В настоящее время накоплены убедительные данные о том, что цервиковагинальные инфекции во время беременности являются причиной осложнений гестационного периода и неблагоприятных перинатальных исходов [1–4]. Особое значение придают генитальным инфекциям на ранних сроках беременности, как триггеру иммунопатологических нарушений, приводящих к формированию «больших акушерских синдромов» [5].
Несмотря на современные диагностические технологии и принятую концепцию двухэтапного лечения цервиковагинальных инфекций, сохраняется высокая частота их рецидивов [6]. Причинами рецидивирующего течения заболевания могут являться применение препаратов без доказанной эффективности, а также отсутствие или неадекватное восстановление микробиоценоза влагалища после использования антимикробных препаратов. Последнее важно с точки зрения современных представлений о роли нормального микробиоценоза влагалища в противоинфекционной защите репродуктивного тракта женщины [1].
Для восстановления микробиоценоза влагалища наиболее часто используются две группы лекарственных средств: препараты, способствующие закислению влагалищной среды, и пробиотики [7, 8, 9]. Наиболее популярными и широко изученными являются пробиотические препараты, обладающие антагонистической активностью против условно-патогенных и патогенных микроорганизмов [9]. Помимо прямой бактерицидной активности, пробиотические штаммы оказывают стимулирующее влияние на колонизационную резистентность слизистых желудочно-кишечного тракта и влагалища, моделируют местный секреторный иммунитет [10]. Одним из направлений восстановления влагалищной микрофлоры является программированное подкисление влагалищной среды, что достигается интравагинальным введением кислотосодержащих препаратов. Проведены исследования по изучению роли молочной кислоты в поддержании вагинального гомеостаза, в которых акцентировано внимание на иммунокорригирующих и антибактериальных свойствах, что обосновывает ее применение в практике как физиологический способ уменьшения рН влагалищного содержимого, подавляющий размножение анаэробной условно-патогенной микрофлоры, создающий оптимальные условия для роста собственного пула лактобактерий [7, 11, 18].
Учитывая, что в результате воздействия антимикробных препаратов изменяется вагинальная микрофлора [12], оценка ее состояния может быть одним из критериев выбора метода для восстановления нормального вагинального микробиоценоза: использование препарата лактобактерий или ацидификация вагинальной среды.
Цель исследования – разработать и оценить эффективность дифференцированной коррекции микробиоценоза влагалища у женщин с неспецифическим цервиковагинитом в I триместре беременности.
Материалы и методы
Для характеристики вагинальной микрофлоры (световая микроскопия, ×1000, окраска по Граму) после применения антисептика деквалиния хлорида на первом этапе терапии цервиковагинита неспецифической этиологии проведено проспективное исследование с участием 25 пациенток. Критерии включения в исследование: спонтанная одноплодная беременность на сроке до 13–14 недель, цервиковагинит неспецифической этиологии, подписанное информированное согласие на участие в исследовании.
Диагноз цервиковагинита основывался на данных объективного осмотра (гиперемия, отек слизистой оболочки влагалища и шейки матки, патологические выделения из половых путей) и результатах микроскопического исследования отделяемого влагалища и шейки матки. Определение этиологии заболевания проводили по результатам культурального исследования материала из влагалища и цервикального канала. На основании полученных данных о состоянии вагинальной микрофлоры после первого этапа терапии предложена дифференцированная коррекция микробиоценоза влагалища, оценка эффективности которой была проведена в рандомизированном клиническом исследовании с участием 50 беременных женщин с цервиковагинитом неспецифической этиологии в I триместре беременности. Лечение проводилось двухэтапно: на первом этапе всем пациенткам назначался разрешенный по инструкции к использованию в I триместре беременности антисептик деквалиния хлорид (по 1 таблетке интравагинально – 6 дней). Перед проведением 2-го этапа случайным образом были сформированы 2 группы. Пациентки обеих групп были сопоставимы по анамнестическим данным и клиническим проявлениям цервиковагинальной инфекции. В основной группе (n=24) пациенткам проводилось дополнительное микроскопическое исследование вагинального отделяемого (увеличение ×1000, окраска по Граму) после лечения антисептиком, по результатам которого дифференцированно назначали препарат 2-го этапа. Пациенткам из группы сравнения (n=26) восстановление микробиоценоза влагалища проводили без учета состояния микрофлоры. Для восстановления состояния нормоценоза влагалища применяли лекарственное средство, содержащее молочную кислоту и гликоген (интравагинально по одному тюбику – 7 дней), или препарат лиофилизированной культуры лактобактерий L. casei rhamnosus Doderleini (интравагинально по 1 капсуле 2 раза в день 7 дней). Эффективность предложенного метода оценивали по частоте развития рецидивов цервиковагинита.
Статистический анализ данных проводили с помощью редактора данных IBM SPSS Statistics 12.1. Номинальные признаки приведены в абсолютных значениях и относительной частоте встречаемости, различия в группах оценивались по критерию χ2 Пирсона. В связи с несоответствием полученных данных нормальному закону распределения количественные и порядковые показатели представлены в виде медианы (Ме), 25 и 75 квартилей. Межгрупповую оценку различий проводили непараметрическим критерием Манна–Уитни. Достоверными считали значения р≤0,05.
Результаты и обсуждение
После проведенного лечения антисептиком у 25 беременных с неспецифическим цервиковагинитом в I триместре беременности на основании детального бактериоскопического качественного и количественного изучения грампозитивных палочек было выявлено три варианта состояния вагинальной микрофлоры. 1-й вариант (28% женщин) – визуализировались мономорфные грамположительные палочки от 11 до 100 в поле зрения. В образцах 44% женщин – 2-й вариант – выявлялись полиморфные грамположительные палочки в количестве от 11 до 100 в поле зрения. При 3-м варианте (28% случаев) в мазках определялись полиморфные грамположительные палочки в количестве 10 и менее в поле зрения.
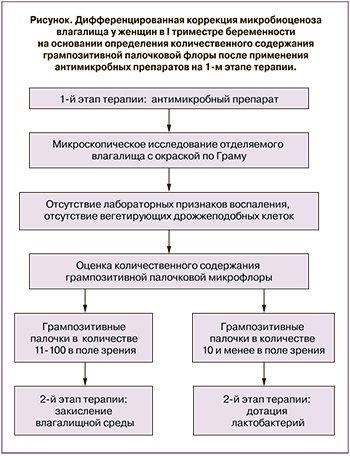 На основании полученных данных был разработан алгоритм дифференцированной коррекции микробиоценоза влагалища (рисунок).
На основании полученных данных был разработан алгоритм дифференцированной коррекции микробиоценоза влагалища (рисунок).
Незначительное количество грампозитивных палочек (при микроскопии единичные клетки в мазке или их отсутствие) после применения антисептика можно рассматривать как показание для дотации культуры лактобактерий, тогда как при умеренном количестве грампозитивных палочек будет достаточным использование кислотосодержащих препаратов.
Эффективность предложенной дифференцированной коррекции микробиоценоза влагалища при двухэтапной терапии неспецифического цервиковагинита у женщин в I триместре беременности оценивали по результатам рандомизированного клинического исследования с участием 50 пациенток.
После лечения рецидивы цервицита или цервиковагинита возникали в обеих группах: через 16 (9…16) недель – в основной и 15 (10,5…19,75) недель – в группе сравнения. Однако в основной группе, где лечение проводилось с дифференцированным подходом, повторные эпизоды отмечены в 12,5% случаев, тогда как в группе сравнения частота рецидивов была достоверно выше и составила 38,5% (р=0,037).
Впоследствии во время беременности после проведенной терапии у пациенток отмечали дисбиоценоз влагалища (обнаружение условно-патогенной флоры в титрах более 104 КОЕ /мл и снижение титра лактофлоры по результатам бактериологического исследования отделяемого влагалища и отсутствие клинических проявлений инфекционного процесса) у 26,9% обследуемых группы сравнения и у 8,3% беременных основной группы. Бактериальный вагиноз диагностировали в 7,7% случаев только у беременных группы сравнения.
У пролеченных женщин отмечался незначительный процент плаценто-ассоциированных осложнений: у трети беременных регистрировали проявления плацентарной недостаточности (25,0% женщин основной группы и 34,6% пациенток группы сравнения); умеренная преэклампсия диагностирована у 4,2% и 7,7% обследованных (основная и группа сравнения соответственно), что может быть связано со своевременной диагностикой цервиковагинита и проведением двухэтапного лечения на ранних сроках беременности. Госпитализации по поводу угрожающих преждевременных родов отмечены у 12,5% женщин основной группы и 19,2% пациенток группы сравнения. Маловодие регистрировалось несколько чаще у женщин основной группы – в 12,5% случаев и у 7,7% беременных группы сравнения, многоводие регистрировалось только у 7,7% женщин группы сравнения. Среди других осложнений беременности отмечено обострение инфекционной патологии мочевыводящих путей (20,8% и 38,5% случаев соответственно).
В группе сравнения, где лечение проводилось без дифференцированного подхода, беременность закончилась преждевременными родами в 19,2% случаев, тогда как в основной группе все роды были своевременными (р=0,05).
У новорожденных от матерей основной группы и группы сравнения в единичных случаях выявлен врожденный порок развития сердечно-сосудистой системы (4,2% и 3,8% соответственно). В структуре осложнений раннего неонатального периода у новорожденных от матерей из группы сравнения были зафиксированы: церебральная ишемия (15,4%), респираторный дистресс-синдром (7,7%), внутриутробные инфекции (7,7%), задержка внутриутробного развития (3,8%).
Обсуждение
На сегодняшний день вагинальная микрофлора, являясь одним из факторов колонизационной резистентности слизистой оболочки влагалища, является первой линией противоинфекционной защиты нижнего одела репродуктивного тракта [1, 11]. Поскольку возникновение инфекционного процесса приводит к изменению качественного и количественного состава лактофлоры, а также учитывая влияние антимикробных препаратов, очевидна необходимость коррекции резидентной микрофлоры при лечении цервиковагинальных инфекций [5, 10]. Установлено, что проведение двухэтапного лечения отражается на успешности проведенной терапии, в частности, приводит к снижению частоты рецидивов цервиковагинальных инфекций [13–17]. При этом остается открытым вопрос выбора препарата для восстановления нормальной микрофлоры влагалища. Учитывая персонифицированную направленность современной медицины, необходимо дифференцировано, с учетом состояния микробиоценоза влагалища, восстанавливать его нормоценоз.
В данном исследовании для оценки состояния вагинальной микрофлоры было отдано предпочтение микроскопической оценке, как одному из доступных способов, принимая во внимание наименьшие временные и материальные затраты, а также возможность получить целостную картину микробиоценоза влагалища, включая оценку эпителиальных клеток и лейкоцитарной реакции. Результаты проведенных нами исследований показали, что применение антисептика при лечении цервиковагинальных инфекций отражается на состоянии резидентной микрофлоры. Таким образом, дотация лактобактерий целесообразна при определении грампозитивных палочек в количестве менее 10 в поле зрения. При наличии грампозитивных полиморфных палочек в достаточном количестве можно прибегнуть к закислению влагалищной среды.
Такой дифференцированный подход позволяет в 3 раза снизить частоту возникновения рецидивов воспалительных инфекционных процессов слизистой оболочки влагалища и шейки матки у женщин во время беременности. Вместе с тем применение данного алгоритма также снижает частоту развития дисбиотических состояний влагалища в течение беременности.
Не было выявлено значимых различий в частоте осложнений гестационного периода у обследованных пациенток. Обращает на себя внимание невысокая частота возникновения таких осложнений, как преэклампсия, плацентарная недостаточность, у женщин с цервиковагинитом в I триместре беременности, пролеченных своевременно, сразу после установления диагноза. Тем не менее в группе, где двухэтапное лечение проводилось без дифференцированного подхода к выбору метода восстановления микробиоценоза влагалища, в 19,2% случаев регистрировались преждевременные роды. Большой процент преждевременных родов в группе сравнения можно объяснить рецидивирующим течением цервиковагинита и наличием дисбиотических состояний у обследованных женщин.
Заключение
Таким образом, данное исследование позволило выявить три варианта состояния вагинальной микрофлоры после применения антисептика на 1-м этапе терапии цервиковагинита неспецифической этиологии у женщин в I триместре беременности. Проведение дифференцированной коррекции микробиоценоза влагалища с учетом состояния микрофлоры влагалища позволяет снизить частоту рецидивов цервиковагинальных инфекций и профилактировать преждевременные роды.