Biochem. 2016; 39(4): 1553-60.
- Gan L., Duan H., Wang S., Xu Q., Tang Y.Q., Zhonghua F. Expression of ER and PR in the endometrium of patients with intrauterine adhesions. Zhonghua Fu Chan Ke Za Zhi. 2017; 52(1): 47-52.
- Kotikov A.R., Ali-Riza A.E., Smirnov A.N. Expression of endometrial receptors for estrogens and progesterone in infertility due to chronic endometritis. Problemy reproduktsii. 2006; 2: 7-10. (in Russian)
- Tabolova V.K. Clinical and molecular genetic basis for the preparation of the endometrium in chronic endometrium in programs of assisted reproductive technologies: diss. ... cand. med. sciences. Moscow; 2016. (in Russian)
- Zheleznov B.I. Structural changes in the mucous membrane of the uterus and ovarian function in chronic endometrium. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 1977; 4: 3-7. (in Russian)
- Rudakova E.B., Loboda O.A. Chronic endometritis in terms of the effectiveness of in vitro fertilization programs. Therapist. 2012; 11: 22. (in Russian)
Received 13.04.2018
Accepted 20.04.2018
About the Authors
Khirieva, Patimat M., postgraduate student of gynecological department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Ac. Oparina str. 4. Tel.: +74954387783. E-mail: dr.khirieva@rambler.ru. ORCID:0000-0002-3440-4121Martynov, Sergey A., MD, Leading Researcher of gynecological department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Ac. Oparina str. 4. Tel.: +74954387783. E-mail: s_martynov@oparina4.ru
Ezhova, Larisa S., PhD, senior scientific researcher of department of anatomic pathology, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Ac. Oparina str. 4. Tel.: +74954382311. E-mail: l_ezhova@oparina4.ru
Adamyan, Leyla V., MD, professor, Academician of RAS, Deputy Director for Science, Head of gynecological department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia.
117997, Ac. Oparina str. 4. Tel.: +74954387783. E-mail: l_adamyan@oparina4.ru
For citations: Khirieva P.M., Martynov S.A., Ezhova L.S., Adamyan L.V. Clinical and morphological characteristics of the endometrium in intrauterine synechiae: evaluation of the expression of estrogen and progesterone receptors. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (9): 48-54. (in Russian)
https://dx.doi.org/10.18565/aig.2018.9.48-54