COVID-19 in pregnant women of Siberia and the Russian Far East: 2-year results of the pandemic
Objective: To assess the morbidity, clinical course, maternal and perinatal outcomes of the new coronavirus infection COVID-19 in pregnant women in the Far Eastern and Siberian Federal Districts based on the results of 2020–2021. Materials and methods: The latest information on COVID-19 in pregnant women, women in labor and women who recently gave birth was analyzed. The findings were presented by the chief obstetricians-gynecologists of the regions in the period from March 11, 2020 to December 25, 2021. Results: A total of 27,210 cases of COVID-19 in pregnant, parturient and puerperal women were registered during the 2-year pandemic. The morbidity rate in these women was 2.4 times higher compared to the general population: 18988.0 vs 8019.5 per 100,000 people. SARS-CoV-2 infection was asymptomatic in 24.2% of mothers; it was mild in 50.0%, moderate in 21.3%, severe in 3.7%, and extremely severe in 0.8%. Pregnant women were more often hospitalized and stayed in intensive care and anesthesiology units compared to patients in the general population (5.5% vs 1.9%, p<0.001), and invasive mechanical ventilation (IMV) was used less often (0.7% vs 1.4%, p<0.05). There were 6,416 (23.6%) patients who gave birth to 6,512 children. Preterm delivery was in 18.5% (6.1% in Russia); cesarean sections – 38.8% (30.1% in Russia); operative vaginal delivery – 0.3% (0.13% in Russia). There were 81 (0.3%) deaths among mothers with COVID-19 (2.5% of cases among the population, p<0.001). Perinatal losses were registered in 156 cases (2.4%): stillbirths – 141 (2.17%), early neonatal mortality – 15 (0.23%). COVID-19(+) was revealed in 165 (2.5%) newborns. Conclusion: The incidence of COVID-19 in pregnant women was significantly higher than in general population during the 2-year pandemic, but the disease is characterized by more frequent hospitalization to intensive care and anesthesiology units, by lower demand for IMV and lower mortality rate. The second year of the pandemic was characterized by a more unfavorable course of COVID-19 in mothers and by an increase in the severe forms of the disease and indicators of maternal and perinatal mortality. The rates of preterm delivery and cesarean section in patients with COVID-19 were higher than in the general population. The incidence of SARS-CoV-2 virus isolation in newborns decreased significantly (from 6.2 to 2.5%). Further studies in this area are necessary. The morbidity rate of COVID-19 in pregnant women in Siberia and the Far East is higher than in the general population, but the disease is characterized by a lower need for IMV and a lower mortality rate. The rates of preterm birth and cesarean section are higher in patients with COVID-19 than in the general population. Finding of the SARS-CoV-2 RNA in newborns suggests vertical transmission of the infection.Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I.
Keywords
New coronavirus infection caused by the SARS-CoV-2 virus (Severe Acute Respiratory Syndrome Coronavirus 2) has continued to pose a significant global health threat for two years. The pandemic began in December 2019 in Wuhan of Hubei Province (China) and rapidly spread to all countries of the world due to active migration of the population and highly contagious causative agent [1, 2].
The World Health Organization (WHO) gave the official name to the infection caused by the new coronavirus COVID-19 (Coronavirus disease 2019) on February 11, 2020. The International Committee on Taxonomy of Viruses named the causative agent of infection as SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) [3].
According to the world data on morbidity, the epidemic has been actively developing for two years and its peak values were reached in the second half of 2021 [4].
The WHO made an official statement about the beginning of the COVID-19 new coronavirus infection pandemic on March 11, 2020. Since then, more than 386 million of confirmed cases of COVID-19 have already been registered in the world, including 5.7 million of cases with a fatal outcome [5].
During these two years of the pandemic, the SARS-CoV-2 virus mutated many times; its new strains resulted in new epidemic increases in morbidity, sometimes all over the world [6, 7].
In addition, the mutation in the coronavirus S-protein caused more virulent and pathogenic strains than the zero Wuhan virus that spread from China. These strains significantly increased the prevalence and mortality in the population and were classified as VOC (Variant of concern) by the WHO [8]. The first strain in this classification was alpha (Great Britain), then beta (South Africa), gamma (Brazil) and delta (India). The omicron variant which was first reported on November 25, 2021, is also classified as VOC [7, 8].
Initially, COVID-19 was not considered to have a higher virulence in women during pregnancy, childbirth and in the postpartum period [9]. However, VOC strains of the SARS-CoV-2 virus began to affect not only elderly and somatically ill people, as it was at the beginning of the pandemic, but also pregnant women, newborns, children, adolescents, and healthy young people [3, 7, 10].
The results which were obtained after the analysis of the outcomes of other pandemics of respiratory viral infections in the XX century and the beginning of the XXI century show a higher morbidity and mortality among pregnant, parturient and puerperal women. The percentage of maternal deaths during the Spanish flu pandemic in 1918–1920 was 27–50%, SARS-CoV – 25–30%, MERS – 40%; mortality rate of pregnant, parturient and puerperal women in influenza A(H1N1) was 2.5 times higher than in the general population [11, 12].
During the first year of the pandemic of a new coronavirus infection, we revealed some differences in the development of the infections. Thus, the proportion of maternal deaths was 13.9 times lower than among the general population, while morbidity was 2.5–3.0 times higher like in previous large-scale epidemics [13, 14].
Currently, there is enough information in the world scientific literature on morbidity and mortality of pregnant, parturient and puerperal women, as well as other categories of the population during the first year of the COVID-19 pandemic [13–26]. At the moment, the SARS-CoV-2 virus epidemic is not over yet and it is necessary to analyze and systematize all the obtained information.
The aim of the study is to assess the morbidity, clinical course, maternal and perinatal outcomes of the new coronavirus infection COVID-19 in pregnant women in the Far Eastern and Siberian Federal Districts based on the results of 2020–2021.
Materials and methods
The latest information on COVID-19 in pregnant women, women in labor and women who recently gave birth was analyzed. The findings were presented by the chief obstetricians-gynecologists of the Far Eastern and Siberian Federal Districts in the period from March 11, 2020 to December 25, 2021.
SARS-CoV-2 virus was identified using nasopharyngeal PCR-test [3, 10]; testing rates in the general population and pregnant women of both federal districts were comparable.
Statistical analysis
Statistical data processing was carried out using the IBM SPSS Statistics Version 25.0 software package (International Business Machines Corporation, USA). Qualitative data are presented as the number n and percentage % (the number of patients with this parameter, the percentage of their number in the group). The mathematical analysis included methods of descriptive statistics, assessment of the difference (pattern of change) between the parameters for the first year and for two years of the pandemic (delta, ∆), analysis of the contingency tables with the assessment of χ2 value and significance level (p). The values were considered statistically significant at p≤0.05.
Results and discussion
The total number of the confirmed COVID-19 cases, the number of COVID-19 cases in pregnant women, women in labor and women who recently gave birth in the Far Eastern and Siberian Federal Districts are presented in Table 1.
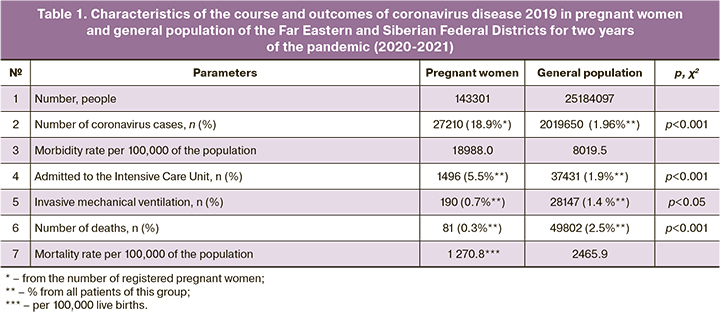
The second year of the COVID-19 pandemic is characterized by a higher morbidity rate of the population. The morbidity rate in the general population of the Far Eastern Federal District and the Siberian Federal District (25,184,097 people) was 1960.8 per 100,000 people, according to the data on December 25, 2020 (Far Eastern Federal District – 2294.6; Siberian Federal District – 1801.7). It increased by 4.1 times and amounted to 8019.5 per 100, 000 people as of December 25, 2021 (Far Eastern Federal District – 8172.4; Siberian Federal District – 7946.6).
In terms of the dynamics of the epidemic process, the infectious disease became more severe, there were more patients with pneumonia, namely 16.3 and 23.6% (∆+7.3%; respectively, as of December 25, 2020 and December 25, 2021); the number of patients who underwent invasive mechanical ventilation (IMV) was 1.05 and 1.39% ((∆+0.34%, respectively). The proportion of patients hospitalized in intensive care units (ICU) decreased slightly from 2.24% to 1.85% (∆-0.39%), which was due to a change in indications and criteria regulated by the first and subsequent versions of temporary guidelines [3].
COVID-19-related mortality rate in the population of both federal districts increased from 1.95 to 2.47% (∆+0.52%; in the Far Eastern Federal District from 1.25 to 1.67%; in the Siberian Federal District from 2.36 to 2.86%). Therefore, new coronavirus infection was more severe in the general population of Siberia and Far East in the second year of the pandemic than in the first one.
The analysis of the morbidity rate and clinical course of COVID-19 in pregnant, parturient and puerperal women of the Siberian and Far Eastern Federal Districts for 2021 also indicates an increase in the activity of the epidemic process, an increase in the number of cases of severe course and adverse outcomes.
During the first year of the pandemic, the SARS-CoV-2 virus was confirmed in 8485 pregnant, parturient and puerperal women (3267 in the Far Eastern Federal District, 5218 in the Siberian Federal District), which accounted for 5.9% pregnant women registered at antenatal clinics and 1.71% of the total population infected with the disease. By the end of the second year, the total number of pregnant, parturient and puerperal women with COVID-19 was 27,210 cases, including 11108 (40.8%) patients in the Far East and 16102 (59.2%) patients in Siberia.
The comparison of the data of December 2020 [14] and December 2021 showed a 3.2-fold increase in the number of women with COVID-19 (+220.7%; 27210 vs 8485), the proportion of pregnant women with SARS-CoV-2 was 19.0% (27210/143301) vs 5.9% (8485/143010) and the morbidity rate was 18988.0 vs 5933.2 per 100,000 pregnant, parturient and puerperal women.
The analysis of the whole pandemic period showed that the morbidity rate of COVID-19 in pregnant women was many times higher than one in the general population: 5933.2 vs 1960.8 per 100,000 people in 2020, a 3.0–fold increase; 18988.0 vs 8019.5 per 100,000 people by the end of 2021; a 2.4-fold increase.
Clinical symptoms of the disease were absent in 27.4% (2324/8485) of women infected with SARS-CoV-2 in 2020 and in 24.2% (6583/27210) in 2021, i.e. the proportion of patients with asymptomatic infection decreased by 2.8%.
According to a large-scale monitoring in 2020, there were 461,825 women with COVID-19 confirmed in the laboratory, 11.3% (52,363) of pregnant women had an asymptomatic course of the infection [15]. The meta-analysis conducted by I. Bellos et al. (2021) showed a similar result of 15% [18]. According to the results of a systematic review by M. Papapanou et al. (2021) which included 13 studies, the incidence of asymptomatic forms varied from 7.5 to 32.6% [21]. In the study published by the National Institute of Child Health and Human Development (NICHD, Eunice Kennedy Shriver, USA), a significantly high proportion of women (from 14 states of USA) infected with SARS-CoV did not have symptoms, namely 47% [23].
According to the results obtained in December 2020 and December 2021, about half of the patients in Siberia and the Far East had a mild form of the disease: 53.0% (4471/8485) and 50,0% (∆-3,0%; 13603/27210), respectively. The proportion of women with a more severe course of the new coronavirus infection was significantly less, however, by the end of the second year of the pandemic, moderate forms were more often recorded, namely, 16.6% (1388/8485) and 21.3% (∆+4.7%; 5806/27210); severe course was revealed in 2.5% (210/8485) and 3.7% (∆+1.2%; 1004/27210) of cases and critical conditions were detected in 0.5% (39/8485) and 0.8% (∆+0,3%; 214/27210) of cases, respectively. According to the national observational study in the USA (2021), the incidence of mild and moderate forms of infection in pregnant women was lower and amounted to 27 and 14%, respectively, while the proportion of patients with severe and critical condition was many times higher than our results, and was equal to 8 and 4%, respectively [23].
The severity of the course of the new coronavirus infection in pregnant women in the Far Eastern and Siberian Federal Districts during the 2-year COVID-19 pandemic is shown in Figure.
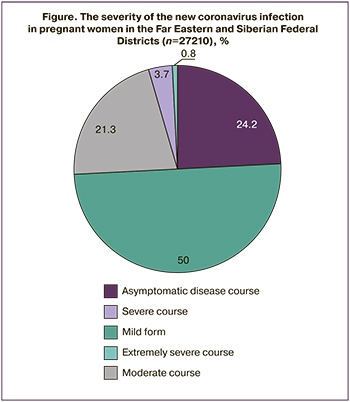
Thus, during the above-mentioned period of the new coronavirus infection pandemic, a large proportion of women (74.2%) had no symptoms of the infectious process (24.2%) or the symptoms were mild (50.0%). However, there was an increase in the rate of moderate, severe and extremely severe course of the disease during the second year of the pandemic in comparison with the first one: 25.8% (7024/27210) vs 19.6% (1637/8485; ∆+6.2%).
In 2020, 3.57% (303/8485) of pregnant, parturient and puerperal women with COVID-19 were treated in ICU; 0.48% (41/8485) underwent treatment with IMV. The proportion of pregnant women hospitalized in ICU was statistically significantly higher in comparison with general population, 3.57% (303/8485) vs 2.24% (1811/80771, p<0.001), however they required IMV less often, namely 0.48% (41/8485) vs 1.05% (845/80771, p<0.001). By the end of 2021, these trends persisted, but their indicators increased: pregnant women were still more likely to undergo treatment in ICU, namely 5.5% (∆+1.93%; 1496/27 210) vs 1.9% (∆-0.34%; 37431/2019650, p<0.001) and needed IMV less often, 0.7% (+0.22%; 190/27210) and 1.4% (+0.35%; 28147/2019650; p<0.001), pregnant women and general population, respectively.
Different modern literature sources provide controversial information on the severity of COVID-19, ICU admission rate and the need for IMV among pregnant women in different countries.
According to a systematic review conducted in 2021 which included 23 studies, ICU admission rate among women ranged from 3% (323/10901 (the largest sample)) to 28.5% (53/186). After the analysis of the quality of the studies, the indicators fluctuated in the range of 3–10% and the largest sample was still at the level of 3% [21]. According to the review of 18 scientific publications, the indicators of IMV in women ranged from 1.4% (155/10713) to 12% (5/41); after the analysis of the quality of the studies, the rate of IMV was 1.4–5.5% and the parameter of 1.4% was characteristic of the largest sample [21]. The Brazilian researchers showed that pregnant women and women in labor had a higher risk of ICU admission (RR=1.60; 95% CI: 1.45–1.77) and receiving IMV treatment (RR=2.02; 95% CI: 1.78–2.30) [22].
During the first year of the pandemic, 2373 (27.97%) women with confirmed SARS-CoV-2 infection gave birth; during the second year of the pandemic, their number was 6416 (23.6%).
The pregnancy outcomes for mother and child in 27210 women with confirmed SARS-CoV-2 infection are presented in Table 2.
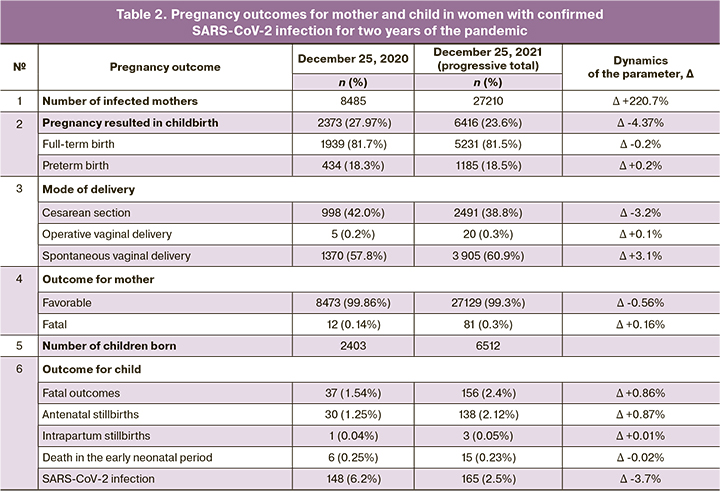
Pregnancy ended in childbirth in 6416 (23.6%) out of 27210 patients with new coronavirus infection. Most of women had a full-term birth – 81.5% (5231/6416), the share of preterm births was 18.5% (1185/6416), which is significantly higher than the national indicator – 6.1% [27].
The results of foreign studies also indicate that maternal infection from COVID-19 is associated with a higher risk of preterm birth. First of all, this is due to the influence of an infectious disease and a developed systemic inflammatory response [10, 28]; secondly, the severe and critical condition of the mother and obstetric and perinatal complications associated with this condition may require preterm delivery [3, 10, 16–19, 21, 23].
The meta-analysis conducted by M. Jafari et al. (2021) showed that the rate of preterm birth in patients with COVID-19 (121 studies, 10,000 pregnant women) was 25.0%, and their relative risk (RR) was 2.5 (95% CI: 1.5–3.5) [19]. The analysis of 42 studies involving 438,548 pregnant women with new coronavirus infection (2021) also revealed an increased preterm birth rate (RR=1.82; 95% CI: 1.38–2.39) [29]. The systematic review of 32 studies conducted by M. Papapanou et al. (2021) showed that preterm birth rate ranged from 14.3% (86/602) to 63.8% (30/47); however, after the assessment of the results of only moderate and high-quality studies, the range of indicators changed from 20.6 to 63.8% [21]. J. Yang et al. (2022) compared the pre–pandemic and pandemic periods and revealed a decrease in the rate of spontaneous preterm birth (RR=0.91; 95% CI: 0.88–0.94) [26].
The rate of cesarean section delivery in patients with COVID-19 decreased during the two years of the pandemic: it was 42.0% on December 25, 2020 (998/2373), and 38.0% on December 25, 2021 (∆-3,2%; 2491/6416). This decrease is due to the wait-and-see obstetric tactics which was used in severe forms of the course of the disease [10]. The rate of operative vaginal delivery (vacuum extraction, use of obstetric forceps) increased from 0.2% (5/2373) to 0.3% (20/6416) in the period 2020-2021. According to the Ministry of Health of the Russian Federation, the rate of cesarean section delivery in 2020 was 30.4%, vacuum extraction 0.13%, use of obstetric forceps 0.005% [27].
The findings of a large-scale meta-analysis conducted in 2021 revealed that the risk for operative vaginal delivery was not increased in women with new coronavirus infection (RR=1.06; 95% CI: 0.97-1.15; p=0.22) [30]. At the same time, most foreign researchers identified the association of this infectious disease with an increased risk of cesarean section. According to the meta-analysis performed by M. Jafari et al. (2021), pregnant women with COVID-19 had cesarean section in 48%, which is significantly higher than uninfected women (RR=3.0; 95% CI:2.0–5.0) [19].
According to a systematic review of 35 studies by M. Papapanou et al. (2021), the rate of cesarean section delivery ranged from 52.3% (390/746) to 95.8% (46/48); after the assessment of the results of only moderate and high-quality studies, the range changed slightly (52.3–94.0%) [21].
According to I. Bellos et al. (2021), the high rate of cesarean section delivery in SARS-CoV-2-positive mothers is mainly due to fears of infecting the babies [18]. However, the majority of researchers does not share this point of view and suggest that this fact is due to an increase in the rate of critical conditions of the fetus and mother with COVID-19 [10, 14, 16, 17, 19].
The analysis of the 2-year epidemic period showed that there were 81 (0.3%) cases of maternal mortality from new coronavirus infection: 12 out of 8485 (0.14%) pregnant, parturient and puerperal patients died in the first year of the pandemic; 69 out of 18275 (0.37%; χ2=10.1; p=0.001) died in the second year. The mortality rate in the general population was statistically significantly higher: it was 1.95% in 2020 (496170/25304117) and 2.5% (49802/2019650, p<0.001) by the end of 2021.
The meta-analysis of 27 studies (2021) revealed that the mortality rate in the maternal group did not exceed 2%, and after low-quality studies were excluded, the rate turned out to be <2%, while the indicator in the largest sample was equal to 0.6% [21]. B. Chmielewska et al. (2021) showed in a large-scale meta-analysis that the risk of maternal mortality during the pandemic increased significantly (RR=1.37; 95% CI: 1.22–1.53; p<0.0001) [30]. According to the national cohort study in the USA (2022), mortality rate of mothers with COVID-19 was 147 (95% CI: 3.0–292.0) vs. 2.5 in uninfected pregnant women (95% CI: 0–7.5) per 100,000 women in the corresponding groups [31].
Perinatal mortality rate in mothers with SARS-CoV-2 infection confirmed in the laboratory was 15.40 deaths per 1000 births (37/2403; 1.54%) at the end of the first year of the pandemic, and 23.96 deaths per 1000 births (156/6512; 2.4%) at the end of the second year of the pandemic (Table 2). The increase in this indicator by 1.6 times occurred due to an increase in the number of cases of antenatal losses, which resulted from the increased rate of severe course of the new coronavirus infection in mothers. Among the causes of perinatal mortality, antenatal stillbirth rate was the highest and increased from 12.48 deaths per 1000 births (30/2403; 1.25%) to 21.19 deaths per 1000 births (138/6512; 2.12%). The rate of intranatal mortality was significantly lower and relatively stable: 0.42 deaths per 1000 births (1/2403; 0.04%) and 0.46 deaths per 1000 births (3/6512; 0.05%). The loss rate in the early neonatal period decreased slightly: 2.50 deaths per 1000 births (6/2372; 0.25%) and 2.30 deaths (15/6512; 0.23%), respectively, in 2020 and 2020–2021.
The results of our study are consistent with the conclusions of the meta-analysis of 26 studies in 2021, where the rates of stillbirth did not exceed 2.5% and varied in the largest samples with medium and high-quality design from 0.6 to 2.4% [21]. According to the conclusions of two meta-analyses in 2021, the risk of stillbirth in mothers with new coronavirus infection was increased in comparison with uninfected pregnant women and amounted to 1.28 (95% CI: 1.07–1.54) (40 studies) [30] and 2.11 (95% CI: 1.14–3.90) (42 studies) [29].
The data published at the time of our analysis showed that the mortality rate of infants born to mothers with COVID-19 in the early neonatal period in other countries ranged from 0.3 to 2.4%, while this indicator was 0.3% in the most numerous study (6/1728) [21]. In the Far Eastern and Siberian Federal Districts, no death was directly associated with neonatal SARS-CoV-2 infection, and this fact is emphasized by other authors [21]. T.D. Metz et al. (2021) concluded that the increased risk of perinatal complications is due to the severe and critical condition of the mother which was caused by COVID-19 [23].
The results of our study confirmed the data obtained in other countries on the possibility of vertical transmission of the SARS-CoV-2 virus from mother to child [9, 12, 17–21]. Given that anti-epidemic measures in childbirth and isolation of mother and baby were implemented according to the temporary guidelines, there were 6.2% (148) of SARS-CoV-2-positive newborns in the first year of the pandemic; the proportion of newborns decreased significantly and was 2.5% in total (165) during the second year.
The meta-analysis by M. Jafari et al. (2021) which included studies in the first year of the pandemic showed that the birth rate of SARS-CoV-2-positive newborns in infected mothers was 8% (4–16%) [19].
The systematic review of 28 studies conducted by M. Papapanou et al. (2021), the proportion of infants with a positive PCR test ranged from 1.6% (4/256) to 10% (7/68). After the analysis of moderate and high-quality studies, the range of fluctuations was 2–7%, while the indicator of 2.5% was characteristic of the largest group [21] and was consistent with the data we obtained in Siberia and the Far East.
It was particularly noted by I. Bellos et al. (2021) that the rate of vertical perinatal transmission did not differ between women admitted to the intensive care unit and women with mild forms of the disease (RR=1.94; 95% CI: 0.50–7.60); there was no correlation with the age of the mother, pregnancy complications or concomitant diseases, except for hypothyroidism in the mother (RR=36.67; 95% CI: 5.56–241.69, p=0.004) [18].
Conclusion
The incidence of COVID-19 in pregnant women was significantly higher than in general population during the 2-year pandemic, but the disease is characterized by more frequent hospitalization to intensive care and anesthesiology units, by lower demand for IMV and lower mortality rate. The second year of the pandemic was characterized by a more unfavorable course of COVID-19 in mothers and by an increase in the severe forms of the disease and indicators of maternal and perinatal mortality. The rates of preterm delivery and cesarean section in patients with COVID-19 were higher than in the general population. The incidence of SARS-CoV-2 virus isolation in newborns decreased significantly (from 6.2 to 2.5%). Further studies in this area are necessary.
References
- Выступление Генерального директора ВОЗ на пресс-брифинге по коронавирусной инфекции 2019-nCoV 11.02.2020. Доступно по: https://www.who.int/ru/dg/ speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 [WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. Available at: https://www.who.int/ru/dg/speeches/detail/who-director-general-s-remarks-at-themedia-briefing-on-2019-ncov-on-11-february-2020 (in Russian)].
- Попова А.Ю., Ежлова Е.Б., Мельникова А.А., Андреева Е.Е., Комбарова С.Ю. и др. Коллективный иммунитет к SARS-CoV-2 жителей Москвы в эпидемический период COVID-19. Инфекционные болезни. 2020; 18(4): 8-16. [Popova A.Yu. Yezhlova E.B., Melnikova A.A., Andreeva E.E., Kombarova S.Yu. et al. Collective immunity to SARS-CoV-2 of Moscow residents during the COVID-19 epidemic period. Infectious diseases. 2020; 18(4): 8-16. (in Russian)]. https://dx.doi.org/10.20953/1729-9225-2020-4-8-16.
- Временные методические рекомендации. Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19). Версия 14. 27.12.2021. Доступно по: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/059/041/original/ВМР_COVID-19_V14_27-12-2021.pdf Режим доступа 30.01.2022 [Temporary methodological guidelines. Prevention, diagnosis and treatment of new coronavirus infection (COVID-19). Version 14 (12/27/2021). Available at: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/059/041/original/ВМР_COVID-19_V14_27-12-2021.pdf (in Russian)].
- https:// coronavirus-monitor.info/ Режим доступа 05.02.2022.
- https://covid19.who.int Дата доступа 05.02.2022.
- Fontanet A., Autran B., Lina B., Kieny M.P., Abdool Karim S.S., Sridhar D. SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021; 397(10278): 952-4. https://dx.doi.org/10.1016/S0140-6736(21)00370-6.: 952-4.
- Abdool Karim S.S., Abdool Karim Q. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021; 398(10317): 2126-8. https://dx.doi.org/10.1016/S0140-6736(21)02758-6.
- https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W. et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395(10226): 809-15. https://dx.doi.org/10.1016/S0140-6736(20)30360-3.
- Министерство здравоохранения Российской Федерации. Временные методические рекомендации. Организация оказания медицинской помощи беременным, роженицам, родильницам и новорожденным при новой коронавирусной инфекции COVID-19. Версия 5. 28.12.2021. 135 c. Доступно по: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/059/052/original/BMP_preg_5.pdf Ссылка активна на: 07.01.2022. [Ministry of Health of the Russian Federation. Organization of medical care for pregnant women, women in labor, women in labor and newborns with a new coronavirus infection COVID-19. Methodological guidelines. Version 5. 28.12.2022. 135 р. Available at: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/059/052/original/BMP_preg_5.pdf (in Russian)].
- Белокриницкая Т.Е., Шаповалов К.Г. Грипп и беременность. М.: ГЭОТАР-Медиа; 2015. 144 c. [Belokrinitskaya T.E., Shapovalov K.G. Influenza and Pregnancy. M.: GEOTAR-Media; 2015. 144 p. (in Russian)].
- Schwartz D.A., Graham A.L. Potential maternal and infant outcomes from (Wuhan) Coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020; 12(2): 194. https://dx.doi.org/10.3390/v12020194.
- Белокриницкая Т.Е., Артымук Н.В., Филиппов О.С., Шифман Е.М. Динамика эпидемического процесса и течение новой коронавирусной инфекции COVID-19 у беременных Дальневосточного и Сибирского федеральных округов. Гинекология. 2020; 22(5): 6-11. [Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Shifman E.M. Dynamics of the epidemic process and the course of the COVID-19 in pregnant women of the Far Eastern and Siberian federal districts. Ginekologiya/ Gynecology. 2020; 22(5): 6-11. (in Russian)].
- Белокриницкая Т.Е., Артымук Н.В., Филиппов О.С., Фролова Н.И. Клиническое течение, материнские и перинатальные исходы новой коронавирусной инфекции COVID-19 у беременных Сибири и Дальнего Востока. Акушерство и гинекология. 2021; 2: 48-54. [Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I. Clinical course, maternal and perinatal outcomes of 2019 novel coronavirus infectious disease (COVID-19) in pregnant women in Siberia and Far East. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 2: 48-54. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.2.48-54.
- Zambrano L.D., Ellington S., Strid P., Galang R.R., Oduyebo T., Tong V.T. et al.; CDC COVID-19 Response Pregnancy and Infant Linked Outcomes Team. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status – United States, January 22-October 3, 2020. MMWR Morb. Mortal. Wkly Rep. 2020; 69(44): 1641-7. https://dx.doi.org/10.15585/mmwr.mm6944e3.
- Allotey J., Stallings E., Bonet M., Yap M., Chatterjee S., Kew T. et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis BMJ. 2020; 370: m3320. https:/dx.doi.org/10.1136/bmj.m3320.
- Figueiro-Filho E.A., Yudin M., Farine D. COVID-19 during pregnancy: an overview of maternal characteristics, clinical symptoms, maternal and neonatal outcomes of 10,996 cases described in 15 countries. J. Perinat. Med. 2020; 48(9): 900-11. https:/dx.doi.org/10.1515/jpm-2020-0364.
- Bellos I., Pandita A., Panza R. Maternal and perinatal outcomes in pregnant women infected by SARS-CoV-2: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021; 256: 194-204. https:/dx.doi.org/10.1016/j.ejogrb.2020.11.038.
- Jafari M., Pormohammad A., Neshin S.A.S., Ghorbani S., Bose D., Alimohammadi S. et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2021; 31(5): 1-16. https:/dx.doi.org/10.1002/rmv.2208.
- Vergara‐Merino L., Meza N., Couve‐Pérez C., Carrasco C., Ortiz‐Muñoz L., Madrid E. et al. Maternal and perinatal outcomes related to COVID‐19 and pregnancy: overview of systematic reviews. Acta Obstet. Gynecol. Scand. 2021; 100(7):1200-18. https:/dx./doi.org/10.1111/aogs.14118.
- Papapanou M., Papaioannou M., Petta A., Routsi E., Farmaki M., Vlahos N., Siristatidis Ch. Maternal and neonatal characteristics and outcomes of COVID-19 in pregnancy: An overview of systematic reviews. Int. J. Environ. Res. Public Health. 2021; 18(2): 596. https:/dx.doi.org/10.3390/ijerph18020596.
- Gonçalves B.M.M., Franco R.P.V., Rodrigues A.S. Maternal mortality associated with COVID-19 in Brazil in 2020 and 2021: Comparison with non-pregnant women and men. PLoS One. 2021; 16(12): e0261492. https:/dx.doi.org/10.1371/journal.pone.0261492.
- Metz T.D., Clifton R.G., Hughes B.L., Sandoval G., Saade G.R., Grobman W.A. et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network. Disease severity and perinatal outcomes of pregnant patients with coronavirus disease 2019 (COVID-19). Obstet. Gynecol. 2021; 137(4): 571-80. https:/dx.doi.org/10.1097/AOG.0000000000004339.
- La Verde M., Riemma G., Torella M., Cianci S., Savoia F., Licciardi F. et al. Maternal death related to COVID-19: A systematic review and meta-analysis focused on maternal co-morbidities and clinical characteristics. Int. J. Gynaecol. Obstet. 2021; 154(2): 212-9. https:/dx.doi.org/ 10.1002/ijgo.13726.
- Piekos S.N., Roper R.T., Hwang Y.M., Sorensen T., Price N.D., Hood L., Hadlock J.J. The effect of maternal SARS-CoV-2 infection timing on birth outcomes: a retrospective multicentre cohort study Lancet Digit. Health. 2022; 4(2): e95-e104. https:/dx.doi.org/10.1016/S2589-7500(21)00250-8.
- Yang J., D'Souza R., Kharrat A., Fell D.B., Snelgrove J.W., Shah P.S. COVID-19 pandemic and population-level pregnancy and neonatal outcomes in general population: A living systematic review and meta-analysis (Update#2: November 20, 2021). Acta Obstet. Gynecol. Scand. 2022; 101(3): 273-92.
- https:/dx.doi.org/10.1111/aogs.14318.
- Филиппов О.С., Гусева Е.В. Основные показатели деятельности акушерско-гинекологической службы В Российской Федерации в 2019 году. М.; 2020. 30 с. [Filippov O.S., Guseva E.V. Key performance indicators of the obstetric and gynecological service in the Russian Federation in 2019. Moscow; 2020. 30 p. (in Russian)].
- Vale A.J.M., Fernandes A.C.L., Guzen F.P., Pinheiro F.I., de Azevedo E.P., Cobucci R.N. Susceptibility to COVID-19 in pregnancy, labor, and postpartum period: immune system, vertical transmission, and breastfeeding. Front. Glob. Womens Health. 2021; 2: 602572. https:/dx.doi.org/10.3389/fgwh.2021.602572.
- Wei S.Q., Bilodeau-Bertrand M., Liu S., Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021; 193(16): E540-8. https:/dx.doi.org/10.1503/cmaj.202604.
- Chmielewska B., Barratt I., Townsend R., Kalafat E., van der Meulen J., Gurol-Urganci I. et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob. Health. 2021; 9(6): e759-72. https:/dx.doi.org/10.1016/S2214-109X(21)00079-6.
- Litman E.A., Yin Y., Nelson S.J., Capbarat E., Kerchner D., Ahmadzia H.K. Adverse perinatal outcomes in a large US birth cohort during the COVID-19 pandemic: adverse perinatal outcomes during COVID-19. Am. J. Obstet. Gynecol. MFM. 2022; 4(3): 100577. https:/dx.doi.org/10.1016/j.ajogmf.2022.100577.
Received 07.02.2022
Accepted 04.03.2022
About the Authors
Tatiana E. Belokrinitskaya, MD, PhD, Professor, Head of the Obstetrics and Gynecology Department of the Pediatric Faculty and Faculty of Professional Retraining,Chita State Medical Academy, Ministry of Health of Russia, +7(3022)32-30-58, tanbell24@mail.ru, https://orcid.org/0000-0002-5447-4223, 39a Gorky str., Chita,
672000, Russian Federation.
Natalya V. Artymuk, MD, PhD, Professor, Head of the G.A. Ushakova Department of Obstetrics and Gynecology, Kemerovo State Medical University, Ministry of Health
of Russia, +7(3842)73-48-56, artymuk@gmail.com, https://orcid.org/0000-0001-7014-6492, 22a Voroshilova str., Kemerovo, 650056, Russian Federation.
Oleg S. Filippov, MD, PhD, Professor, Professor of the Department of Obstetrics and Gynecology, A.I. Yevdokimov Moscow State Medical and Dental University,
Ministry of Health of Russia, Deputy Director, Federal Research and Clinical Center for Children and Adolescents of FMBA of Russia, +7(499)324-43-00,
filippovolsem@yandex.ru, https://orcid.org/0000-0003-2654-1334, 20 Mockvorechye str., Moscow, 115409, Russian Federation.
Nataly I. Frolova, MD, PhD, Associate Professor of the Department of Obstetrics and Gynecology of the Pediatric Faculty and Faculty of Professional Retraining,
Chita State Medical Academy, Ministry of Health of Russia, taasyaa@mail.ru, https://orcid.org/0000-0002-7433-6012, 39a Gorky str., Chita, 672000, Russian Federation.
Corresponding author: Tatiana E. Belokrinitskaya, tanbell24@mail.ru
Authors’ contributions: Artymuk N.V., Belokrinitskaya T.E. – design and concept of the study, collection and processing of the material; Frolova N.I. – statistical data processing; Belokrinitskaya T.E., Artymuk N.V. – writing the text; Filippov O.S. – editing.
Conflicts of interest: The authors declare that they have no competing interests.
Funding: The study was performed without external funding.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I.
COVID-19 in pregnant women of Siberia and the Russian Far East: 2-year results of the pandemic.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 4: 47-54 (in Russian)
https://dx.doi.org/10.18565/aig.2022.4.47-54