Продолжение рода и реализация репродуктивной функции – естественная потребность человека [1]. Бесплодие является серьезным препятствием для продолжения рода и актуальной медицинской, социальной и демографической проблемой [2]. В условиях успешного развития вспомогательных репродуктивных технологий (ВРТ) одной из важных задач является уточнение места репродуктивной хирургии в лечении и ведении пациентов с бесплодием [3]. Всем известны преимущества хирургического лечения бесплодия, проявляющиеся в долгосрочном восстановлении репродуктивной функции. Вместе с тем ВРТ имеют явное преимущество в преодолении бесплодия. Есть ли место для репродуктивной хирургии в лечении бесплодия, или это уже история?
Цель исследования – уточнить место хирургического вмешательства в диагностике и лечении бесплодия.
Материалы и методы
Нами проведен ретроспективный анализ результатов хирургического вмешательства у 1845 женщин, прошедших этап диагностики и лечения бесплодия в период с 01 января 2010 г. по 31 декабря 2017 г. на базе гинекологического отделения ЧУЗ «Клиническая больница «РЖД-Медицина» города Барнаула» (главный врач к.м.н. Зальцман А.Г., зав. отделением Тимченко М.А.). Настоящее научное исследование проводилось в рамках комплексной исследовательской работы, утвержденной на заседании научно-координационного совета и одобренной локальным комитетом по биомедицинской этике ФГБОУ ВО «Алтайский государственный медицинский университет» Министерства здравоохранения РФ. Выбор места выполнения хирургического этапа обусловлен опытом совместных комплексных научных исследований, связью с клинической базой кафедры акушерства и гинекологии Алтайского государственного медицинского университета. Кроме того, в названном отделении более 30 лет лечение женского бесплодия является одним из приоритетных направлений.
Для выполнения поставленной задачи, используя сведения базы данных и контактную информацию, указанную в амбулаторных картах, осуществлен телефонный опрос 1845 женщин, прошедших хирургическое вмешательство с целью диагностики и лечения бесплодия. В ходе опроса уточнялись: способ преодоления бесплодия, время и частота наступления беременности и ее исход, факт и количество выполненных процедур ВРТ.
После телефонного опроса из исследования были исключены: пациентки с сопутствующим мужским фактором бесплодия; пациентки, информация о состоянии которых отсутствовала; пациентки, отказавшиеся предоставить информацию о себе; пациентки старше 40 лет. Таким образом, в исследовании осталось 1364 женщины.
Все женщины, прошедшие хирургический этап диагностики и лечения бесплодия, были разделены на четыре группы (рисунок): «хирургическое вмешательство с лечебной целью» (n=671); «лечебно-диагностические гистероскопии» (n=373); «эндоскопическая диагностика причин бесплодия» (n=179); «хирургическое лечение в рамках подготовки к ВРТ» (n=141).
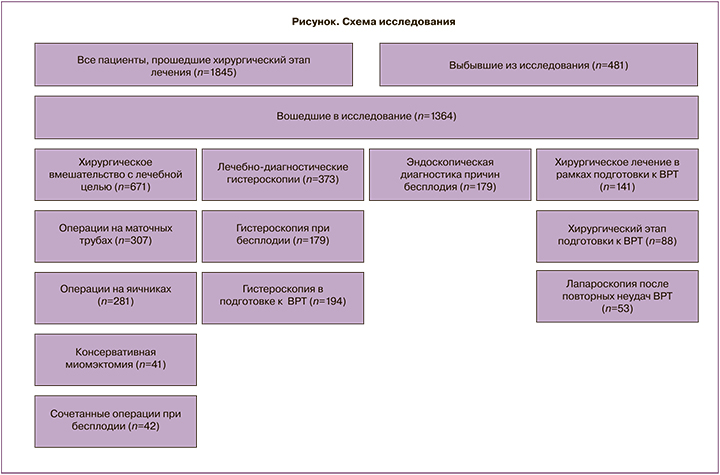
Хирургическое вмешательство с целью долгосрочного восстановления репродуктивной функции применено 671 пациентке. Группа состояла из четырех подгрупп: пациентки после операций на маточных трубах (n=307), после операций на яичниках (n=281), после консервативной миомэктомии (n=41) и после сочетанных операций при бесплодии (n=42).
Тяжесть перитубарного спаечного процесса оценивали по общепринятой шкале Американского общества фертильности (1988). Если в ходе хирургического лечения бесплодия устанавливался низкий прогноз спонтанного наступления беременности, как, например, при IV степени тяжести перитубарного спаечного процесса, пациенткам рекомендовалось экстракорпоральное оплодотворение (ЭКО). В данном случае выполненный объем лечения расценивался как этап подготовки к ЭКО. Так, 41 пациентке с малой вероятностью наступления беременности после проведенного хирургического лечения рекомендовано применение ВРТ. При анализе эти пациентки были отнесены в группу «хирургическое лечение в рамках подготовки к ВРТ».
В группу «лечебно-диагностических гистероскопий» были отнесены 373 женщины. Группа состояла из двух подгрупп. В первой подгруппе (n=179) гистероскопия произведена для исключения патологии полости матки, как причины бесплодия. Ко второй подгруппе отнесены 194 пациентки с гистероскопией на этапе подготовки к ВРТ. Вторая подгруппа состояла из двух когорт: гистероскопия на этапе подготовки к ВРТ (n=87) и 107 женщин с гистероскопией после одной (n=64) или нескольких неудач в цикле ВРТ (n=43).
Диагностическая лапароскопия 179 женщинам осуществлялась в рамках диагностики женского бесплодия неуточненного генеза (N97.9). Условием для включения пациенток в названную группу было отсутствие необходимости хирургического вмешательства при исследовании. Основным клиническим показанием к эндоскопическому лечебно-диагностическому обследованию являлось подозрение на трубный и маточные факторы бесплодия (МКБ-10: N97.1; N97.2) или другие формы женского бесплодия (N97.9). Считается, что сочетание лапароскопии и гистероскопии способствует более точной диагностике причин бесплодия и, как следствие, выбору эффективной тактики лечения [4].
В группу пациенток, обратившихся для комбинированного эндоскопического обследования и лечения с целью подготовки к ВРТ, вошла 141 женщина. Названная группа состояла из двух подгрупп: женщины, оперативное лечение которым осуществлено как хирургический этап подготовки к первому протоколу ВРТ (n=88), и женщины с хирургическим вмешательством с целью диагностики возможных причин неудач в предыдущих циклах ВРТ (n=53).
Методы статистической обработки и анализа полученной информации
Для применения современных методов хранения и анализа массива информации в программе для работы с электронными таблицами Microsoft Excel была создана база данных. Основными требованиями при создании базы данных были ее универсальность, простота использования в практической работе, архивировании и статистической обработке и возможность конвертирования в другие статистические программы. Распределение непрерывных переменных выражалось как среднее значение и стандартное отклонение. Категориальные переменные представлены в виде пропорций и процентов от общего числа. Для доказательства статистически значимого различия сравниваемых величин использовался z-критерий для долей [5]. Значение р<0,05 считалось статистически значимым. Для статистического анализа применялся программный пакет Statistica (разработка компании StatSoft) версия 10.
Результаты
Эффективность хирургического лечения бесплодия
В рамках хирургического лечения бесплодия оперативные вмешательства были применены 671 пациентке. Средний возраст оперированных составил 29,7 (2,4) года. Средняя длительность бесплодия – 3,6 (1,5) года. В течение двух лет после хирургического лечения самостоятельное наступление беременности диагностировано у 225 (33,5%) пациенток. Внематочная беременность как исход репродуктивной хирургии наступила у 17 женщин (7,6%). Самопроизвольное прерывание беременности в раннем сроке произошло у 34 (15,1%). Роды как конечная цель лечения бесплодия произошли у 174 женщин (25,9%). Частота наступления беременности в зависимости от объема хирургического вмешательства приведена в таблице 1.
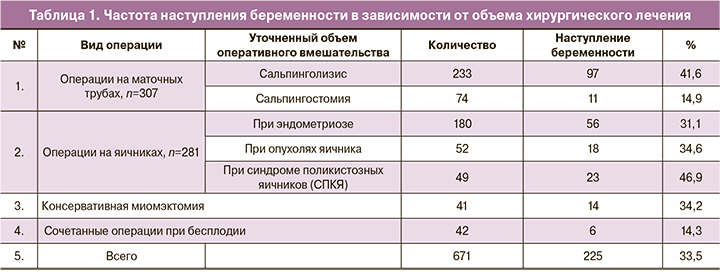
Эффективность консервативно-пластических операций на маточных трубах
Операции на маточных трубах при бесплодии выполнены 307 женщинам. Средний возраст обратившихся был 31,3 (2,2) года. Средняя длительность бесплодия – 3,3 (1,5) года. Из 307 случаев хирургического вмешательства на маточных трубах у 233 женщин был выполнен сальпинголизис при I степени выраженности перитубарного спаечного процесса, а у 74 пациенток – сальпингостомия, фимбриопластика и сальпингостоматопластика при II–III степени тяжести спаечного процесса. Женщины отличались только по выполненному объему лечения.
Беременность после сальпинголизиса при I степени тяжести перитубарного спаечного процесса наступила у 97 женщин (41,6%) и у 11 (14,9%) при II–III степени тяжести перитубарного спаечного процесса (р<0,0001). Причем, у большинства оперированных на маточных трубах (82 из 108 – 75,9%) беременность наступила в первые 6–8 месяцев после операции. Общепризнанно, что репродуктивная хирургия является фактором риска трубной беременности. Из 108 беременностей у 14 женщин диагностирована внематочная беременность (13%). В большинстве случаев внематочная беременность наступила у пациенток после операций при I степени тяжести перитубарного спаечного процесса, тогда как повторные операции, связанные с формированием или рецидивом гидросальпинкса отмечены у каждой третьей из оперированных в объеме сальпингостомии и фимбриопластики. Повторная беременность, закончившаяся родами, наступила у 20 женщин (18,5%), что является свидетельством долгосрочного восстановления репродуктивной функции. Невынашивание беременности диагностировано у 17 женщин (15,7%), что не превышает частоту прерывания беременности в популяции [6].
Влияние хирургического вмешательства на яичниках на реализацию репродуктивной функции
Операции на яичниках выполнены 281 женщине. В большинстве случаев оперативное вмешательство на яичниках являлось симультанным и осуществлялось по гинекологическим показаниям. Так, у 180 женщин операции на яичниках осуществлены при эндометриозе, 52 – при опухолях яичника и 49 пациенткам произведен дриллинг или электрокаутеризация при СПКЯ. Таким образом, только у 49 женщин целью операции на яичниках было бесплодие. Несмотря на то что основным показанием к операции у 232 женщин были опухоли яичников, отмечено положительное влияние проведенного лечения на сопутствующее бесплодие. Спонтанная беременность после хирургического лечения наступила у 77 пациенток (33,2%).
Среди оперированных на яичниках у 180 бесплодных женщин показанием к операции был эндометриоз яичников. Средний возраст пациенток названной группы – 30,7 (2,3) года. У большинства (62,5%) бесплодие было первичным. В послеоперационном периоде 35 (19,4%) пациенткам назначался курс агониста гонадолиберина. После лечения самостоятельная беременность наступила у 56 женщин (31,1%), семь беременностей закончились выкидышем.
Другими опухолями яичника, сопутствующими бесплодию, были зрелые тератомы и цистаденомы, обнаруженные у 52 женщин. Средний возраст оперированных составил 28,6 (2,2) года. В 55% случаев бесплодие было первичным. Оперативное вмешательство проводилось в объеме цистэктомии или резекции яичника. У 20 женщин (38,5%) резекция яичников была двусторонней. Самостоятельная беременность после резекции объемного образования яичника при бесплодии наступила у 18 женщин (34,6%). После двусторонней резекции яичников беременность наступила у 7 (35%) из 20 женщин с названным объемом вмешательства. У большинства женщин беременность наступила в течение первого года после операции. У трех пациенток после резекции яичников был ановуляторный цикл, и беременность наступила в стимулированном кломифеном цикле; одна беременность наступила при инсеминации спермой мужа. У 12 женщин (23,1%) оперативное вмешательство на яичниках ассоциировалась с последующим выраженным снижением овариального резерва, затруднившим реализацию репродуктивной функции.
Показанием для оперативного лечения (дриллинга или электрокаутеризации яичников) у 49 женщин явилось эндокринное бесплодие при СПКЯ. Средний возраст этой группы составил 25,6 (1,7) года. Большинство женщин с СПКЯ имели в анамнезе повторные циклы стимуляции овуляции. У 7 женщин была ранее диагностирована резистентность к кломифену. После хирургического лечения беременность наступила у 23 женщин (46,9%). У большинства пациенток (n=12) наступление беременности произошло в течение первых 8 месяцев после операции. У восьми пациенток после родов отмечено наступление повторной беременности.
Влияние консервативной миомэктомии на реализацию репродуктивной функции
Сорок одной женщине с бесплодием неуточненного генеза выполнена консервативная миомэктомия. Во всех случаях миома была сопутствующей патологией и не ассоциировалась с причиной бесплодия. Оперативное вмешательство, как правило, выполнено на субсерозных и интрамуральных узлах. Средний возраст пациенток данной подгруппы был 32,4 (2,1) года. У всех оперированных маточные трубы были проходимы, и менструальный цикл был овуляторным. Случаи миомэктомии с проникновением в полость матки и при сочетанных операциях исключались из названной группы.
Самостоятельная беременность после консервативной миомэктомии наступила у 14 (34,2%) женщин. У 6 беременность наступила в течение первого года после операции. Гестация закончилась родами у 12 женщин, и у 3 диагностирована внематочная беременность (у одной пациентки после трубной беременности наступила спонтанная маточная беременность, закончившаяся родами).
Реализация репродуктивной функции после сочетанных операций при бесплодии
Сочетанное оперативное вмешательство при бесплодии применено 42 женщинам. Средний возраст оперированных составил 32,7 (2,1) года. Средняя длительность бесплодия – 4,3 (1,5) года. Ранее 10 женщинам уже осуществлялись оперативные вмешательства на репродуктивных органах. Сочетанное хирургическое вмешательство проведено: на маточных трубах и яичниках – 21 женщине; на маточных трубах, резекция яичников и консервативная миомэктомия – 18 пациенткам; у 3 пациенток операции на маточных трубах и яичниках сочетались с иссечением и коагуляцией очагов эндометриоза. Самостоятельная беременность наступила всего у 6 женщин (14,3%).
Реализация репродуктивной функции после лечебно-диагностических гистероскопий
Гистероскопия, будучи инструментальным методом, применяется не только для диагностики причин бесплодия, но и для уточнения причин неудач в программах ВРТ, составления дальнейшего прогноза преодоления бесплодия. В группу лечебно-диагностических гистероскопий вошли 373 женщины. У пациенток 1-й подгруппы (n=179) с бесплодием неуточненного генеза при гистероскопии исключалась патология эндометрия как возможная причина бесплодия. Средний возраст женщин данной подгруппы составил 29,3 (2,1) года. Во 2-й подгруппе (n=194) гистероскопия выполнялась в рамках подготовки к ВРТ либо для диагностики возможных причин неудач в предыдущих циклах ВРТ. Средний возраст женщин данной подгруппы составил 34 (1,9) года.
При гистероскопии в рамках диагностики причин бесплодия патология эндометрия была обнаружена в 46,2% случаев. Наиболее часто при оценке полости матки диагностировались: хронический эндометрит (24,4%), полипы эндометрия (11,6%), субмукозная миома (10,5%). Синехии полости матки и гиперпластический процесс эндометрия встречались с одинаковой частотой – 4,7%. Аномалии развития матки диагностированы в 3,5% случаев.
После выполнения гистероскопии, а при наличии показаний – и коррекции обнаруженной патологии, в период от 1 до 2 лет беременность наступила у 28 (15,6%) из 179 женщин. У 12 женщин (42,9%) беременность наступила в течение первых 6 месяцев после процедуры. Повторная беременность наступила только у 4 пациенток в течение двух лет после родоразрешения.
Особый интерес вызывают данные, полученные при гистероскопии, осуществленной в рамках подготовки к ВРТ (n=194). По характеру отношения к циклам ВРТ проведен сравнительный анализ особенностей пациенток названной подгруппы. У 87 женщин гистероскопия предшествовала первой программе ВРТ, 107 пациенткам гистероскопия выполнена при планировании протокола после повторных неудач программ ВРТ (табл. 2).
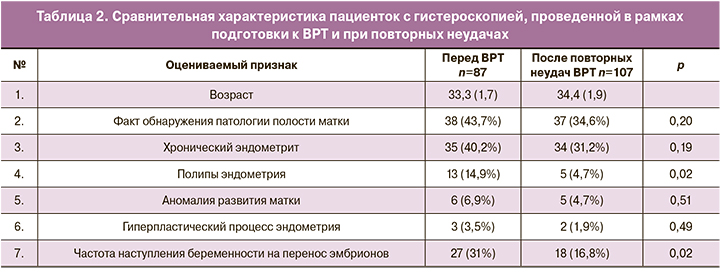
Информация, представленная в таблице, наглядно демонстрирует отсутствие позитивного влияния гистероскопии на последующую результативность циклов ВРТ. Известно, что частота наступления беременности у женщин после комбинированного эндоскопического обследования в рамках подготовки к ВРТ – 31,3%. При сравнении показателей частоты наступления беременности в циклах ВРТ статистически значимой разницы между комбинированным эндоскопическим обследованием и гистероскопией перед ВРТ не обнаружено (31,3% и 31,0%). Статистически значимое различие в частоте наступления беременности было при сравнении подгрупп пациенток с гистероскопией перед программой ВРТ и после неудачных программ ВРТ – 31% и 16,8% (р<0,05).
Реализация репродуктивной функции после диагностической лапароскопии при бесплодии
В рамках инструментальной диагностики причин бесплодия диагностическая лапароскопия применена 179 пациенткам. Средний возраст пациенток с диагностической лапароскопией составил 27,8 (2,3) года. При хромолапароскопии у 17 женщин (9,5%) диагностирована непроходимость маточных труб в истмических или интрамуральных отделах, что определило дальнейшую лечебную тактику по преодолению бесплодия.
После диагностической лапароскопии в период от 1 до 2 лет беременность наступила у 82 из 162 женщин (50,6%), ожидающих наступления беременности. Средний возраст женщин с наступлением спонтанной беременности был 25,1 (2,1) года. Всего у 82 женщин наступило 103 беременности (87 родов, 17 самопроизвольных выкидышей в раннем сроке, 5 абортов, 4 внематочных беременности). Повторная беременность наступила у 31 пациентки в течение первых полутора лет после родоразрешения, что является показателем долгосрочного восстановления фертильности после диагностической лапароскопии.
Эффективность наступления беременности у пациентов, прошедших эндоскопическое обследование в рамках подготовки к ВРТ
Эндоскопическое обследование в рамках подготовки к ВРТ выполнено 141 женщине. Группа состояла из двух подгрупп: 88 женщинам обследование осуществлялось на этапе планирования ВРТ; 53 женщинам после неудач ВРТ – для исключения либо минимизации влияния патологии органов малого таза на результативность ВРТ.
Из 88 женщин 1-й подгруппы у 41 при сочетанном хирургическом лечении прогнозировалась низкая вероятность наступления беременности при выжидательной тактике. У 30 пациенток были удалены маточные трубы при гидросальпинксе либо его рецидиве, и у 17 женщин трубное бесплодие было подтверждено диагностической лапароскопией. Средний возраст женщин, прошедших хирургический этап подготовки к ВРТ, составил 32,5 (2,1) года. У 33 пациенток (37,5%) были оперированы яичники (объемные образования, в половине случаев являющиеся эндометриоидными кистами). Консервативная миомэктомия на этапе подготовки к ВРТ проведена 17 женщинам. У двух женщин, 30 и 35 лет, при ожидаемом неблагоприятном прогнозе наступления беременности после хирургического лечения на этапе ожидания программы ВРТ наступила спонтанная беременность, закончившаяся самостоятельными родами. Восемьдесят шесть оставшихся женщин провели 118 программ ВРТ, беременность наступила у 62. Кумулятивная частота наступления беременности на пациентку составила 72,1%, частота наступления беременности на программу с учетом переносов в криоциклах составила 52,5% и частота наступления беременности на перенос эмбрионов – 31,3%.
Эндоскопическое обследование в рамках диагностики возможных причин предшествующих неудач ВРТ применено 53 женщинам. Средний возраст пациенток составил 34,2 (2,2) года. В анамнезе названной когорты было от 1 до 6 неудачных программ ВРТ (в среднем 1,9). При эндоскопическом обследовании 26 пациенткам осуществлены операции на маточных трубах, причем у 14 маточные трубы удалены из-за визуально выраженных морфологических изменений. У трех пациенток с повторными неудачами ВРТ диагностированы вентильные гидросальпинксы, явившиеся интраоперационной находкой. У 32 пациенток выполнены операции на яичниках, у 6 – консервативная миомэктомия, в 11 случаях (20,8%) –коагуляция очагов эндометриоза. У 4 женщин (7,6%) отмечено спонтанное наступление беременности на этапе планирования очередной программы ВРТ. Кумулятивная частота наступления беременности при применении ВРТ после проведенного оперативного вмешательства составила уже 54,2%. Эффективность программ ВРТ с учетом криопереносов составила 37,2%, частота наступления беременности на перенос – 23,8%.
На этапе планирования ВРТ консервативная миомэктомия выполнена 23 женщинам: 17 – в рамках хирургического этапа подготовки к ВРТ и 6 – при повторных неудачах циклов ВРТ. Кумулятивная частота наступления беременности у пациентов, оперированных в объеме консервативной миомэктомии, составила 60,9%. Статистически значимого различия в частоте наступления беременности среди пациентов ВРТ не отмечено.
Обсуждение
В 1997 г. Glatstein et al. сообщили, что лапароскопия применялась 89% специалистов, занимающихся диагностикой бесплодия в США [7]. Однако уже в 2002 г. Fatum M. et al. поставили под сомнение ценность лапароскопического вмешательства при бесплодии с учетом возможностей ЭКО [8]. По мнению Xiaoming Yu. et al. (2019), достижения в области неинвазивных методов, таких как ультразвуковое исследование или гистеросальпингография, поставили под сомнение необходимость лапароскопии при лечении бесплодия [9].
В литературе широко дискутируется вопрос целесообразности реконструктивно-пластических операций при трубном бесплодии [10]. Результаты нашего исследования свидетельствуют о зависимости эффективности операций на маточных трубах от объема проведенного лечения. Сальпинголизис при I степени перитубарного спаечного процесса у молодых пациенток имеет явные преимущества перед сальпингостомией и сочетанными операциями на маточных трубах (41,6%, 14,9% и 14,3%; р<0,0001). Полученные данные подтверждают мнение других исследователей о невысокой эффективности реконструктивно-пластических операций на маточных трубах [11].
Хирургические вмешательства на яичниках – зачастую вынужденная мера. Показанием к оперативному вмешательству является объемное образование яичника, а не бесплодие. В ходе оперативного лечения кист яичников, сопутствующих бесплодию, возможно восстановление репродуктивной функции. Согласно нашему исследованию, беременность наступила у 18 женщин из 52 прошедших оперативное лечение (34,6%). Однако практически у каждой пятой (23,1%) операция на яичниках привела к выраженному снижению овариального резерва. Общепризнано, что операции на яичниках негативно влияют на репродуктивный потенциал [12]. При хирургическом вмешательстве на яичниках важно стремиться к минимальному повреждению овариальной ткани.
После резекции яичников при синдроме поликистозных яичников (СПКЯ) у большинства молодых пациенток беременность может наступить в течение 6–12 месяцев. Данный вид вмешательства может рассматриваться в рамках персонифицированного подхода у кломифенрезистентных пациенток с СПКЯ.
Связь эндометриоза и бесплодия несомненна [12, 13]. Хирургическое лечение при наружном генитальном эндометриозе эффективно только у каждой третьей. При сравнительном анализе частота наступления беременности после оперативного лечения у пациенток с сальпинголизисом выше, чем у пролеченных по поводу эндометриоза (41,6% и 31,1%; р=0,02). Считается, что операция дает преимущества пациентам с ранней стадией эндометриоза [14, 15]. Вопрос о том, следует ли лечить минимальный и умеренный эндометриоз в случае бесплодия, остается до сих пор нерешенным [11]. Ожидание эффективности лечения может занимать длительный срок, от 12 до 24 месяцев. В старшей возрастной группе (женщины после 35 лет) длительность ожидания наступления беременности может иметь негативные последствия. Частота хромосомных аномалий в ооцитах растет пропорционально возрасту пациенток [16]. После оперативного лечения эндометриоза яичников у женщин старше 35 лет необходимо оценить целесообразность проведения ВРТ. Полученные нами данные позволяют подтвердить негативное влияние эндометриоза на репродуктивную функцию.
По мнению Zepiridis L.I. еt al. (2016), Carranza-Mamane et al. (2015), миома матки сопровождает бесплодие в 5–10% и может быть одной из его причин [17, 18]. В нашем исследовании частота диагностики миомы при бесплодии составила 14,7%. В исследовании Goldberg J. еt al. (2006) сообщается о 50–60% частоте наступления беременности после миомэктомии с хорошими акушерскими результатами [19]. Частота наступления беременности после консервативной миомэктомии в нашем исследовании составила 34,2%. Вместе с тем, нет веских доказательств влияния непосредственно миомэктомии на последующее наступление спонтанной беременности.
В исследовании Bulletti C. еt al. (2004) сообщается, что хирургическое удаление миом на этапе подготовке к ВРТ может быть полезно для повышения результативности программ [20], а в работе Ojo-Carons M. еt al. (2016) – о возможной экономической выгоде удаления узлов перед проведением ВРТ [21]. В нашем исследовании статистически значимого влияния миомэктомии на последующую кумулятивную результативность программ ВРТ не обнаружено (72,1% и 60,9%; р=0,3).
Несмотря на представления о миомэктомии как о золотом стандарте лечения [18], убедительных доказательств влияния миомы и ее оперативного лечения на реализацию репродуктивной функции, как спонтанной, так и после ВРТ, нами не получено.
В исследовании Perquin D.A.M. еt al. (2006) сообщается о наступлении спонтанной беременности после диагностической лапароскопии в 51% [22] случаев, в более позднем исследовании Shimizu Y. et al., (2016) частота спонтанной беременности после лапароскопии сопоставима по эффективности с ВРТ [23]. В работе, проведенной нами, частота наступления беременности после диагностической лапароскопии составила 50,6%. Учитывая длительность бесплодия перед диагностической лапароскопией от 2 до 10 лет (в среднем 3,3 года), очевиден положительный эффект данной манипуляции.
В настоящее время гистероскопия является наиболее эффективным способом оценки состояния эндометрия и цервикального канала [24, 25]. Патология эндометрия часто встречается у бесплодных женщин, препятствуя наступлению спонтанной беременности, и может снижать частоту беременности при ВРТ (стимуляции овуляции, инсеминации, ЭКО) [25]. В исследовании Sardo et al. (2016) были получены доказательства увеличения частоты клинических беременностей у бесплодных женщин после хирургической коррекции обнаруженной патологии полости матки. В других публикациях звучит требование применения гистероскопии при неуточненном бесплодии и необходимости дополнительных исследований влияния манипуляции на реализацию репродуктивной функции [26, 27]. Полученные нами данные не выявили повышения частоты наступления беременности у пациентов после гистероскопии. Вне зависимости от вмешательств, направленных на коррекцию обнаруженной при гистероскопии патологии, частота наступления спонтанной беременности не превышала 15,6%.
Некоторые авторы свидетельствуют о повышении эффективности ВРТ после применения гистероскопии [27, 28]. В нашем исследовании позитивного влияния гистероскопии на последующую эффективность ВРТ не обнаружено.
Недостатком нашего исследования является ограниченное число женщин, которые приняли участие в испытании. Пациенты, включенные в анализ, были чрезвычайно разнородными по нескольким факторам. В исследовании присутствует риск систематической ошибки. Особенности методологии, снижающие чистоту эксперимента при клиническом разнообразии анализируемых групп, могут ограничивать научную ценность нашей работы. Однако представленный пациентами срез является универсальным, соответствующим реальной клинической практике.
Заключение
Хирургическое лечение бесплодия – действенный способ восстановления репродуктивной функции. Эффективны хирургические вмешательства у молодых женщин с минимальной степенью повреждения маточных труб. Целесообразность консервативно-пластических вмешательств на маточных трубах сомнительна ввиду невысокой частоты наступления маточной беременности, повышенного риска эктопической локализации плодного яйца и высокого риска рецидива рубцово-спаечного процесса. Важность хирургического этапа при планировании ВРТ несомненна. Гидросальпинксы, субмукозная локализация миомы, активный эндометриоидный процесс могут снижать частоту наступления беременности при ВРТ. Своевременная диагностика и хирургическая коррекция этой патологии гениталий перед протоколом могут повысить вероятность успешности ВРТ. Сочетанные изменения органов малого таза должны оперироваться по гинекологическим показаниям в рамках подготовки к ЭКО.