The risk factors and pattern of preterm birth in the fetal residents of the Republic of Kazakhstan
Objective. To identify the risk factors and pattern of preterm birth.Marat A.A., Ukybassova T.
Subjects and methods. A total of 11,861 births were retrospectively analyzed; 1806 (15.2%) of them were preterm. The odds ratio (OR) and confidence interval (CI) were calculated for the risk factors of preterm birth.
Results. The study of the social portrait of women having preemies showed that their educational level (OR, 2.7; SE, 0.29; 95% CI, 1.5–4.8), employment (OR, 2.4; SE, 0.29; 95% CI, 1.3–4.1), and place of residence (OR, 1.5; SE, 0.29; 95% CI, 0.9–2.7) were statistically significant risk factors for preterm birth.
The main risk factors for preterm birth were isthmic-cervical insufficiency, a history of preterm birth and fetal loss (OR, 2.66; SE, 0.35; 95% CI, 1.3–5.3), and low-weight birth babies (OR, 2.38; SE, 0.37; 95 CI, 1.2–5.1).
Conclusion. Family planning, pregravid preparation of an expectant mother, and preventive measures in pregnant women at high risk for preterm birth can reduce preterm birth rates.
Keywords
In 1974, the World Health Organization (WHO) proposed to consider children viable born with a body weight of more than 500 g at 22 weeks gestation and later. Thus, according to WHO, preterm labor is considered to be childbirth up to 37 full weeks of gestation. Since 2008, in the Republic of Kazakhstan (and since 2002 in the city of Almaty as a pilot project), WHO livebirth and stillbirth criteria have been applied [1]. Despite advances in medical science, according to WHO 15 million children worldwide are born “too early” annually, more than 1 million of these children die every year. According to the WHO data, the preterm birth rate in the Republic of Kazakhstan in 2010 was 8.8 per 100 births [2].
In 2013, the WHO experts evaluated the mortality rate in children under 5 years old in the Republic of Kazakhstan. According to this evaluation, the infant mortality rate caused by preterm birth was 19% and premature birth took the second place after the congenital malformations of the fetus [3].
Since WHO livebirth criteria were applied in our country, the preterm birth rate has remained relatively stable. In the Republic, there was a slight increase in the preterm birth rate in 2011, it was 6.7%; a decrease in the preterm birth rate was observed in 2015, it was 5.8%. In 2017, the preterm birth rate in the country was 6.1% [4, 5, 6].
The causes of the onset of preterm labor are diverse. The development of spontaneous preterm labor results from many pathological processes, and their cause may be due to the interaction of various factors from the mother and the environment, as well as the fetus.
The identification of risk factors for the prediction of preterm labor is necessary for several reasons. First, identifying a woman at risk allows specialists to begin treatment with a risk perspective. Secondly, risk factors can determine the population for studying specific interventions. Finally, identifying risk factors helps reveal important mechanisms which might cause premature birth [7].
The purpose of the study was to investigate possible risk factors for the onset of preterm labor and to analyze the pattern of preterm labor.
Materials and Methods
To achieve the goals, we retrospectively analyzed 11,861 deliveries including 1,806 premature ones (15.2%) from January 2015 to December 2017 at National Scientific Center for Motherhood and Childhood and Astana Medical University, Kazakhstan. The odds ratio (OR), the confidence interval (CI) of risk factors for preterm labor, and logistic regression were calculated to determine the probability of the onset of preterm labor.
Results
The preterm birth rate was 15%, which was twice as high as average rate in the Republic. It was due to the concentration of patients with severe obstetric and extragenital pathology in these medical institutions. The studies of the causes of preterm births showed that the majority of premature births (76.7%) were due to medical reasons including 16% of induced preterm delivery. Premature cesarean deliveries were performed in 60.7% of cases, spontaneous premature births were observed in 23.3% of cases including premature births resulting from preterm rupture of membranes, 11.5%. Therefore, half of the spontaneous preterm births began with premature rupture of membranes.
The main reasons for programmed preterm labor were such indications as mother’s hypertension, in 33% of cases, and impaired functional status of the fetus, in 25% of cases. Pregnant women were prematurely delivered by induction of labor and cesarean section in 33% of cases due to severe preeclampsia, eclampsia and in one case due to the development of HELLP syndrome; 6.2% of the deliveries were due to diabetes-related complications. Placental attachment disorders were an indication for premature delivery in 3.2% of cases.
Another crucial complication of pregnancy course was premature detachment of a normally situated placenta, its frequency during preterm labor was 2.4% (Figure).
Other indications for premature birth were onset of labor, premature rupture of membranes as well as the presence of a scar in the uterus after cesarean section and/or contraindications to vaginal delivery. Extragenital diseases contributed to the development of pregnancy complications in every third patient. Most frequent extragenital diseases were blood diseases (anemia, thrombocytopenia) in 33% of cases, diseases of the cardiovascular system (arterial hypertension, congenital and acquired heart defects) in 10.9% of cases, diseases of the urinary system and digestive organs were revealed in 6.7% and 4.5% of patients, respectively.
Somatic health disorders in patients who gave preterm birth determined a high incidence of impaired functional status of the fetus: intrauterine growth retardation was revealed in 21% (373) of patients, fetal abnormality in 4.3% (79) of cases, fetopathy due to diabetes in 5.4% (99) of patients. There was a threatening condition of the fetus which was an indication for emergency premature delivery in 25.3% (458) of cases. Also, the impairment of the fetal status resulting from rhesus incompatibility occurred in 4.5% (82) of cases.
After studying the period of the onset of preterm labor, it was noted that the majority of preterm births (70%) were births from 32 weeks 0 days to 36 weeks 6 days; about 18% of births were from 28 weeks 0 days to 31 weeks 6 days; and 12% of births were from 22 weeks to 27 weeks 6 days.
During the next stage of investigation, social and demographic risk factors for the onset of preterm labor were studied. The age of women who gave birth prematurely ranged from 18 to 42 years. The average age was 29.2 ± 3.4 years. A majority of women who gave birth prematurely were aged between 20 and 30 years, their number was 721 (40%) patients. Women whose age was between 30 and 34 years were less numerous, 636 (35.2%) patients.
Among women who gave preterm birth, 65% were rural residents, 62% were housewives, 57% of them did not have higher education. Distribution by social indicators and odds ratios are shown in Table1.

Thus, according to the data obtained as the result of our research, the level of education (OR – 2.7, SE – 0.29, 95% CI:1.5–4.8), employment (OR – 2.4, SE - 0.29, 95% CI:1.3–4.1) and place of woman’s living (OR – 1.5, SE – 0.29, 95% CI:0.9–2.7) are statistically significant risk factors for preterm birth. Perhaps this is due to the low socio-economic status of such families. As a rule, these are patients who come from remote regions of the country. Due to the difficulties in counting, we did not analyze such risk factors as daily workload during working hours (mental workload, night, day time, hard work, standing work), social and economic aspects: family income, etc.
Analysis of obstetric history of pregnant women showed that 14.2% of patients were primigravidas, 85.8% of women were multigravidas. Among recurrent infections, 26.3% of pregnancies occurred after several perinatal losses (two or more miscarriages), 32.2% of pregnancies were preceded by preterm births, 2.4% of patients had surgical interventions in the anamnesis due to cervical insufficiency.
Preterm births in the anamnesis were often associated with the subsequent preterm births, and this connection is reflected in our study (Table 2).
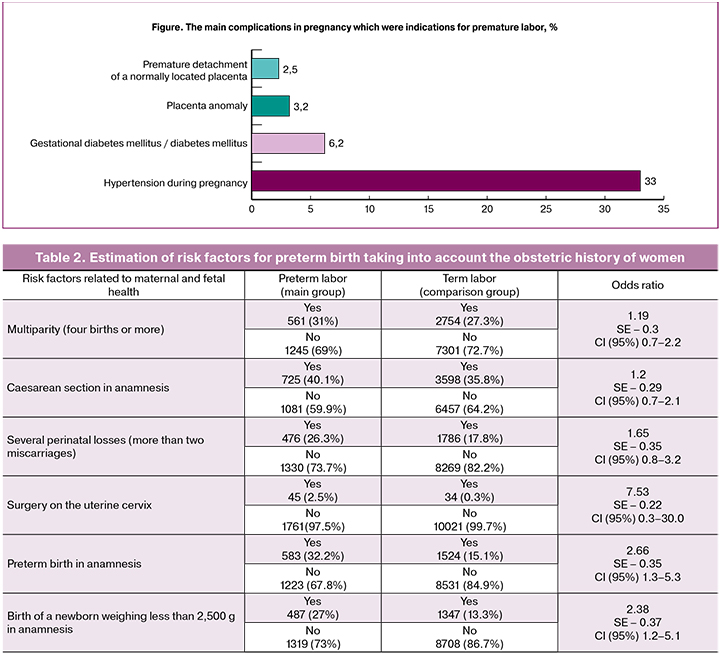
As shown in Table 2, statistically significant risk factors associated with maternal health and affecting preterm birth were previous pregnancy loss (OR - 1.65, SE – 0.35, 95% CI:0.8–3.2), birth of a newborn weighing less than 2,500 g in anamnesis (OR – 2.38, SE – 0.37, 95% CI:1.2–5.1), previous preterm birth (OR – 2.66, SE – 0.35, 95% CI:1.3–5.3). It should be noted that cervical insufficiency (OR – 7.53, SE – 0.22, 95% CI:0.3–30.0) also affected the development of preterm labor. Such factors as multiparity including four or more births (OR – 1.19, SE – 0.3, 95% CI:0.7–2.2) and the presence of a scar in the uterus after cesarean section (OR – 1.2, SE – 0.29; 95% CI:0.7–2.1) were not statically significant.
To determine the most significant risk factor for the onset of preterm labor, a logistic regression was applied. To this end, 11 dichotomous variables were analyzed. Of all 11,861 cases, 861 cases were selected using the random number generator function in Excel. With the help of logistic regression, we stopped at a three-factor model, which included the Body Mass Index (BMI), education and birth of a child weighing 2,500 g and less in the anamnesis.
Y= 0.151 + 5.041*BMI – 3.515*Education + 0.455*Anamnesis _2500
The percentage of correctly predicted values of the dependent variable increased by 7.8% from 68.5% to 76.3%. And such a measure of certainty as the Nagelkerk R square increased by 0.291 from 0.214 to 0.505. If we take the values of three independent variables for the obtained model for the first woman from our database, we get
Y= 0.151 + 5.041*1 – 3.515*1 + 0.455*0
With these values of independent variables, the value of Y will be 1.677. This value must be substituted into the logistic function, which has the following form:
Substitute the obtained value of 1.677 in the formula
As a result, we get 0.843. This value indicates the likelihood of preterm labor. Since the threshold value is a probability of 0.5, it can be predicted with an 84.3% probability that this patient will have a preterm birth.
Discussion
The frequency of preterm birth in Kazakhstan in 2017 according to official statistics was 6.4%, in specialized obstetric organizations this rate reached 15%.
The results of our study show that in three-quarters of women premature birth was caused by the condition of maternal health, such as hypertensive status, preeclampsia, eclampsia, cardiovascular diseases. Somatic diseases of the mother can be not only a predictor of the development of complications in the mother, but also in the intrauterine fetus, which is evident from the results of our research. Impairments of the functional fetal state contributed to the induction of labor in 25% of cases. In every fifth patient, the indication for induction of labor was a delay in the development of the fetus; in one out of four patients, there was a threatening condition of the fetus.
Among all premature births, the quantity of spontaneous labor was 23.3% of cases, half of them started with premature rupture of membranes.
According to the data of our study, the social portrait of women who gave birth prematurely is as follows: from 20 to 34 years old, mainly from rural areas, housewives, primary and/or secondary education. Similar data were obtained by other authors. According to them, the maternal demographic characteristics associated with preterm birth include low socio-economic and educational level, low and high maternal age and the absence of a partner [8, 9].
The result of our study showed that the course and outcome of previous pregnancies were closely related to the course and outcome of current pregnancy: loss of pregnancies (OR – 1.65, SE – 0.35, 95% CI:0.8–3.2), birth of a low weight baby (OR – 2.38, SE – 0.37, 95% CI:1.2–5.1), preterm birth (OR – 2.66, SE — 0.35, 95% CI:1.3–5.3). Also, a history of cervical insufficiency (OR – 7.53, SE - 0.22, 95% CI:0.3–30.0) was a risk factor that was statistically significant in the development of preterm labor.
The risk of recurrence of preterm birth in women with previous preterm birth varies from 15% to 50%, depending on the number and gestational age of previous preterm births. Thus, according to the authors, previous premature births increased the risk of premature births by 2–5 times during the next pregnancy [10]. Moreover, an interval between pregnancies is of critical importance. According to the meta-analysis of Conde-Agudelo A. et al. (2006) there is an increased risk for preterm delivery with a short intergenetic interval, so with an interval of less than 6 months, the risk of premature birth increases twice [11].
Similar data were obtained in a study of risk factors for preterm birth in Europe [12]. However, according to some authors, the age of the mother, place of work, education level did not have a statistically significant relationship with preterm birth. The results of another study revealed that premature rupture of membranes, multiple pregnancies, hypertension conditions, obstetric history, isthmic-cervical insufficiency, and the mother’s age over 35 years significantly increased the frequency of preterm birth [13].
Conclusion
In our study, the incidence of preterm labor in facilities providing highly specialized care was 15% (1.806 cases out of 11.861 births). Due to the deterioration in maternal and fetal condition, programmed labor (76%) dominated among preterm births. The background for the onset of preterm labor was maternal disorders, such as hypertensive diseases, cardiovascular diseases. Health improvement in these women may become a real way to reduce the frequency of preterm birth in Kazakhstan.
According to the results of our study, risk factors for preterm birth are isthmic-cervical insufficiency, repeated pregnancies with previous preterm labors and a history of several perinatal losses, low birth weight babies, mother’s age, low level of education, living in rural areas, and BMI more than 25. Therefore, the above mentioned risk factors referring to the onset of preterm labor are of critical importance for the residents of Kazakhstan.
Family planning, preconception care of expectant mothers and preventive measures for reducing the frequency of preterm birth in pregnant women at high risk can affect the decrease in premature birth rate.
References
1. Распоряжение Премьер-Министра Республики Казахстан от 1 марта 2006 года № 38-р «Об утверждении Плана мероприятий по переходу Республики Казахстан на критерии живорождения и мертворождения, рекомендованные Всемирной организацией здравоохранения». [Decree of the Prime Minister of the Republic of Kazakhstan dated March 1, 2006 No. 38-p “On approval of the Action Plan for the transition of the Republic of Kazakhstan to the live birth and stillbirth criteria recommended by the World Health Organization”.]
3. Всемирная организация здравоохранения. Информационный бюллетень N°363 ноябрь 2012г. Available at: http://www.who.int/mediacentre/facts heets/fs 363/ru. [World Health Organization. 2012 newsletter. //www.who.int/maternal_child_adolescent/documents/ born_too_soon/ru/.]
4. WHO. Kazakhstan: WHO statistical profile. Available at: http://who.int/gho/mortality_burden_disease/en/
5. Юлдашева Ж.Р., Ерғалиқызы А., Уркумбаева С.Н. Анализ преждевременных родов как резерв в снижении перинатальной смертности. Вестник КазНМУ. 2015; 2: 1-5. [Yuldasheva Zh.R., Yergalygyzy A., Urkumbaeva S.N. Analysis of preterm birth as a reserve in reducing perinatal mortality. Bulletin of KazNMU. 2015; 2: 1-5. (in Russian)]
6. Goldenberg R.L., Goepfert A.R., Ramsey P.S. Biochemical markers for the prediction of preterm birth. Am. J. Obstet. Gynecol. 2005; 192(5, Suppl.): S36-46.
7. Heaman M., Kingston D., Helewa M.E., Brownell M., Derksen S., Bogdanovic B., McGowan K.L., Bailly A. Perinatal services and outcomes in Manitoba, November 2012, Manitoba Centre for Health Policy Department of Community Health Sciences Faculty of Medicine, University of Manitoba.
8. Palmer K.T., Bonzini M., Harris E.C., Linaker C., Bonde J.P. Work activities and risk of prematurity, low birth weight and pre-eclampsia: an updated review with meta-analysis. Occup. Environ. Med. 2013; 70(4): 213-22.
9. Yatnita Parama Cita and Resmiati. The relationship between demographic factors and low birth weight infants. Int. J. Res. Nurs. 2010; 1(1): 25-
10. Conde-Agudelo A., Rosas-Bermudez A., Kafury-Goeta A.C. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006; 295(15): 1809-23.
11. Tucker C.M., Berrien K., Menard M.K., Herring A.H., Daniels J., Rowley D.L., Halpern C.T. Predicting preterm birth among participants of North Carolina’s Pregnancy Medical Home Program. Matern. Child Health J. 2015; 19(11): 2438-52.
12. Derakhshi B., Esmailnasab N., Ghaderi E., Hemmatpour S. Risk factor of preterm labor in the West of Iran: a case-control study. Iran. J. Public Health. 2014; 43(4): 499-506.
Received 17.05.2018
Accepted 22.06.2018
About the Authors
Marat, Aizada M., PhD, obstetrician-gynecologist, Department of Obstetrics and Gynecology №1, Astana Medical University.010000, Astana, Kazakhstan, Beibitshilik str. 49А. Tel.: +77172539453. E-mail: aizadamarat0708@gmail.com
Ukybassova, Talshyn, MD, professor of the Department of Women’s Diseases, “University Medical Center” National Research Center for Maternal and Child Health.
010000, Astana, Kazakhstan, Turan avenue str. 32. Tel.: +77172701430. E-mail: talshynu@yandex.ru
For citations: Marat A.A., Ukybassova T. The risk factors and pattern of preterm birth in the fetal residents of the Republic of Kazakhstan. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (12): 50-4. (in Russian)
http://dx.doi.org/10.18565/aig.2018.12.50-54



