Clinical characteristics of dysmenorrhea and its association with lifestyle factors in adolescent girls
Kriuchkova O.M., Istomina N.G., Baranov A.N.
Dysmenorrhea is the most common pathology among adolescent girls, affecting between 41.7% and 95%, depending on the diagnostic criteria and calculation method used. The multicomponent clinical manifestations, significant impact on quality of life, and potential modifiability of this condition make it not only a medical issue, but also a socially important problem.
Objective: To investigate the prevalence of dysmenorrhea among adolescent girls aged 15–19 years, as well as its symptoms, menstrual function characteristics, and impact on behavioral characteristics, physical activity, and quality of life, depending on the severity of the pain syndrome.
Materials and methods: A cross-sectional study was conducted at outpatient healthcare facilities in Arkhangelsk by surveying 585 healthy teenage girls aged 15–19 years who met the inclusion criteria, followed by a comparative statistical analysis.
Results: The prevalence of dysmenorrhea in our study was 97%. Clinical parameters of menstrual function were comparable between girls with painless and painful menstruation, suggesting that menstrual cycle characteristics alone are insufficient to fully assess dysmenorrhea. More than half of the teenage girls (52.9%) rated the severity of the pain as moderate, while approximately a quarter (24.9%) rated it as severe. Severe forms of dysmenorrhea were characterized by more widespread localization of pain. Dysmenorrhea included a wide range of “non-gynecological” symptoms, the frequency and severity of which correlated with the intensity of pain. It also had a significant negative impact on various aspects of life for the vast majority (up to 79.7%) of adolescent girls, including decreased academic performance, difficulties with homework, absenteeism, concentration problems, and limited social and physical activity. These findings are consistent with data from similar studies, and emphasize the importance of an integrated diagnostic approach for this condition.
Conclusion: The wide prevalence of dysmenorrhea and the lack of other symptoms in standard gynecological evaluations can normalize the condition and hinder a realistic assessment, potentially worsening both the medical and social prognosis. Given the specificity of the condition and the subjectivity of its clinical manifestations, careful development of objective tools for assessing the severity of dysmenorrhea is essential.
Authors' contributions: Kriuchkova O.M. – conception and design of the study, data collection, statistical analysis, drafting of the manuscript; Istomina N.G. – literature review, analysis, drafting of the manuscript; Baranov A.N. – design of the study, final editing. All authors confirm that their authorship meets the international ICMJE criteria (all authors have made a substantial contribution to the design, conduct of the study and writing of the article, and have read and approved the final version before submission).
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Kriuchkova O.M., Istomina N.G., Baranov A.N.
Clinical characteristics of dysmenorrhea and its association with lifestyle factors in adolescent girls.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (12): 94-107 (in Russian)
https://dx.doi.org/10.18565/aig.2024.207
Keywords
Adolescence is a critical stage in a person’s life, during which the principles of a healthy lifestyle are often formed, and specific behavioral characteristics are established that can significantly impact reproductive health [1]. Some of these characteristics, related to social, behavioral, and medical aspects, are potentially modifiable and can be of great importance to public health [1–8]. The menstrual cycle is considered the main integrated indicator of the functioning of the female reproductive system; thus, the assessment of menstrual function in adolescents has special significance [9–15].
It is well known that menstrual cycle disorders in adolescent girls are prominent in gynecological pathology, including uterine bleeding (20–30%) and amenorrhea (3.3–11%). However, according to numerous researchers, the most common issue in this age group is dysmenorrhea, affecting up to 90% of adolescents [15–19].
Dysmenorrhea is categorized into primary and secondary types. Primary dysmenorrhea is defined by most authors as a syndrome of cyclic pain, often accompanied by a complex of emotional-psychic, vegetative, vascular, and metabolic-endocrine symptoms, in the absence of obvious gynecological pathology. In contrast, secondary dysmenorrhea is a pain syndrome caused by the presence of chronic gynecological diseases, which are more common in women of middle and late reproductive age, or by anomalies in the development of the genitals [20–23]. Primary dysmenorrhea is most common among adolescents, and its widespread prevalence has several important consequences. First, many girls do not seek gynecological care for painful or irregular periods, considering them normal, compounded by the low alertness of gynecologists for the same reason. Second, there are "non-gynecological" complaints associated with menstrual pain that often remain outside the attention of gynecologists. However, numerous studies have demonstrated a direct link between the severity of dysmenorrhea symptoms and symptoms across the neurological, psychological, and metabolic-endocrine spectrum as well as various aspects of the lifestyle of adolescent girls [24–27].
All these factors contribute to the normalization of dysmenorrhea symptoms among most adolescents, leading them to use ineffective symptomatic therapy or refuse treatment altogether. This trend negatively affects quality of life, reduces personal and social activity, impacts emotional well-being, and may lead to a late diagnosis of secondary dysmenorrhea and a decrease in reproductive potential [28–30].
This study aimed to investigate the prevalence of dysmenorrhea among adolescent girls aged 15–19 years, as well as its symptoms, menstrual function characteristics, and impact on behavioral characteristics, physical activity, and quality of life, depending on the severity of the pain syndrome.
Materials and methods
The results of the study are presented in accordance with the STROBE guidelines for observational studies [31].
This cross-sectional study was conducted at randomly selected outpatient healthcare facilities in Arkhangelsk. Data were collected from January to April 2023 using anonymous questionnaires. The study participants consisted of a random sample of adolescent girls aged 15–19 years who lived in Arkhangelsk, agreed to participate in the study, and did not have established gynecological diseases.
The questionnaire was pretested to assess the clarity and comprehensibility of the questions, which were then adjusted for use with the main sample of respondents. A total of 620 questionnaires were collected; however, 15 were excluded due to the absence of menstruation and 10 were excluded due to incomplete responses.
The questionnaire consisted of four blocks of questions:
- The first block included demographic, anthropometric, and social characteristics (age, weight, and height).
- The second block focused on the behavioral characteristics of the respondents (bad habits, dietary habits, sleep duration, and physical activity).
- The third block included questions that assessed menstrual characteristics.
- The fourth block addressed pain syndrome, additional symptoms, the need for medication, and history of seeking medical care.
The standard deviation of body mass index (SDS BMI) was used to diagnose overweight and obesity among adolescents. According to federal clinical guidelines developed using the World Health Organization (WHO) recommendations, obesity in children and adolescents aged 0–19 years is defined as a BMI value equal to or greater than +2.0 SDS BMI. Overweight was diagnosed in the range of +1.0 to +2.0 SDS BMI, while normal weight was defined as BMI values within ±1.0 SDS BMI [32, 33].
Each girl's BMI was calculated. BMI is defined as weight divided by the square of height. The resulting values were assessed using normative tables recommended by the WHO [34].
The age at menarche was determined retrospectively, and gynecological age was calculated as the difference between the current age of the respondent and the onset of menstruation.
The volume of bleeding during menstruation was measured using the pictorial blood loss assessment chart (PBAC), which considers the duration of blood loss exceeding eight days, expulsion of clots, and estimated volume of blood loss. According to the FIGO criteria, blood loss was categorized as heavy (> 80 ml), moderate (5-80 ml), or scant (less than 5 ml) [11, 35].
To assess dysmenorrhea, all girls who reported pain of varying intensity during menstruation were included in the corresponding group. The severity of dysmenorrhea was measured using a numerical rating scale: scores from 1 to 3 were classified as mild, 4 to 7 as moderate, and >8 as severe [36, 37].
To evaluate additional neurovegetative symptoms associated with menstruation, girls were asked to indicate the presence of symptoms from a supplementary list of the most common criteria [38–40].
Physical activity was assessed using the International Physical Activity Questionnaire (IPAQ) [41]. The results (scores) were interpreted as follows: hypodynamia, <21 points; and optimal physical activity, ≥ 28 points [42].
Statistical analysis
Statistical analysis was conducted using STATA 14.2 Windows. Given the large number of respondents, the normality of the distribution within the group was tested using the Kolmogorov–Smirnov test with Lilliefors correction. Continuous variables with abnormal distributions are presented as the median (Me) along with the first and third quartiles (Q1 and Q3). Continuous variables between the study groups were compared using the parametric Student's t-test for independent samples and nonparametric Mann–Whitney test. The Kruskal–Wallis test was used to compare the numerical data between three or more groups. Categorical variables were analyzed using Pearson’s χ2 test. The level of statistical significance was set at p≤0.05. Criteria that showed statistically significant differences in the multi-way tables were compared pairwise using Bonferroni correction.
Results
General description of the study group
A total of 585 girls aged 15–19 years participated in this study. According to the data presented, most of the examined girls (n=184) were in the 15-year age group (31.4%). This distribution may be due to the fact that extended preventive examinations are performed at this age. The remaining age groups were represented by almost equal numbers of participants (Fig. 1). The median age (Me) in our study was 16.0 years, with the lower (Q1) and upper (Q3) quartiles being 15.0 and 18.0 years, respectively.
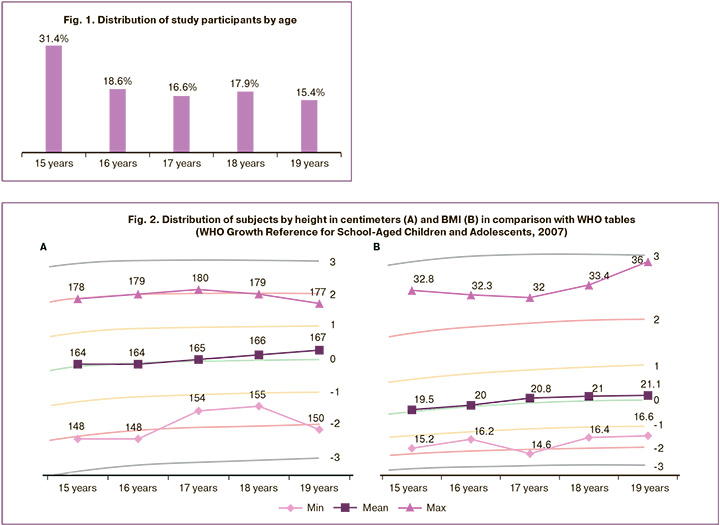
The distribution of the main anthropometric data of the study participants—height and BMI—corresponded to the WHO age centile tables (Fig. 2). The medians of these indicators in all age subgroups reflect the average age indicators. Girls’ weight values were not compared with centile tables because of the absence of recommended reference values for body weight in relation to age [43].
The age at menarche (Me (Q1; Q3)) of the adolescents in our study was 12.5 (12; 13) years. Notably, in 557/585 (95.2%) cases, this indicator ranged from 10 to 15 years old. Early onset of menarche (before 10 years) was noted in 3/585 (0.5%) girls, whereas late menarche (15 years and older) occurred in 25/585 (4.3%) girls.
The gynecological age (Me (Q1; Q3)) in the study group was 4 (3; 5). Data on the median gynecological age and its minimum and maximum values in the different age groups are presented in Figure 3.
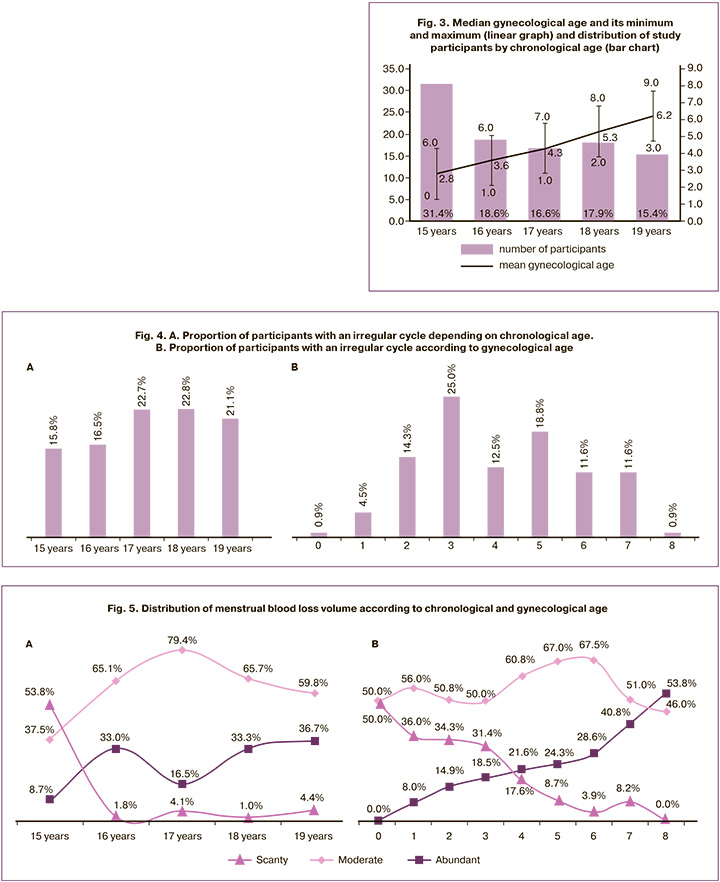
A regular menstrual cycle was observed in 473/585 (80.9%) respondents; in 307/585 (64.9%), it was established within the first 12 months; and in 166/585 (35.1%) – within one year after menarche, but all were established within 24 months. Almost every fifth (19.1%) of the girls in the study noted that they currently have an irregular cycle. When analyzing the distribution of this indicator based on chronological and gynecological age (Fig. 4, bar graphs), we did not find a specific pattern, except that the frequency of irregular cycles increased with the respondents' age and during the first three years following menarche. We have not yet found an explanation for this phenomenon in the available literature and we plan to study this indicator in more detail in the future. However, the overall prevalence of irregular cycles in adolescents in our study was consistent with findings from other researchers [44–46].
Of the girls who reported having a regular cycle, 364/473 (77%) had a menstrual cycle duration of 21–30 days, which aligns with the age norms from similar population studies [44–46].
Analysis of the survey results regarding the duration of menstrual bleeding showed that nearly all participants, 582/585 (99.5%), noted that it ranged from 3 to 8 days. The estimated volume of menstrual bleeding was classified as moderate for more than half of the respondents: 339/585 (58%), heavy for 136/585 (23.2%), and scant for 110/585 (18.8%). The distribution of menstrual blood loss volume according to chronological and gynecological ages is shown in Figure 5. Our data indicated a correlation between the abundance of menstruation and age; as gynecological age increased, the percentage of heavy menstruation increased, while the frequency of scanty discharge decreased.
When assessing the relationship between the amount of blood loss and cycle duration in girls with an irregular cycle, the frequency of heavy and scanty menstruation was higher than expected (25% vs. 22.8% for heavy, and 22.3% vs. 18% for scanty, between irregular and regular cycles, respectively), but this difference was not statistically significant.
Thus, the adolescent girls who participated in our study exhibited a standard distribution of anthropometric features, a timely onset of menarche, and normal menstrual cycle parameters in the vast majority (over 80 %).
In analyzing the pain syndrome accompanying menstruation, only 16/585 (3%) girls reported that it was absent. The remaining 569/585 (97%) participants were categorized into three subgroups based on their self-assessment of pain intensity using a rating scale: weak degree of pain syndrome, 126 (22.2%); moderate, 300 (52.9%); and strong, 143 (24.9%). The data are shown in Figure 6.
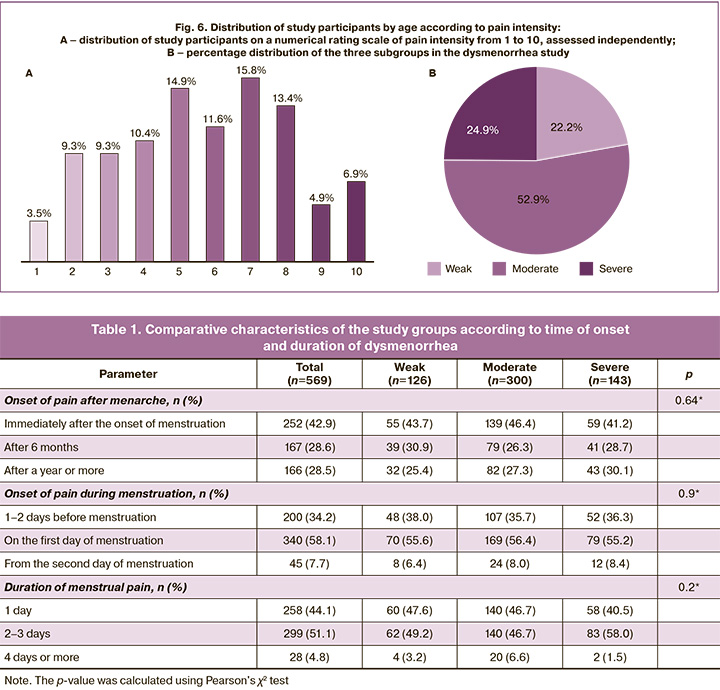
More than 70% of the respondents reported the onset of pain associated with menstruation during the first year after menarche, with 42.9% experiencing it immediately after the onset of menstruation. When analyzing the intensity of dysmenorrhea by age (Fig. 7), we observed a trend toward an increase in the proportion of girls who rated their pain as severe, along with a decrease in the percentage of those who rated it as mild, as both chronological age and, more noticeably, gynecological age increased. Additionally, the distribution by gynecological age revealed a decrease in the proportion of girls without dysmenorrhea.
More than half of the teenage girls, 331/569 (58.1%), began to experience pain on the first day of menstruation, and in 95.2% of cases, it lasted from 1 to 3 days. Statistical analysis within the groups with different pain intensities did not reveal any significant differences (p>0.05). The data are presented in Table 1.
Only half – 307/569 (53.9%) – of the teenagers with dysmenorrhea surveyed reported that the pain was localized to the lower abdomen. Many girls noted three additional areas of pain associated with menstruation: the groin, lumbar region, and lower extremities. Figure 8 illustrates the distribution of pain locations in various combinations. The most frequent secondary location of pain was the lumbar region, which was reported by more than one-third (35%) of the respondents.
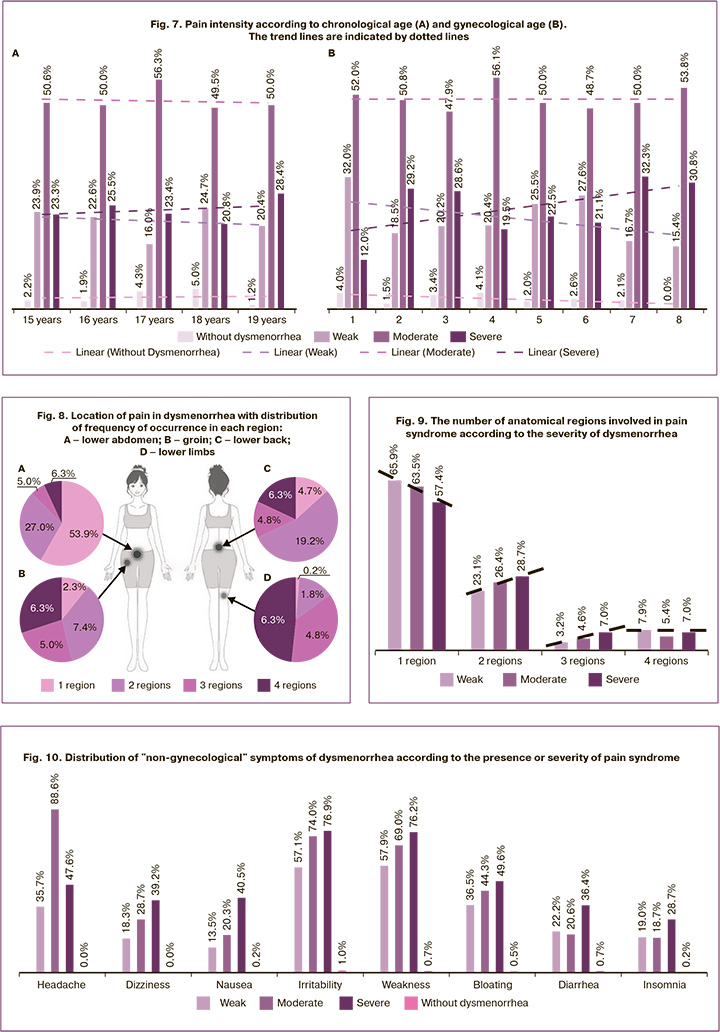
In our study, the severity of pain syndrome and the number of involved regions were associated with an increase in pain intensity to moderate and severe levels. The proportion of patients with one localized area decreased (63.5% to 57.4%), whereas the percentage of girls experiencing pain in two (23.1% to 28.7%), three (3.2% to 7.0%), and four (7.9% to 7.0%) regions increased (Fig. 9).
In the subsequent analysis of the anthropometric parameters of the study participants (Table 2), we observed a lower percentage of girls with dysmenorrhea who had a normal BMI than those without dysmenorrhea. Underweight in the dysmenorrhea group (21.8% vs. 12.5% in the group without dysmenorrhea), as were overweight or obese participants (12.6% vs. 6.2% without dysmenorrhea). However, in our study, these differences were not statistically significant (p>0.05).
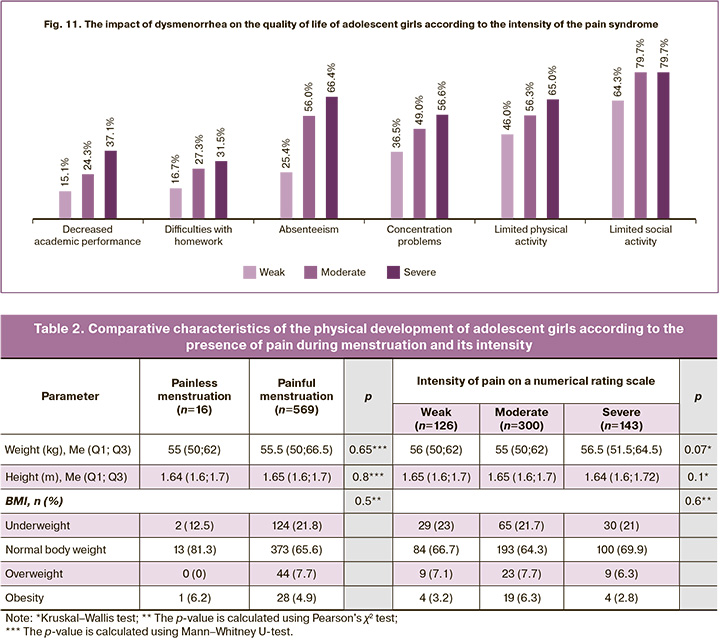
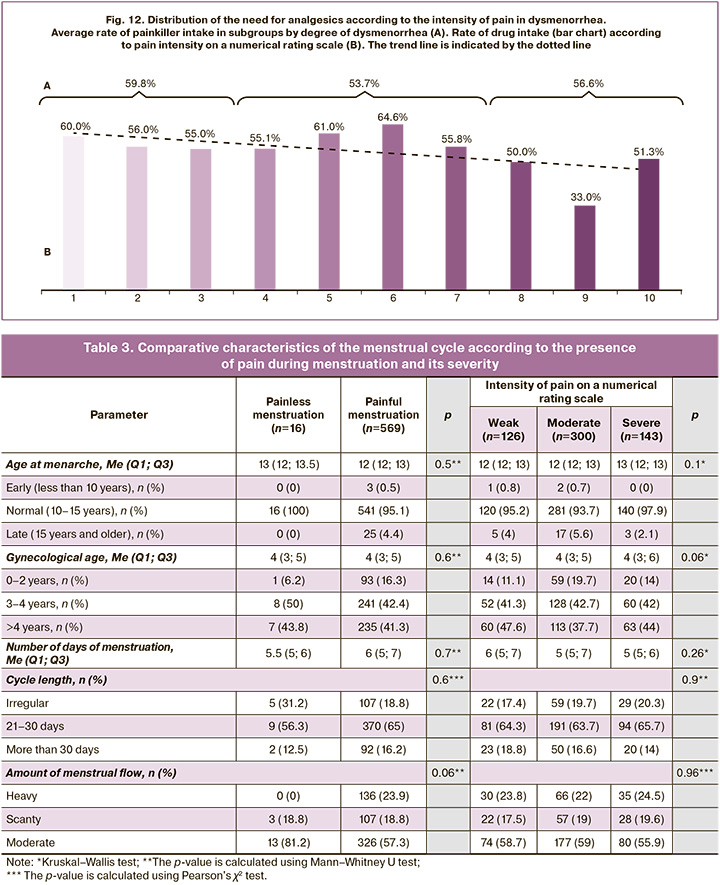
When examining the menstrual cycle parameters in the study and control groups, we found that adolescents with dysmenorrhea were more likely to experience regular cycles and heavier menstrual blood loss. However, overall, these findings did not reach statistical significance (p>0.05) and did not demonstrate clear trends based on pain intensity (Table 3).
The most informative part of the questionnaire for the study of dysmenorrhea was the section in which respondents were asked about the presence of "non-gynecological" symptoms accompanying dysmenorrhea (Fig. 10). Adolescents with dysmenorrhea most frequently reported experiencing symptoms, such as headaches – 504/569 (88.6%), irritability – 421/569 (74.0%), weakness – 393/569 (69.0%), and bloating – 252/569 (44.3%). In almost all cases (except for headaches, diarrhea, and insomnia), the maximum values were observed in the group with high pain intensity. These results highlight the importance of considering concomitant symptoms when diagnosing dysmenorrhea.
Similarly, girls with dysmenorrhea responded to questionnaire questions regarding their quality of life, including their social and physical activities; the distribution of these indicators is shown in Figure 11.
As pain intensity increased from mild to severe, there was a significant increase in the proportion of adolescents reporting declines in academic performance, difficulty concentrating, and missed classes on menstrual days (up to 66.4%). However, the most notable limitations for girls with dysmenorrhea were observed in the areas of social interaction (in terms of meetings and outings with friends) (46.0–65.0%) and physical activity (64.3–79.7%).
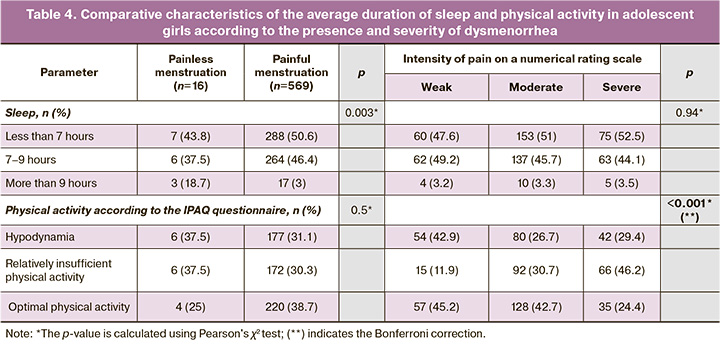
We further investigated the duration of sleep and parameters of physical activity in these subgroups; the results are presented in Table 4.
Self-assessment of the average sleep duration revealed that almost half of the adolescents participating in our study had a sleep deficit. For adolescents with dysmenorrhea, an increase in the proportion of girls with insufficient sleep duration (less than 7 h per day) correlated with the intensity of pain, showing statistically significant differences (p<0.05). When assessing physical activity using the IPAQ questionnaire, we identified a general trend towards insufficient physical activity in both the study and control groups. However, girls with dysmenorrhea exhibited higher rates of insufficient physical activity and lower rates of optimal physical activity, with both factors correlating with pain syndrome severity. Statistically significant differences in pain intensity were observed (p<0.05), and the Bonferroni test indicated statistically significant differences between the groups experiencing moderate and severe pain (p=0.040). At present, we find it difficult to determine the cause-and-effect relationship between decreased physical activity and the severity of dysmenorrhea, as this issue, in our opinion, requires consideration of a larger number of objective factors.
We obtained interesting data when studying the need for medications to relieve dysmenorrhea among study participants. More than half (304 participants, 53.4%) of girls with dysmenorrhea reported taking painkillers during menstruation. Interestingly, the distribution of medication use based on pain intensity was the opposite, as adolescents with minimal pain intensity reported using medications more often than those with high pain intensity (Fig. 12). This form of questioning does not allow for a complete evaluation of information, and future studies will need to focus more on assessing pain without the use of painkillers. It will also be essential to include a scale for assessing the effectiveness of pain relief in the questionnaires and to ask about the reasons for girls' refusal of painkillers.
Discussion
Main results
In our study, the prevalence of dysmenorrhea, which is defined as painful menstruation, was 97%. The clinical parameters of menstrual function that we assessed were comparable between the girls with painless and painful menstruation.
More than half of the girls with dysmenorrhea we surveyed (52.9%) rated the severity of their pain as moderate, while approximately a quarter (24.9%) rated it as severe. Severe forms of dysmenorrhea were characterized by more widespread pain localization and a high frequency of "non-gynecological" symptoms, such as headache, irritability, general weakness, and nausea. The severity of these symptoms is correlated with the intensity of the pain syndrome.
Additionally, painful sensations significantly impact the quality of life of adolescent girls during menstruation, primarily due to forced limitations in social, academic, and physical activities. This included a decrease in academic performance (up to 37.1%), missed classes (up to 66.4%), concentration problems (up to 56.6%), social limitations (up to 66.5%), and physical activity (up to 79.7%). These findings are consistent with data from similar studies, and emphasize the importance of an integrated approach for diagnosing this condition.
Main limitations of the study
- The use of questionnaires for data collection may introduce subjectivity in the assessment of dysmenorrhea symptoms, particularly pain intensity.
- There are no generally accepted objective methods for diagnosing dysmenorrhea.
- Responses may be biased because of social desirability.
- The sample was limited to one city (Arkhangelsk), which may reduce the generalizability of the results to a broader population of adolescent girls.
Interpretation of the study results
The findings of this study align with those of other researchers who estimate the prevalence of dysmenorrhea among adolescent girls to be between 41.7% and 95%, depending on the diagnostic criteria and calculation methods [47, 48] used. The high prevalence of dysmenorrhea identified in our study confirms that this condition is one of the most pressing issues in adolescent gynecology.
The clinical parameters of the menstrual cycle in girls with pronounced symptoms of dysmenorrhea did not generally differ from the data of other population studies [44–46]. This indicates that assessing menstrual cycle parameters alone is insufficient for complete evaluation of dysmenorrhea severity. It is particularly important to note that severe forms of dysmenorrhea are characterized by more pronounced "non-gynecological" symptoms and a significant negative impact on various areas of adolescent girls' lives.
Currently, there is no widely accepted classification or definition for primary dysmenorrhea. However, the widespread prevalence of this potentially manageable condition makes it not only a medical but also a socially significant problem. Unfortunately, these factors lead to a situation in which the assessment of dysmenorrhea during short preventive examinations by gynecologists typically focuses on normalizing the condition. Adolescents often perceive pain as an inevitable symptom of menstruation. The authors believe that the development of a special questionnaire and preparation of informational materials can help address this issue. We believe that an important first step is to bring attention to the decreased social activity associated with dysmenorrhea, including academic performance, in most adolescent girls. This limitation affects their personal and professional potential, in addition to worsening their medical prognosis and impacting their reproductive futures.
An important but insufficiently studied aspect is the assessment of clinical components of dysmenorrhea from the perspective of potentially modifiable conditions. The most accessible methods for addressing dysmenorrhea include drug and non-drug pain relief, normalization of daily routines, and increased physical activity. The design of such a study should differentiate between the features of objective and subjective assessments of pain syndromes and the effectiveness of pain relief methods, and should also consider additional factors, such as overall anxiety levels and lifestyle.
External validity
The results of this study, conducted on a representative sample of teenage girls in Arkhangelsk, can generally be extrapolated to the population of teenage girls in Russia. This is because of the comparable prevalence of dysmenorrhea, its clinical manifestations, and its impact on various aspects of adolescents' lives, as indicated by other domestic and foreign studies.
At the same time, it should be considered that the socio-economic, cultural, and climatic-geographical features of different regions can impact the course and manifestation of dysmenorrhea in teenage girls. Therefore, additional studies that cover various regions of the Russian Federation are needed to achieve a more comprehensive assessment of the situation in the country.
Conclusions
- Dysmenorrhea is a condition common among the vast majority of adolescents.
- The assessment of menstrual function parameters does not provide a complete picture of the severity of dysmenorrhea; parameters related to pain syndrome (intensity, localization, use of various pain relief methods, their effectiveness, etc.) require further study and standardization.
- The evaluation of dysmenorrhea should include vegetative symptoms typical of most adolescents as well as indicators of limitations in social and physical activity, for which there are currently no generally accepted measurement tools.
- It is essential to develop objective criteria for assessing the severity of dysmenorrhea.
References
- Уварова Е.В., Коломейцев М.Г., Радченко М.В. Правовые аспекты охраны репродуктивного здоровья несовершеннолетних по профилю "акушерство и гинекология" в Российской Федерации. Репродуктивное здоровье детей и подростков. 2022; 18(1): 16-33. [Uvarova E.V., Kolomeitsev M.G., Radchenko M.V. Legal aspects of the protection of the reproductive health of minors in the profile «obstetrics and gynecology» in the Russian Federation. Pediatric and Adolescent Reproductive Health. 2022; 18(1): 16-33. (in Russian)]. https://dx.doi.org/10.33029/1816-2134-2022-18-1-16-33.
- Стародубов В.И., Леонов С.А., Савина А.А., Фейгинова С.И., Алексеева В.М.,Зимина Э.В. Тенденции показателей общей заболеваемости населения в субъектах Центрального федерального округа Российской Федерации. Проблемы социальной гигиены, здравоохранения и истории медицины. 2019; 27(6): 947-52. [Starodubov V.I., Leonov S.A., Savina A.A., Feiginova S.I., Alekseeva V.M., Zimina E.V. The trends of population general morbidity in the subjects of the Central Federal Okrug of the Russian Federation. Problemi socialnoi gigieni, zdravookhranenia i istorii meditsini.. 2019; 27(6): 947-52. (in Russian)]. https://dx.doi.org/10.32687/0869-866X-2019-27-6-947-952.
- Радзинский В.Е., Хамошина М.Б., Лебедева М.Г., Архипова М.П., Руднева О.Д., Чакчурина И.А. Девушки-подростки РФ: современные тенденции формирования репродуктивного потенциала (обзор литературы). Сибирский медицинский журнал. 2010; 25(4-2): 9-14. [Radzinsky V.E., Khamoshina M.B., Lebedeva M.G., Arkhipova M.P., Rudneva O.D., Chakchurina I.A. Adolescent girls in Russia: contemporary trends of reproductive potential formation. Siberian Medical Journal. 2010; 25(4-2): 9-14. (in Russian)].
- Баранов А.А., Альбицкий В.Ю. Состояние здоровья детей России, приоритеты его сохранения и укрепления. Казанский медицинский журнал. 2018; 99(4): 698-705. [Baranov A.A., Albitskiy V.Yu. State of health of children in Russia, priorities of its preservation and improving. Kazan Medical Journal. 2018; 99(4): 698-705. (in Russian)]. https://dx.doi.org/10.17816/KMJ2018-698.
- Султанаева З.М., Шарафутдинова Н.Х. Заболеваемость в детском и подростковом возрасте как фактор формирования репродуктивного здоровья. Здравоохранение Российской Федерации. 2010; 2: 22-5. [Sultanaeva Z.M., Sharafutdinova N.Kh. Morbidity in puerile and adolescent age as factor in reproductive health being emerged. Zdravookhranenie RossiiskoiFederatsii. 2010; (2): 22-5. (in Russian)].
- Курбатова С.П., Пенькова П.К. Поведенческие факторы риска нарушения репродуктивного здоровья. В кн.: Научная сессия ПГМУ им. академика Е.А. Вагнера. Материалы научно-практической конференции с международным участием студентов, ординаторов, аспирантов, молодых ученых (до 35 лет), Пермь, 19-20 апреля 2023 г. Том 1. Пермь: Пермский национальный исследовательский политехнический университет; 2023: 307-10. [Kurbatova S.P., Pen’kova P.K. Behavioral risk factors for reproductive health disorders. In: Scientific session of Perm State Medical University named after Academician E.A. Wagner. Materials of the scientific and practical conference with international participation of students, residents, graduate students, young scientists (up to 35 years old), Perm, April 19-20, 2023. Vol. 1. Perm: Perm National Research Polytechnic University; 2023: 307-10.(in Russian)].
- Хащенко Е.П., Суханова Ю.А., Пятаева С.В., Володина М.А., Тарасова Н.В., Цвиркун Д.В., Уварова Е.В., Высоких М.Ю. Показатели митохондриального функционирования у девочек-подростков с синдромом поликистозных яичников с учетом наличия метаболических нарушений и избыточного веса. Акушерство и гинекология. 2017; 7: 104-13. [Khashchenko E.P., Sukhanova Yu.A., Pyataeva S.V., Volodina M.A., Tarasova N.V., Tsvirkun D.V., Uvarova E.V., Vysokikh M.Yu. Indicators of mitochondrial functioning in adolescent girls with polycystic ovary syndrome with regard to the presence of metabolic disorders and overweight. Obstetrics and Gynecology. 2017; (7): 104-13. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.7.104-13.
- Барегамян Г.Г., Барсегян А.А., Бегларян Г.А. Состояние репродуктивного здоровья девочек-подростков. Акушерство и гинекология. 2021; 8: 166-74. [Baregamyan G.G., Barsegyan A.A., Beglaryan G.A.The state of adolescent girls' reproductive health. Obstetrics and Gynecology. 2021; (8): 166-74. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.8.166-174.
- Муяссарова М.М., Абдурашитова Ш.А. Состояния репродуктивного здоровья женщин и основные факторы. European Journal of Interdisciplinary Research and Development. 2023; 19(0): 8-11. [Muyassarova M.M., Abdurashitova Sh.A. Women's reproductive health conditions and main factors. European Journal of Interdisciplinary Research and Development. 2023; 19(0): 8-11. (in Russian)]. Available at: http://ejird.journalspark.org/index.php/ejird/article/view/763
- Уварова Е.В. Проблема репродуктивного потенциала современных детей и подростков стоит остро. Эффективная фармакотерапия. 2019; 15(26): 6-7. [Uvarova E.V. The problem of the reproductive potential of modern children and adolescents is acute. Effective Pharmacotherapy. 2019; 15(26): 6-7.(in Russian)].
- Munro M.G., Critchley H.O.D., Fraser I.S.; FIGO Menstrual Disorders Committee. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int. J. Gynaecol. Obstet. 2018; 143(3):393-408. https://dx.doi.org/10.1002/ijgo.12666.
- ACOG Committee Opinion No. 651: menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Obstet. Gynecol. 2015; 126(6): e143-e146. https://dx.doi.org/10.1097/AOG.0000000000001215.
- Harley K.G., Watson A., Robertson S., Vitzthum V.J., Shea A. Menstrual cycle characteristics of U.S. adolescents according to gynecologic age and age at menarche. J. Pediatr. Adolesc. Gynecol. 2024; 37(4): 419-25.https://dx.doi.org/10.1016/j.jpag.2024.03.005.
- American Academy of Pediatrics Committee on Adolescence, American College of Obstetricians and Gynecologists Committee on Adolescent Health Care; Diaz A., Laufer M.R., Breech L.L. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics. 2006; 118(5): 2245-50.https://dx.doi.org/10.1542/peds.2006-2481.
- World Health Organization multicenter study on menstrual and ovulatory patterns in adolescent girls. II. Longitudinal study of menstrual patterns in the early postmenarcheal period, duration of bleeding episodes and menstrual cycles. World Health Organization Task Force on Adolescent Reproductive Health. J. Adolesc. Health Care. 1986; 7(4): 236-44.
- Клинические рекомендации (проект). Аномальные маточные кровотечения в пубертатном периоде. Репродуктивное здоровье детей и подростков. 2021; 17(3): 5-30. [Clinical guidelines (project). Abnormal uterine bleeding during puberty. Pediatric and Adolescent Reproductive Health. 2021; 17(3): 5-30. (in Russian)]. https://dx.doi.org/10.33029/1816-2134-2021-17-3-5-30.
- Barbosa-Silva J., Avila M.A., de Oliveira R.F., Dedicação A.C., Godoy A.G., Rodrigues J.C. et al. Prevalence, pain intensity and symptoms associated with primary dysmenorrhea: a cross-sectional study. BMC Womens Health. 2024; 24(1): 92. https://dx.doi.org/10.1186/s12905-023-02878-z.
- Адамян Л.В., Сибирская Е.В., Пивазян Л.Г., Аветисян Д.С., Лаевская А.А., Мурватова С.К. Первичная аменорея: этиология, методы диагностики и лечение. Эффективная фармакотерапия. 2023; 19(44): 50-7. [Adamyan L.V., Sibirskaya E.V., Pivazyan L.G., Avetisyan D.S., Laevskaya A.A., Murvatova S.K. Primary amenorrhea: etiology, diagnosis and treatment. Effective Pharmacotherapy. 2023; 19(44): 50-7. (in Russian)].https://dx.doi.org/10.33978/2307-3586-2023-19-44-50-57.
- Momma R., Nakata Y., Sawai A., Takeda M., Natsui H., Mukai N. et al. Comparisons of the prevalence, severity, and risk factors of dysmenorrhea between Japanese female athletes and non-athletes in Universities. Int. J. Environ. Res. Public Health. 2021; 19(1): 52. https://dx.doi.org/10.3390/ijerph19010052.
- Hashim R.T., Alkhalifah S.S., Alsalman A.A., Alfaris D.M., Alhussaini M.A., Qasim R.S. et al. Prevalence of primary dysmenorrhea and its effect on the quality of life amongst female medical students at King Saud University, Riyadh, Saudi Arabia. A cross-sectional study. Saudi Med. J. 2020; 41(3): 283-9.https://dx.doi.org/10.15537/smj.2020.3.24988.
- Hu Z., Tang L., Chen L., Kaminga A.C., Xu H. Prevalence and risk factors associated with primary dysmenorrhea among Chinese female university students: a cross-sectional study. J. Pediatr. Adolesc. Gynecol. 2020; 33(1): 15-22. https://dx.doi.org/10.1016/j.jpag.2019.09.004.
- Chen L., Tang L., Guo S., Kaminga A.C., Xu H. Primary dysmenorrhea and self-care strategies among Chinese college girls: a cross-sectional study. BMJ Open. 2019; 9(9): e026813. https://dx.doi.org/10.1136/bmjopen-2018-026813.
- Nyirenda T., Nyagumbo E., Murewanhema G., Mukonowenzou N., Kagodora S.B., Mapfumo C. et al. Prevalence of dysmenorrhea and associated risk factors among university students in Zimbabwe. Womens Health (Lond.). 2023; 19: 17455057231189549. https://dx.doi.org/10.1177/17455057231189549.
- Durand H., Monahan K., McGuire B.E. Prevalence and impact of dysmenorrhea among university students in Ireland. Pain Med. 2021; 22(12): 2835-45. https://dx.doi.org/10.1093/pm/pnab122.
- Сергеева С.П., Александров Л.С. Тревога, депрессия и вегетативные нарушения у женщин с дисменореей. Российский журнал боли. 2017; 1: 80-1. [Sergeeva S.P., Aleksandrov L.S. Anxiety, depression, and autonomic disorders in women with dysmenorrhea. Rossiiskii Zhurnal Boli. 2017; (1): 80-1.(in Russian)].
- Филиппова И.Л. Психосоматические предпосылки болевого синдрома при дисменорее. В кн.: Мечниковские чтения-2022. Материалы 95-й Всероссийской научно-практической студенческой конференции с международным участием, Санкт-Петербург, 28 апреля 2022 г. Часть I. Санкт-Петербург: Северо-Западный государственный медицинский университет имени И.И. Мечникова; 2022: 38-9. [Filippova I.L. Psychosomatic prerequisites for pain syndrome in dysmenorrhea. In: Mechnikov readings-2022. Materials of the 95th All-Russian scientific and practical student conference with international participation, St. Petersburg, April 28, 2022. Part I. St. Petersburg: Northwestern State Medical University named after I.I. Mechnikov; 2022: 38-9. (in Russian)].
- Попова А.С., Клаучек С.В., Фокина А.С., Барулин Л.А. Дифференцирующие характеристики эмоционально-поведенческой сферы у молодых женщин с первичной дисменореей. В кн.: Физиология - актуальные проблемы фундаментальных и прикладных исследовании. Материалы Всероссийской с международным участием научно-практической конференции, посвященной 125-летию со дня рождения академика Петра Кузьмича Анохина, Волгоград, 16-17 мая 2023 г. Волгоградский государственный медицинский университет; 2023: 145-7. [Popova A.S., Klauchek S.V., Fokina A.S., Barulin L.A. Differentiating characteristics of the emotional-behavioral sphere in young women with primary dysmenorrhea. In: Physiology - current problems of fundamental and applied research. Materials of the All-Russian international participation in a scientific and practical conference dedicated to the 125th anniversary of the birth of academician Petr Kuzmich Anokhin, Volgograd, May 16-17, 2023. Volgograd State Medical University; 2023: 145-7.(in Russian)].
- Попова А.С. Психосоматические исследования в современной медицине на материале ранней дисменореи. Гуманитарные проблемы медицины и здравоохранения. 2023; 1(2): 53-60. [Popova A.S. Psychosomatic research in modern medicine based on the material of early dysmenorrhea. Humanitarian Problems of Medicine and Healthcare. 2023; 1(2): 53-60.(in Russian)].
- Becker C.M., Bokor A., Heikinheimo O., Horne A., Jansen F., Kiesel L. et al.; ESHRE Endometriosis Guideline Group. ESHRE guideline: endometriosis. Hum. Reprod. Open. 2022; 2022(2): hoac009. https://dx.doi.org/10.1093/hropen/hoac009.
- Муфтайдинова Ш.К., Муминова З.А., Абдуллажонова М.У. Эндометриоз у девочек-подростков. Мodels and methods for increasing the efficiency of innovative research. ISOC. 2023; 2(20): 100-1. [Muftaidinova Sh.K., Muminova Z.A., Abdullazhonova M.U. Endometriosis in adolescent girls. Models and Methods for Increasing the Efficiency of Innovative Research. ISOC. 2023; 2(20): 100-1. (in Russian)].
- Vandenbroucke J.P., von Elm E., Altman D.G., Gøtzsche P.C., Mulrow C.D., Pocock S.J. et al.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int. J. Surg. 2014; 12(12): 1500-24. https://dx.doi.org/10.1016/j.ijsu.2014.07.014.
- Дедов И.И., Петеркова В.А., ред. Федеральные клинические рекомендации (протоколы) по ведению детей с эндокринными заболеваниями. М.: Практика; 2014. 442с. [Dedov I.I., Peterkova V.A., eds. Federal clinical guidelines (protocols) for the management of children with endocrine diseases. Moscow: Praktika; 2014. 442p. (in Russian)].
- Российская ассоциация эндокринологов. Оценка физического развития детей и подростков. Методические рекомендации. М.; 2017. 98c. [Russian Association of Endocrinologists. Assessing the physical development of children and adolescents. Guidelines. Moscow; 2017. 98p.(in Russian)].
- De Onis M., Onyango A.W., Borghi E., Siyam A., Nishida C., Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007; 85(9): 660-7. https://dx.doi.org/10.2471/blt.07.043497.
- Higham J.M., O'Brien P.M., Shaw R.W. Assessment of menstrual blood loss using a pictorial chart. Br. J. Obstet. Gynaecol. 1990; 97(8): 734-9. https://dx.doi.org/10.1111/j.1471-0528.1990.tb16249.x.
- Bijur P.E., Latimer C.T., Gallagher E.J. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad. Emerg. Med. 2003; 10(4): 390-2. https://dx.doi.org/10.1111/j.1553-2712.2003.tb01355.x.
- Nadia N., Sri Sunaringsih Ika Wardojo, Rosidah N. Relationship between menstrual pain (dysmenorrhea) and quality of life sleep in adolescent girls at SMA Negeri 1 School West Daha, Hulu Sungai Selatan Regency. J. EduHealth. 2024; 15(02): 1288-93. https://dx.doi.org/10.54209/eduhealth.v15i02.
- Navroski E.C, Franco E.M., Penteado F.A., de Andrade G.F., Lopes J. Dysmenorrhea and pelvic floor muscular dysfunctions in young nuliparaus women: is there an association? 1st Student Scientific Conference of the Brazilian Association for Research and Postgraduate in Physiotherapy (ABRAPG-Ft). BJPT. 2024; 28(Suppl. 1): 100713. https://dx.doi.org/10.1016/j.bjpt.2024.100713.
- Alsaleem M.A. Dysmenorrhea, associated symptoms, and management among students at King Khalid University, Saudi Arabia: an exploratory study. J. Family Med. Prim. Care. 2018; 7(4): 769-74. https://dx.doi.org/10.4103/jfmpc.jfmpc_113_18.
- Yesuf T.A., Eshete N.A., Sisay E.A. Dysmenorrhea among University Health Science students, Northern Ethiopia: impact and associated factors. Int. J. Reprod. Med. 2018; 2018: 9730328. https://dx.doi.org/10.1155/2018/9730328.
- Craig C.L., Marshall A.L., Sjöström M., Bauman A.E., Booth M.L., Ainsworth B.E. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003; 35(8): 1381-95. https://dx.doi.org/10.1249/01.MSS.0000078924.61453.FB.
- Анищенко А.П., Архангельская А.Н., Гуревич К.Г., Дмитриева Е.А., Игнатов Н.Г., Рогозная Е.В. Особенности физического развития студентов вузов. Курский научно-практический вестник «Человек и его здоровье». 2016; 2: 113-5. [Anishchenko A.P., Arkhangel'skaya A.N., Gurevich K.G., Dmitrieva E.A., Ignatov N.G., Rogoznaya E.V. Features of physical development of undergraduates. Kursk Scientific and Practical Bulletin "Man and His Health". 2016; (2): 113-5. (in Russian)]. https://dx.doi.org/10.21626/vestnik/2016-2/21.
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. Suppl. 2006; 450: 76-85. https://dx.doi.org/10.1111/j.1651-2227.2006.tb02378.x.
- Aktaş D. Prevalence and factors affecting dysmenorrhea in female university students: effect on general comfort level. Pain Manag. Nurs. 2015; 16(4): 534-43. https://dx.doi.org/10.1016/j.pmn.2014.10.004.
- Ullah A., Fayyaz K., Javed U., Usman M., Malik R., Arif N. et al. Prevalence of dysmenorrhea and determinants of pain intensity among university-age women. Pain Med. 2021; 22(12): 2851-62. https://dx.doi.org/10.1093/pm/pnab273.
- Potur D.C., Bilgin N.C., Komurcu N. Prevalence of dysmenorrhea in university students in Turkey: effect on daily activities and evaluation of different pain management methods. Pain Manag. Nurs. 2014; 15(4): 768-77.https://dx.doi.org/10.1016/j.pmn.2013.07.012.
- Duman N.B., Yıldırım F., Vural G. Risk factors for primary dysmenorrhea and the effect of complementary and alternative treatment methods: sample from Corum, Turkey. Int. J. Health Sci. (Qassim). 2022; 16(3):35-43.
- Пендрикова О.В., Беридзе Р.М., Захаренкова Т.Н. Современные представления о дисменорее. В кн.: Молодежь и медицинская наука. Статьи VI Всероссийской межвузовской научно-практической конференции молодых ученых с международным участием, Тверь, 22 ноября 2018 г. Тверь: Тверская государственная медицинская академия Министерства здравоохранения Российской Федерации; 2019: 311-3. [Pendrikova O.V., Beridze R.M, Zakharenkova T.N. Modern ideas about dysmenorrhea. In: Youth and medical science. Articles of the VI All-Russian Interuniversity Scientific and Practical Conference of Young Scientists with International Participation, Tver, November 22, 2018. Tver: Tver State Medical Academy of the Ministry of Health of the Russian Federation; 2019: 311-3. (in Russian)].
Received 16.08.2024
Accepted 28.11.2024
About the Authors
Olga M. Kriuchkova, PhD Student at the Department of Obstetrics and Gynecology, Northern State Medical University, Ministry of Health of Russia,163000, Russia, Arkhangelsk, Troitsky Ave., 51, +7(8182)24-03-46, +7(921)477-47-84, Olga.Kriuchkova2@yandex.ru, https://orcid.org/0000-0002-9689-5499
Natalia G. Istomina, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Northern State Medical University, Ministry of Health of Russia,
163000, Russia, Arkhangelsk, Troitsky Ave., 51, +7(8182)24-03-46, +7(921)477-47-84, nataly.istomina@gmail.com, SPIN: 3839-9145, https://orcid.org/0000-0001-9214-8923
Alexey N. Baranov, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology, Northern State Medical University, Ministry of Health of Russia,
163000, Russia, Arkhangelsk, Troitsky Ave., 51, a.n.baranov2011@yandex.ru, SPIN: 5935-5163, https://orcid.org/0000-0003-2530-0379