Clinical and anamnestic features of diseases of the cervix
Objective: Investigation of risk factors for tumor transformation based on the study of clinical and anamnestic features of the course of various pathological processes in the cervix. Materials and methods: The study included 210 female patients of reproductive age, who were divided into 5 groups: group 1 consisted of 37 women with cytological findings "NILM"+high carcinogenic risk of human papillomavirus (HR HPV); group 2 consisted of 43 women with cytological findings "LSIL"+HR HPV; group 3 consisted of 46 patients with cytological findings "HSIL"+HR HPV; group 4 comprised 39 patients with cytological findings "NILM", hyperkeratosis of squamous epithelium an absence of HPV; group 5 (the comparison group) comprised 45 women with cytological findings "NILM" and the absence of HPV. Results: The severity of cervical intraepithelial lesions was not associated with the age of patients and the intake of oral contraceptives. The patients with LSIL+HR HPV and HSIL+HR HPV had early sexual debut (the average age of 17 years), (p<0,001). It was found that the severity of intraepithelial lesions and duration of HPV persistence depended on the number of sexual partners (p<0,001). The largest number of smoking patients (51.2% and 41,3%) and women with early sexual debut were in the groups with mild and severe cervical intraepitheliasl lesions in combination with HR HPV (p<0.001). Sexually transmitted infections were significantly more common in women infected with HR HPV. A combination of endometriosis, uterine fibroids, endometrial hyperplasia and benign mammary dysplasia was found in patients with HPV and squamous intraepithelial lesions of the cervix (p<0.001). Conclusion: Analysis of the anamnestic data and specific features of the clinical cause of pathological processes in the cervix confirmed again the significance of the importance of certain factors in tumor formation and transformation of cervical epithelial cells. Authors’ contribution: Levakov S.A. – the concept of the study, search for literature data; Obukhova E.A., Dzhafarova M.M. – conduction of the study, analysis of the research data; Shenshukova N.A., Kaviladze M.G. – article editing. Conflicts of interest: The authors declare that they have no conflict of interest to declare. Funding: The study was conducted without any sponsorship. Ethical Approval: This study was been approved by the local Ethics Committee of I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University) on January 20, 2022. Patient Concent for Publication: The patients signed informed consent for publication of their data. Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator. For citation: Levakov S.A., Obukhova E.A., Sheshukova N.A., Dzhafarova M.M., Kaviladze M.G. Clinical and anamnestic features of diseases of the cervix. Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2023; (9): 122-128 (in Russian) https://dx.doi.org/10.18565/aig.2023.90Levakov S.A., Obukhova E.A., Sheshukova N.A., Dzhafarova M.M., Kaviladze M.G.
Keywords
Сervical cancer ranks third in terms of frequency of occurrence after malignant neoplasms of breast and body of the uterus (https://gco.iarc.fr/today). There is an increase in the incidence rate of cervical cancer in women of reproductive age in the structure of oncological diseases. In 2020, the prevalence of cervical cancer among women of childbearing age in Russia was in 21361 (13.8%) cases (https://gco.iarc.fr/today). Mortality rate within one year after the diagnosed cervical cancer decreased over ten years and was 16.3% versus 20.8% in 2004.
Despite the fact that the role of human papillomavirus (HPV) in the development of malignant degeneration of the cervical epithelium has been determined, the occurrence of the pathological process is impossible without additional risk factors leading to changes in the genetic material of cells resulting from the introduction of the HPV genome into the host genome [2, 3]. The role of HIV in the pathogenesis of HPV-associated cervical cancer is proven [4, 5].
According to the findings of multiple research studies, the relationship between the development of cervical cancer and smoking [6–8], early onset of sexual activity and a great number of sexual partners [9–11], the use of hormonal contraceptives [12, 13], immune suppresiion [14, 15], traumatic cervical injury, low social status and long-term persistence of sexually transmitted infections [16, 17] was noted.
Several studies found that in women, who had two or more abortions and births in medical history, the risk of cervical cancer is 5 times higher than in the population [18]. Nevertheless, this association was not confirmed by other studies.
Thus, a large number of publications reflecting the results of epidemiological studies indicate the relationship between cervical cancer development and many interdependent factors. In this regard, it seems relevant to continue to study anamnestic and clinical features of the course of cervical disorders to identify the risk group for precancerous conditions of the cervix and develop timely treatment strategy.
Early diagnosis and effective treatment of preinvasive lesions remain the most effective way to prevent cervical cancer [19–21].
The purpose of the study was investigation of risk factors for tumor transformation of cervical epithelial cells based on the study of clinical and anamnestic features of the course of various pathological processes in the cervix.
Materials and methods
The prospective study included 210 female patients of reproductive age. Depending on the changes in the cervix, the cytological and histological findings, as well as HPV test results, the patients were divided into 5 groups: group 1 consisted of 37 women with cytological result of negative for intraepithelial lesion or malignancy (NILM) and high carcinogenic risk of HPV (HR HPV); group 2 consisted of 43 women with cytological result of low-grade squamous intraepithelial lesion (LSIL) and HR HPV; group 3 consisted of 46 patients with cytological result of high grade squamous intraepithelial lesion (HSIL) and HR HPV; group 4 comprised 39 patients with cytological result of NILM, hyperkeratosis of squamous epithelium and absence of HPV; group 5 (the comparison group) comprised 45 women with cytological result of NILM and no HPV. All patients who participated in the study received all necessary information and signed informed consent to participate in the study.
Exclusion criteria for study participants were: acute pelvic inflammatory disease; irregular periods; HPV vaccination; pregnancy, postpartum period and lactation; oncological and autoimmune diseases; decompensation stage of extragenital diseases; hormone intake; patient’s refusal to participate in the study; protocol violation.
Patients’ passport data, contact information, marital status, complaints, epidemiologic anamnesis, social history, hereditary diseases, past medical history and chronic diseases, surgical interventions, gynecological and obstetric history were collected. The gynecological history included information about the age at menarche, characteristics of the menstrual cycle, sexual debut, the total number of sexual partners, sexual activity, the data related to pregnancies and pregnancy outcomes, gynecological diseases and surgical interventions, and methods of contraception. Inheritance data, the presence of allergies, bad habits (drinking alcohol, narcotic and toxic substances, smoking) were taken into account. The history of cervical diseases was described in detail, including the presence of human papillomavirus infection, viral load and duration of viral persistence, the methods that were previously used for diagnosis and treatment of cervical diseases.
Statistical analysis
Software program StatTech v.2.1.0 (“Stattech”, Russia) was used for statistical analysis. The Shapiro–Wilk test was used to estimate normal distribution of the quantitative parameters (the number of examined patients ˂50) or the Kholmogorov–Smirnov test (the number of examined patients ˃50).
The formula for the W value of the Shapiro–Wilk test is:
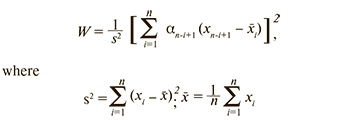
the numerator is the sum of squares of standard deviation according to Lloyd’s model;
coefficients an-i+1 are the known constants taken from the tables.
The formula for the Dn value of the Kholmogorov–Smirnov test:
where Xn – the sample of independent identically distributed random variables, Fn(x) – the empirical distribution function;
F(x) – “true” distribution function with known parameters.
In the absence of normal distribution, the quantitative data were described using median (Me) and lower and upper quartiles (Q1–Q3). The categorical data were described using absolute values and percentage. The Kruskal–Wallis test was used for comparison between quantitative variables in the groups that differed from normal distribution. Post-hoc Dunn's test with the Holm correction was used for A posteriori comparisons.
The comparison of percentages in four-fold contingency tables was madeut using Pearson’s chi-square test (for the values of the expected phenomenon ˃ 10).
The strength and direction of correlation between two quantitative variables was assessed using Spearman's rank correlation coefficient (when distribution of variables differed from normal).
Results
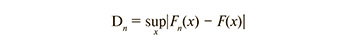
Analysis of clinical and anamnestic data of all patients participating in the study were comparable with regard to age, characteristics of menstrual function and frequency of extragenital diseases. Fig. 1 shows the median age of examined women.
Anthropometric measurement did not detect any significant differences between the groups. Obesity was identified in 27/210 (12.86 %) patients: in group 1 (NILM and HR HPV) in 5/37 (13.5%) women; in group 2 (LSIL and HR HPV) in 8 /43 (18.6%) patients, in group 3 (HSIL and HR HPV) in 5/46 (10.9%) women; in group 4 (NILM, hyperkeratosis of squamous epithelium, HPV) in 4/39 (10.3%) patients; in group 5 (NILM and absence of HPV) in 5/45 (11,1%) patients.
Analysis of sexual activity showed that the age at sexual initiation for most women under study was 17–20 years. However, earlier sexual debut was in group 2 (LSIL and HR HPV) and group 3 (HSIL and HR HPV), and the average age of first sexual intercourse was 17 years (p<0.001) (Fig. 2).
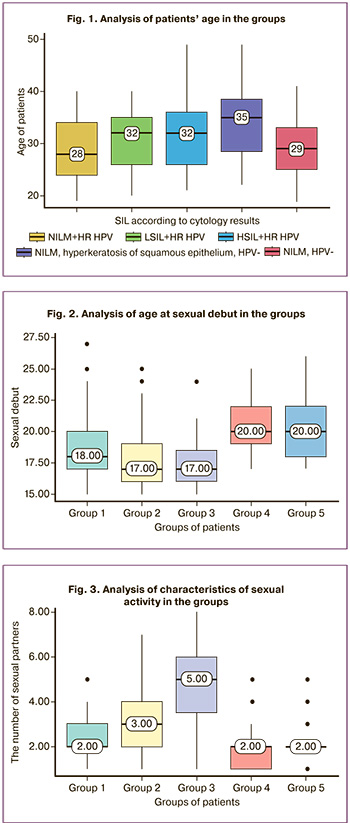
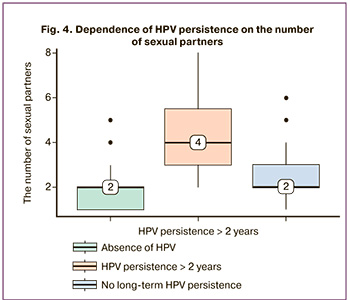
The average number of sexual partners at the time of being enrolled in the study was 2 in group 1 (NILM and HR HPV), 3 in group 2 (LSIL and HR HPV), 5 in group 3 (HSIL and HR HPV), 2 in group 4 (NILM, hyperkeratosis of squamous epithelium, no HPV) and 2 sexual partners in group 5 (NILM, no HR HPV) (Fig. 3). According to the assessment results, the total number of sexual partners in patients with LSIL and HSIL was statistically higher versus other groups. At the same time, the severity of intraepithelial lesions depended on the number of sexual partners (p<0.001).
The results of the study showed that duration of HPV persistence also depended on the number of sexual partners. The patients with long-term HPV persistence had in average a higher number of sexual partners (Me=4) in anamnesis versus women with no HPV according to the results of polymerase chain reaction test or with the length of infectious period less than 2 years (Me=2) (p<0.001) (Fig. 4).
The analysis of obstetric anamneses detected statistically significant differences: most pregnancies were in groups of patients with LSIL and HSIL, and the average number of pregnancies was 4 (Fig. 5). The severity of intraepithelial lesions did not depend on the number of pregnancies (p>0.05). The lowest number of pregnancies in history was in group 1 and group 5 with normal cytology results, and the average number of pregnancies was 2 (p<0.001).
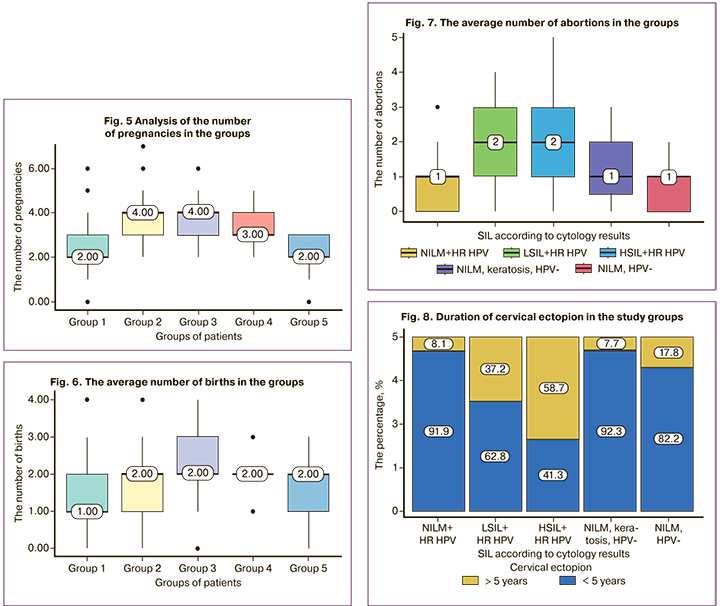
The highest number of births was found in group 3 (HSIL and HR HPV), and the average number was ˃ 2 (p=0.001) (Fig. 6).
The highest average number of abortions in history was 2 in group 2 (LSIL and HR HPV) and group 3 (HSIL and HR HPV) (Fig. 7). In the groups of patients with squamous intraepithelial lesions, the number of abortions in history was statistically higher versus the group of patients with normal cytology despite the presence of HPV (p<0.001). However, according to the result of analysis, the grade of intraepithelial lesion did not depend on the number of abortions in history. The results of analysis showed that there was no statistically significant difference in the average number of abortions between the group of patients with cervical leukoplakia (group 4) and the group of patients without pathological changes of the cervix (group 5) (р>0.05).
According to gynecological anamnesis, cervical ectopion for more than 5 years significantly more often was found in group 2 (LSIL and HR HPV) and group 3 (HSIL and HR HPV), in 16 /43 (37.2%) and 27/46 (58.2%) cases, respectively (Fig. 8). In the group of patients with HSIL cervical ectopion for more than 5 years (p<0001) was detected most often.
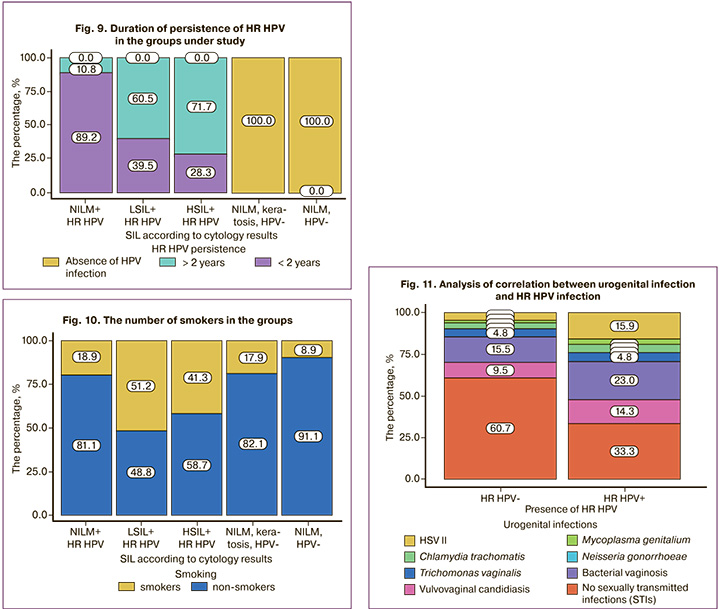
According to the results of the study, persistence of HR HPV in cervical epithelium for more than 2 years was detected in в 59/89 (66.3%) cases of squamous intraepithelial lesions: in 26/43 (60.5%) women in group 2 (LSIL and HR HPV) and in 26/43 (60.5%) women in group 3 (HSIL and HR HPV) (Fig. 9).
In patients with HPV and squamous intraepithelial lesions of the cervix, a combination of endometriosis, uterine fibroids, endometrial hyperplasia and benign mammary dysplasia was found significantly more often versus the comparison group. Endometriosis was diagnosed more often in women with cervical dysplasia. However, the frequency of occurrence did not depend on the grade on intraepithelial lesion in 29/43 (675%) women in group 2 (LSIL and HR HPV) and in 27/46 (58,7%) women in group 3 (HSIL and HR HPV).
Frequency detection of uterine fibroids by pelvic ultrasound was highest in group 2 and group 3, and was in 14/43 (32.6%) and 19/46 (41.3%) cases, respectively.
Breast ultrasound in patients with cervical dysplasia, benign mammary dysplasia was detected most often: 0 (0%) in group 1 (NILM and HR HPV), 8/43 (18.6%) patients in group 2, 12/46 (26.1%) in group 3 (HSIL and HR HPV), 5 /39(12.8%) in group 4 (NILM, hyperkeratosis of squamous epithelium and no HPV) and 1/45 (2.2%) patient in the comparison group (NILM, absence of HPV).
It can be probably assumed that there is a high proliferative potential, resistance to apoptosis, high aromatase activity, activation of oxidative stress and inflammation in women with squamous intraepithelial lesions.
Regular smoking for more than 5 years was noted in 59/210 (28.1%) examined women, 43/210 (20.47%) patients abandoned smoking, 63/210 (30%) patients were intermittent hookah and cigarette smokers. The highest number of smokers was detected in the groups with squamous intraepithelial lesions: 22/43 (51.2%) patients in group 2 (LSIL and HR HPV) and 19/46 (41.3%) patients in group 3 (HSIL and HR HPV) (p<0.001) (Fig. 10). None of the participants of the study abused alcohol or used drugs. A consumption of 30 g or more of pure alcohol per day 2–3 times a week or more often was considered as alcohol abuse.
Hormonal contraception was used by 36/210 (17.1%) patients: 11.37 (29.7%) in group 1 (NILM and HR HPV), 8/43 (18.6%) in group 2 (LSIL and HR HPV), 5/46 (10.9%) in group 3, 4/39 (10.3%) in group 4 (NILM, hyperkeratosis of squamous epithelium, no HPV), 8/45 (17.8%) patients in group 5 (NILM, no HR HPV). The analysis did not detect statistically significant differences between the groups (p=0.148).
Urogenital infections were relatively common in the groups. Herpes simplex virus type 2 was detected in 3/37 (8.1%) patients with NILM and HR HPV, in 9/43 (20.9%) patients with LSIL, in 8/46 (17.4%) patients with HSIL, in 1/39 (5.1%) patient with cervical leukoplakia and in 2/45 (4.4%) patients in the comparison group. Bacterial infections (Micoplasma genitalium, Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis) were found in 25/210 (11.9%) cases, of them combined bacterial and viral infections were detected in 17/25 (68%) cases. Bacterial vaginosis was detected in 42/210 (20%) cases: in 5/37 (13.5%) patients with NILM and HR HPV, in 9/43 (20.9%) patients with LSIL, in 15/46 (32.6%) patients with HSIL, in 9/39 (23.1%) patients with cervical leukoplakia and in 4/45 (8.9%) patients in the comparison group.
Also, correlation between urogenital infections and HR HPV infection was analyzed (Fig. 11). Sexual infections were statistically more common in patients infected with HR HPV (p<0.012).
It should be noted that every third patient with LSIL and HR HPV (37.3%), and in more than half of observed cases, the women with HSIL and HR HPV (58.2%) in history had cervical ectopion for more than 5 years. In this regard, it is logical to assume that the risk of developing precancerous diseases and cervical cancer increases the incomplete process of epithelization of ectopia.
Conclusion
Thus, analysis of the anamnestic data and specific features of the clinical cause of pathological processes in the cervix confirmed once again the significance of certain factors in tumor formation and transformation of cervical epithelial cells. In assessing risk factors for malignancy of cervical diseases, it is necessary to take into account not only the presence of HPV infection, but also the length of time since the primary diagnosis in anamnesis, the age of sexual debut, number of sexual partners, presence of sexually transmitted infections and smoking.
References
- Морхов К.Ю., Нечушкина В.М., Кузнецов В.В. Индукционная химиотерапия местнораспространенного рака шейки матки. Вопросы онкологии. 2015; 61(2): 208-13. [Morkhov K.Y., Nechushkina V.M., Kuznetsov V.V. Induction chemotherapy for locally advanced cervical cancer. Problems in Oncology. 2015; 61(2): 208-13. (in Russian)].
- Lagunas-Martínez A., Madrid-Marina V., Gariglio P. Modulation of apoptosis by early human papillomavirus proteins in cervical cancer. Biochim. Biophys. Acta. 2010; 1805(1): 6-16. https://dx.doi.org/10.1016/j.bbcan.2009.03.005.
- Леваков С.А., Шешукова Н.А., Пауков С.В., Обухова Е.А. Доброкачественные и преинвазивные состояния шейки матки. Учебно-методическое пособие. Практическая медицина; 2022. 63с. [Levakov S.A., Sheshukova N.A., Paukov S.V., Obukhova E.A. Benign and preinvasive conditions of the cervix. Educational and methodological manual. Practical medicine; 2022. 63p.(in Russian)].
- Teixeira N.C.P., Araújo A.C.L., Correa C.M., da Costa Lodi C.T., Lima M.I.M., de Oliveira Carvalho N. et al. Prevalence and risk factors for cervical intraepithelial neoplasia among HIV-infected women. Braz. J. Infec.t Dis. 2012; 16(2): 164-9. https://dx.doi.org/10.1016/s1413-8670(12)70299-4.
- Thorsteinsson K., Ladelund S., Jensen-Fangel S., Katzenstein T.L., Somuncu Johansen I., Pedersen G. et al. Incidence of cervical dysplasia and cervical cancer in women living with HIV in Denmark: Comparison with the general population. HIV Med. 2016; 17(1): 7-17. https://dx.doi.org/10.1111/hiv.12271.
- Fonseca-Moutinho J.A. Smoking and cervical cancer. ISRN Obstet. Gynecol. 2011; 2011: 847684. https://dx.doi.org/10.5402/2011/847684.
- Su B., Qin W., Xue F., Wei X., Guan Q., Jiang W. et al. The relation of passive smoking with cervical cancer: a systematic review and meta-analysis. Medicine (Baltimore). 2018; 97(46): e13061. https://dx.doi.org/10.1097/MD.0000000000013061.
- Sugawara Y., Tsuji I., Mizoue T., Inoue M., Sawada N., Matsuo K. et al.; Research Group for the Development and Evaluation of Cancer Prevention Strategies in Japan. Cigarette smoking and cervical cancer risk: An evaluation based on a systematic review and meta-analysis among Japanese women. Jpn. J. Clin. Oncol. 2019; 49(1): 77-86. https://dx.doi.org/10.1093/jjco/hyy158.
- Dutta T., Haderxhanaj L., Agley J., Jayawardene W., Meyerson B. Association between individual and intimate partner factors and cervical cancer screening in Kenya. Prev. Chronic Dis. 2018; 15: E157. https://dx.doi.org/10.5888/pcd15.180182.
- Endalew D.A., Moti D., Mohammed N., Redi S., Alemu B.W. Knowledge and practice of cervical cancer screening and associated factors among reproductive age group women in districts of Gurage zone, Southern Ethiopia. A cross-sectional study. PLoS One. 2020; 15(9): e0238869. https://dx.doi.org/10.1371/journal.pone.0238869.
- Kaneko N. Factors associated with cervical cancer screening among young unmarried Japanese women: Results from an internet-based survey. BMC Womens Health. 2018; 18(1): 132. https://dx.doi.org/10.1186/s12905-018-0623-z.
- Vanakankovit N., Taneepanichskul S. Effect of oral contraceptives on risk of cervical cancer. J. Med. Assoc. Thai. 2008; 91(1): 7-12.
- La Vecchia C., Boccia S. Oral contraceptives, human papillomavirus and cervical cancer. Eur. J. Cancer Prev. 2014; 23(2): 110-2. https://dx.doi.org/10.1097/CEJ.0000000000000000.
- Bedoya A.M., Tate D.J., Baena A., Córdoba C.M., Borrero Mauricio, Pareja R. et al. Immunosuppression in cervical cancer with special reference to arginase activity. Gynecol. Oncol. 2014; 135(1): 74-80. https://dx.doi.org/10.1016/j.ygyno.2014.07.096.
- Dugué P.-A., Rebolj M., Garred P., Lynge E. Immunosuppression and risk of cervical cancer. Expert Rev. Anticancer Ther. 2013; 13(1): 29-42.https://dx.doi.org/10.1586/era.12.159.
- Clure C., Rivard C. Primary herpes simplex virus infection mimicking a cervical malignancy in an immunocompetent individual. Cureus. 2018; 10(6): e2753. https://dx.doi.org/10.7759/cureus.2753.
- Kenarkoohi A., Bamdad T., Soleimani M., Soleimanjahi H., Fallah A., Falahi S. HSV-TK expressing mesenchymal stem cells exert inhibitory effect on cervical cancer model. Int. J. Mol. Cell. Med. 2020; 9(2): 146-54.https://dx.doi.org/10.22088/IJMCM.BUMS.9.2.146.
- Gadducci A., Barsotti C., Cosio S., Domenici L., Genazzani A.R. Smoking habit, immune suppression, oral contraceptive use, and hormone replacement therapy use and cervical carcinogenesis: a review of the literature. Gynecol. Endocrinol. 2011; 27(8): 597-604. https://dx.doi.org/10.3109/09513590.2011.558953.
- Maseko F.C., Chirwa M.L., Muula A.S. Health systems challenges in cervical cancer prevention program in Malawi. Glob. Health Action. 2015; 8: 26282. https://dx.doi.org/10.3402/gha.v8.26282.
- Murfin J., Irvine F., Meechan-Rogers R., Swift A. Education, income and occupation and their influence on the uptake of cervical cancer prevention strategies: a systematic review. J. Clin. Nurs. 2020; 29(3-4): 393-415.https://dx.doi.org/10.1111/jocn.15094.
- Sundström K., Miriam Elfström K. Advances in cervical cancer prevention: efficacy, effectiveness, elimination? PLoS Med. 2020; 17(1): e1003035.https://dx.doi.org/10.1371/journal.pmed.1003035.
Received 05.04.2023
Accepted 06.09.2023
About the Authors
Sergey A. Levakov, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology of N.V. Sklifosovsky ICM, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), levakoff@yandex.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.Natalia A. Sheshukova, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology of N.V. Sklifosovsky ICM, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), dr.sheshukova@mail.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Elizaveta A. Obukhova, Teaching Assistant at the Department of Obstetrics and Gynecology of N.V. Sklifosovsky ICM, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), liza_obukhova@mail.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Makhluga M. Dzhafarova, graduate student at the Department of Obstetrics and Gynecology of N.V. Sklifosovsky ICM, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), goglu55@mail.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Mariam G. Kaviladze, Teaching Assistant and graduate student at the Department of Obstetrics and Gynecology of N.V. Sklifosovsky ICM, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), mariam-kaviladze@mail.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.