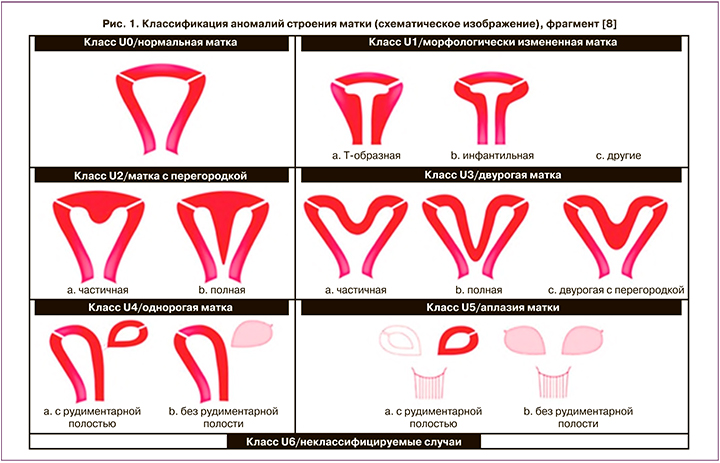
Несмотря на то что в течение последних десятилетий произошло снижение материнской летальности на 77,2% (с 47,4 на 100 тыс. новорожденных в 1990 г. до 10,8 на 100 тыс. новорожденных в 2014 г. в России), среди ее причин второе место (27%) занимают акушерские кровотечения [1]. При отсутствии своевременного оказания специализированной медицинской помощи период времени от момента развития акушерского кровотечения до наступления смерти женщины не превышает 2 ч. Одной из причин развития массивных акушерских кровотечений является нарушенная внематочная (эктопическая) беременность, в том числе беременность в рудиментарном роге матки [2]. Впервые подобная беременность описана в 1669 г. Mauriceau и Vassal [3]. 1:200–1:600 женщин репродуктивного возраста страдают аномалиями развития женских половых органов, среди которых рудиментарный рог матки встречается достаточно редко – 1:100 тыс., что составляет 0,1–3% и является следствием неполного слияния парамезонефральных протоков [4–7]. По классификации ESHRE/ESGE (2013) матка с рудиментарным рогом относится к U4a типу аномалий строения матки (рис. 1) [8].
В рудиментарном роге матки существуют наиболее благоприятные условия для имплантации плодного яйца по сравнению с другими эктопическими локализациями, так как в большинстве случаев слизистая оболочка рудиментарного рога состоит из базального и функционального слоев, последний из которых вследствие процессов секреторной трансформации становится пригодным для полноценной инвазии трофобласта. Тем не менее частота беременности в рудиментарном роге матки составляет 1 на 76–140 тыс. беременностей, что в 10 раз реже фактов наступления абдоминальной беременности и в 1000 раз реже трубной [9, 10].
По данным литературы, полости рудиментарного рога и матки в 72–85% случаев не сообщаются между собой [11–13], однако предполагается, что беременность может наступить и в несообщающемся рудиментарном роге путем трансперитонеальной миграции сперматозоидов или оплодотворенной яйцеклетки [14].
Сообщающийся с полостью рудиментарный рог матки практически никогда не проявляет себя клинически вне беременности, однако в 38% наблюдений его наличие сочетается с аномалиями строения органов мочевыделительной системы. Такие патологические состояния, как заболевания почек в анамнезе, а также бесплодие, дисменорея и невынашивание беременности, должны насторожить врача в отношении возможных аномалий строения матки [15].
Диагностика беременности в рудиментарном роге матки зачастую оказывается сложной задачей. Ультразвуковое исследование (УЗИ) является наиболее распространенным методом визуализации во время беременности по причине своей безопасности, однако неэффективным в 74% наблюдений в отношении диагностики эктопической беременности [16]. При этом с увеличением срока гестации чувствительность ультразвукового метода снижается на 26–29% [17]. Поэтому в последние годы для проведения дифференциального диагноза используют метод магнитно-резонансной томографии (МРТ).
После установления факта прогрессирующей беременности в рудиментарном роге матки единственным методом лечения является хирургическое удаление рога с ипсилатеральной тубэктомией, что поможет избежать спонтанного разрыва стенок плодовместилища с возможными катастрофическими последствиями для пациентки. В 52,4% наблюдений причинами неудач при оказании медицинской помощи выступают запоздалое обращение пациентов, заочное консультирование, неукомплектованность выездных бригад, нарушение принципов маршрутизации, недостаточная квалификация специалистов.
Нами представлены наблюдения прогрессирующей беременности в рудиментарном роге матки, а также нарушенной эктопической беременности посредством разрыва стенок рудиментарного рога с массивным внутрибрюшным кровотечением.
Клиническое наблюдение № 1
Повторнобеременная пациентка С., 21 года, поступила в стационар по направлению врача женской консультации в связи с подозрением на прогрессирующую эктопическую беременность сроком 19–20 недель на основании результатов проведения очередного УЗИ. Пациентка соматически не отягощена, менструальная функция не нарушена, гинекологические заболевания отрицает. Первая беременность в 2017 г. протекала физиологически и завершилась своевременными родами через естественные родовые пути. С начала II триместра настоящей беременности пациентка находилась на учете в женской консультации. Осложнений во время беременности не наблюдалось. При осмотре на момент поступления: состояние пациентки удовлетворительное, жалобы отсутствовали, гемодинамические показатели находились в пределах нормальных значений, живот был мягким, безболезненным при пальпации во всех отделах, перистальтика кишечника обычной звучности, физиологические отправления не нарушены. При пальпации живота под передней брюшной стенкой от верхнего края лобкового симфиза до уровня пупка, больше справа от средней линии определялось плодовместилище с одним плодом. На уровне гребня подвздошной кости по среднеключичной линии справа выслушивалось сердцебиение плода – ясное, ритмичное, частотой 145 в минуту. При проведении бимануального исследования предлежащая часть плода через своды влагалища не определялась. В приемном отделении акушерского стационара произведено УЗИ, при котором определялся один живой плод. По данным фетометрии размеры плода соответствовали гестационному сроку 20 недель. Стенки плодовместилища четко не прослеживались. Плацента толщиной 20 мм располагалась по задней стенке плодовместилища. Слева и кзади от плодовместилища визуализировалось тело матки размерами 88×65×54 мм с четкими контурами. Заключение: «Прогрессирующая эктопическая беременность сроком 19–20 недель».
С целью уточнения локализации и характера плодовместилища произведено МРТ органов малого таза, а также ангиография брюшного отдела аорты и ее ветвей. По данным МРТ (импульсные последовательности T2FASE, T2FSat, DWI) матка находилась в положении anteversio-anteflexio, была несколько увеличена в размерах, полость ее расширена. Толщина миометрия составляла 16 мм. К наружной поверхности матки в области дна, а также к правому яичнику интимно прилежало плодовместилище, содержавшее один плод. По задней стенке плодовместилища располагалась слепая кишка. Плацента прослеживалась по задней стенке плодовместилища с переходом на нижнюю и верхнюю его стенки. В почках, печени, желчном пузыре, селезенке и поджелудочной железе патологических изменений не обнаружено. Тонкий и толстый кишечник интактны. Заключение: «Картина прогрессирующей эктопической беременности».
По данным ангиографии брюшного отдела аорты и ее ветвей (катетеризация общей бедренной артерии по методике Сельдингера, интродьюсер 5 FR, катетер Cobra 2, контрастное средство «Ультравист» 370–200 мл), дополнительных (патологических) ветвей при контрастировании селезеночной, верхней и нижней брыжеечных артерий не определялось. На ангиограмме левой маточной артерии отмечалась гиперваскуляризация матки. На ангиограмме правой маточной артерии визуализировалась крупная ветвь, отходившая к округлому образованию, которое накапливало контрастное вещество.

Принимая во внимание полученные результаты дополнительных методов исследования, консультативно был подтвержден диагноз прогрессирующей эктопической беременности и определена необходимость проведения хирургического лечения. Произведена срединная лапаротомия. Во время ревизии органов брюшной полости обнаружено плодовместилище диаметром до 20 см (рис. 2 [18]), представленное перерастянутыми и истонченными стенками правого рудиментарного рога матки, от которого отходила правая маточная труба и правая круглая связка. Тело матки розового цвета размерами 60×80 мм располагалось слева и кзади от добавочного рога матки с плодом. Рудиментарный рог с правой маточной трубой отсечен от матки. Интраоперационная кровопотеря составила 100 мл.
 При вскрытии полости добавочного рога матки обнаружен нежизнеспособный плод женского пола массой 390 г и длиной 26 см, а также плацента, пуповина и плодные оболочки (рис. 3).
При вскрытии полости добавочного рога матки обнаружен нежизнеспособный плод женского пола массой 390 г и длиной 26 см, а также плацента, пуповина и плодные оболочки (рис. 3).
Послеоперационный период протекал без осложнений. На 6-е сутки пациентка выписана из стационара в удовлетворительном состоянии.
К сожалению, не всегда удается, как в представленном выше наблюдении, выполнить хирургическое лечение пациенток до момента прерывания эктопической беременности, так как лишь 26% беременностей в рудиментарном роге матки диагностируются на этапе их прогрессирования [19]. Традиционно клиническое течение подобного варианта эктопической беременности характеризуется высокой частотой (85%) разрыва стенок добавочного рога на ранних сроках гестации [20]. Условий для пролонгирования беременности в рудиментарном роге матки до состояния жизнеспособности плода, как правило, не хватает по причине довольно низкой растяжимости стенок рога вследствие преобладания соединительной ткани над мышечной, а также по причине недостаточной выраженности сосудистой сети. Тем не менее, в литературе описаны случаи неонатальной выживаемости при беременности в добавочном роге матки [21]. Однако в подавляющем большинстве наблюдений прогрессирующий рост плодного яйца и внедрение ворсин хориона приводит к истончению стенок рога и разрыву плодовместилища [22]. Клинические симптомы нарушенной эктопической беременности в рудиментарном роге матки включают выраженные абдоминальные боли и признаки геморрагического шока, ассоциированные с развитием внутрибрюшного кровотечения.
Клиническое наблюдение № 2
Первобеременная пациентка Ч., 22 лет, доставлена бригадой скорой медицинской помощи в акушерский стационар в тяжелом состоянии с жалобами на выраженную слабость и кинжальные боли в животе, появившиеся внезапно в состоянии покоя. Кожные покровы бледные, дыхание частое, поверхностное, пульс 120 в минуту, нитевидный. Артериальное давление 70/40 мм рт. ст. на обеих руках. Пальпация живота затруднена вследствие выраженности симптомов мышечной защиты. Сердцебиение плода не выслушивалось. При бимануальном исследовании отмечено нависание сводов влагалища с положительными симптомами Болта и Промптова. Выделения из половых путей слизистые. Из анамнеза: пациентка соматически не отягощена, менструальная функция не нарушена, гинекологические заболевания отрицает. С ранних сроков беременности состояла на учете в женской консультации. В начале II триместра проводилось лечение угрожавшего самопроизвольного выкидыша препаратами прогестерона с положительным эффектом. По данным УЗИ органов брюшной полости и малого таза на момент поступления обратило на себя внимание большое количество свободной жидкости в брюшной полости (кровь), а также отсутствие сердечной деятельности плода. Заключение: «Беременность 20–21 неделя. Разрыв матки? Антенатальная гибель плода. Внутрибрюшное кровотечение». Учитывая наличие симптомов геморрагического шока, пациентка транспортирована в операционную, где ей в экстренном порядке произведена нижнесрединная лапаротомия в условиях эндотрахеального наркоза. Развернут аппарат Sell-Saver. В брюшной полости обнаружено около 2000 мл яркой крови со сгустками, а также мертвый плод женского пола массой 430 г, свободно располагавшийся под передней брюшной стенкой вместе с последом. Тело матки размерами 60×55 мм, плотное, розового цвета. В области правого угла матки визуализировались перерастянутые стенки добавочного рога с линейным разрывом (рис. 4), переходящим на правый мезосальпинкс. От стенок рудиментарного рога отходила правая маточная труба. Добавочный рог вместе с маточной трубой отсечен от матки, выполнена метропластика. Общая кровопотеря составила 3000 мл. Произведена аутогемотрансфузия в объеме 1020 мл.

Лечение пациентки в послеоперационном периоде осуществлялось в условиях отделения реанимации и интенсивной терапии с последующим переводом в гинекологическое отделение. Через неделю пациентка выписана из стационара в удовлетворительном состоянии.
Заключение
Благоприятный исход в рамках прогноза для жизни, здоровья и сохранения репродуктивной функции у данных пациенток оказался возможным по причине своевременно и адекватно оказанной медицинской помощи. Нельзя не отметить тот факт, что обе пациентки – молодые, здоровые и социально адаптированные женщины, которые состояли на учете по беременности в женской консультации, где им неоднократно проводились осмотры и ультразвуковые исследования. В анамнезе одной из пациенток имела место беременность, завершившаяся родами через естественные родовые пути без осложнений. Другой пациентке на гестационном сроке 14 недель проводилась терапия, направленная на пролонгирование беременности, которая в конечном счете оказалась эктопической. При регулярном посещении женской консультации ни обе эти пациентки, ни наблюдавшие их акушеры-гинекологи не подозревали о существовании беременности в рудиментарном роге матки.
Удаление добавочного рога до наступления беременности позволило бы избежать непосредственной угрозы для жизни таких пациенток. Об эктопической беременности всегда следует помнить при так называемой нетипичной ультразвуковой картине. В подобных ситуациях по жизненным показаниям необходимо проводить диагностику с использованием высокотехнологичных методов визуализации. Для предотвращения материнской смертности, связанной с последствиями нарушенной эктопической беременности, важно осуществлять дифференцированный подход к ведению каждой пациентки с учетом факторов риска и клинических особенностей на основании грамотной интерпретации результатов лабораторных и инструментальных методов исследования.



