Analysis of the structure of gynecological diseases and extent of surgery in patients of different age groups supervised in the cervical and endometrial pathology office
Rosyuk E.A., Oboskalova T.A., Verba T.E., Salimova I.V., Tureeva A.V.
Objective: This study aimed to analyze the structure of gynecological diseases and the extent of surgery in patients of different age groups supervised in the cervical and endometrial pathology office.
Materials and methods: A total of 369 patients from different age groups were included in this study. Group 1 (n=290) consisted of women aged 18–44 years who received medical care in the cervical and endometrial pathology office. Group 2 (n=44) consisted of women aged 45–59 years old. Group 3 (n=30) included women aged 60–74 years old. The study analyzed the structure of gynecological pathology in these groups.
Results: The study found that CIN I was more frequently detected in women in group 2, while CIN II was most frequently detected in women in group 3. The rate of CIN III was similar in all three groups, with percentages of 14.1, 15.9, and 13.3%, respectively. In terms of surgical procedures, cervical excision (LLETZ) was performed less frequently in all age groups (group 1, 8.62%; group 2, 4.55%; and group 3, 10%) than cervical electroconization (group 1, 27.93%; group 2, 45.45%; group 3, 36.67%).
Conclusion: The findings of this study indicate that in the cervical and endometrial pathology office, the majority of patients (78.59%) were women aged 18–44 years. In 93.3–100% of cases, patients undergo tissue treatment with a solution cavitated by low-frequency ultrasound before surgical treatment. Electroconization is most commonly performed in women aged 45–59 years (45.45%) for the treatment of precancerous diseases of the cervix. Ablative treatments are predominantly used for hemostasis, and less commonly for the treatment of CIN I.
Authors' contributions: Rosyuk E.A., Oboskalova T.A., Verba T.E., Salimova I.V., Tureeva A.V. – conception and design of the study; Verba T.E., Salimova I.V. – material collection and processing; Rosyuk E.A. – statistical analysis, drafting of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Ural State Medical University.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Rosyuk E.A., Oboskalova T.A., Verba T.E., Salimova I.V., Tureeva A.V. Analysis of the
structure of gynecological diseases and extent of surgery in patients of different age groups
supervised in the cervical and endometrial pathology office.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (5): 92-98 (in Russian)
https://dx.doi.org/10.18565/aig.2024.6
Keywords
The most effective methods for preventing cervical cancer are vaccination and the treatment of cervical precancerous diseases once detected [1]. Prompt and effective treatment of cervical intraepithelial neoplasia (CIN) can result in complete cure and prevent progression to malignancy [2].
Although cervical cancer is more common in older women, there has been an increase in cases of diagnosing early forms of reproductive system cancer in young women [3, 4]. Therefore, it is important to determine the incidence of cervical precancerous disease in women based on age. By analyzing these data, we can identify a specific age group of women who require closer screening for cervical cancer and justify the need for appropriate medical management [5].
Currently, there is a rising trend in the incidence of endometrial cancer among younger women. Researchers have emphasized the importance of preventive therapy, including the morphological control of the endometrium [6]. It is promising to gather high-risk patients for endometrial cancer in one institution to facilitate diagnosis, surgical treatment if necessary, and effective treatment prescriptions. The authors also highlight that after surgical treatment for abnormal uterine bleeding, hormone therapy is often prescribed for a short period or not at all, which is insufficient for preventing endometrial cancer in the future [7].
This study aimed to analyze the prevalence of gynecological diseases and the extent of surgeries performed in patients of different age groups under the supervision of cervical and endometrial pathology offices.
Materials and methods
This epidemiological descriptive study of the incidence and prevalence of gynecological diseases in patients at the cervical pathology office was conducted at the Yekaterinburg Clinical Perinatal Center (YCPC) between 2022 and 2023. The study analyzed the indicators of the adult female population.
In the cervical and endometrial pathology office of the YCPC, various manipulations were performed in 412 patients. For this study, the authors selected a group of women who had undergone a full range of diagnostic tests, including general clinical investigations, colposcopy in patients with cervical pathology, cervical cytology, and morphological examination of cervical, vaginal, endometrial, or vulvar tissues. A total of 369 patients were included in this study (n=369).
Patients aged 18–20 years represented 7/369 (1.9%) of the cohort, those aged 21–30 years 73/369 (19.7%), and those aged 31–40 years 168/369 (45.5%). The 41-50 age group comprised 64/369 (17.3%) of the cohort, while the 51-60 age group comprised 22/369 (5.96%). The 61–70 age group comprised 23/369 (6.2%) of the cohort, and individuals 71 years of age or older comprised 12/369 (3.3%).
To make a comparative analysis of the structure of cervical and endometrial diseases, we divided the patients into three groups according to their age (based on the WHO classification):
Group 1 included women who received medical care in the cervical and endometrial pathology office, aged 18–44 years (young age according to the WHO), n=290.
Group 2 included women who received medical care in the cervical and endometrial pathology office, aged 45–59 years (WHO average age), n=44.
Group 3 included women who received medical care in the cervical and endometrial pathology office, aged 60–74 years (old age according to WHO), n=30.
All women who took part in the study were referred by doctors from antenatal clinics in the city of Yekaterinburg in accordance with order 521-p dated March 16, 2022 “On the organization of medical care for patients with pathology of the cervix and endometrium in the city of Yekaterinburg”. Medical care was provided in accordance with the order of the Ministry of Health of Russia dated October 20, 2020, N 1130n “On approval of the procedure for providing medical care in the field of obstetrics and gynecology”, as well as clinical recommendations.
All manipulations of the cervix, vagina, and vulva were carried out under the control of the MK-200 “Scanner” video colposcope with the ability to use the visual VIA method, archiving images on paper in color. Treatment with low-frequency ultrasound solutions was performed using an ultrasonic surgical device AUZH-100 “Fotek” (for carrying out cavity and extra-cavitary cavitation). Tissue biopsy, cervical excision (LLETZ), cervical electroconization, argon plasma coagulation of the cervix was performed on a high-frequency electrosurgical device with argon-enhanced coagulation EHVCha-140 “Fotek.” Smoke evacuation during manipulation was carried out using an ASD smoke aspiration device “Fotek.” Laser vaporization of tissues was performed using a laser surgical device with photodynamic and hyperthermic exposure modes (Lakhta-Milon). Office hysteroscopy was performed using the SOPRO-181 endoscopic video camera, which allows the procedure to be performed on an outpatient basis without instrumental dilation of the cervical canal or anesthesia. The authors analyzed the structure of gynecological diseases in patients of different age groups and the list of medical procedures in each group.
Statistical analysis
Statistical analysis was performed using descriptive statistics in an Excel spreadsheet. The arithmetic mean (M) and standard deviation (SD), presented as M (SD), were used to describe quantitative data with normal distribution.
Results
The mean age of the patients in group 1 was 33.76 (6.07) years. After carrying out a full diagnostic investigation, including histological examination of the tissue of the cervix, vagina, or vulva, we obtained the following data on the structure of the disease. The incidence of CIN I was 69/290 (23.79%), whereas CIN II occurred in 139/290 (47.93%) patients. CIN III was found in of 41/290 (14.13%) patients. Benign conditions and normal cervical tissue (leukoplakia, true erosion, and normal cervical epithelium) were observed in 58/290 (20%) patients. Hyperplastic endometrial disease was found in 17/290 cases (5.86%). Cervical cancer was detected in 5/290 patients (1.72%), while vulvar intraepithelial neoplasia (VIN) was not detected.
The mean age of patients in group 2 was 50.89 (4.09) years. The structure of diseases of the cervix, vagina, vulva, and endometrium is presented as follows: incidence of CIN I, 13/44 (29.55%); CIN II, 18/44 (40.91%); CIN III, 7/44 (15. 91%), benign diseases of the cervix – 11/44 (25%), cervical cancer – 1/44 (2.27%), endometrial hyperplastic processes – 2/44 (4.55%), VIN – 1/44 (2.27 %).
The mean age of the patients in group 3 was 67.13 (3.86) years. The structure of diseases of the cervix, vagina, vulva, and endometrium is presented as follows: incidence of CIN I, 5/30 (16.67%); CIN II, 18/30 (60%); CIN III, 4/30 (13.33%); benign diseases of the cervix, 6/30 (20%); cervical cancer, 0; endometrial hyperplastic process, 0; VIN, 3/30 (10%).
Comparative analysis of the structure of cervical, vulvar, and endometrial diseases in women of different age groups revealed the following characteristics (Table 1): CIN I was more frequent in women in group 2, but CIN II was more frequent in women in group 3. CIN III occurred with almost the same incidence in all three groups (14.13, 15.91 %, and 13.33 %, respectively). The incidence of benign diseases, cervical cancer, and endometrial hyperplastic processes does not depend on patient age. VIN was not registered in group 1, but in group 3, it occurred at a frequency of 2.27% (Table 1).
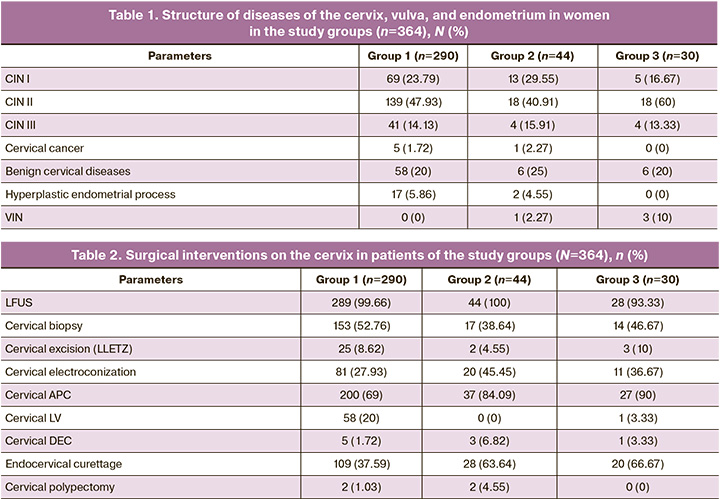
A comparative analysis of the extent of surgical interventions in the cervical and endometrial pathology office revealed the following features (Table 2). In group 1, the genital tract was treated with low-frequency ultrasound (LFUS) cavitated solutions in 289/290 (99.66%) cases. The following procedures were performed on the cervix for therapeutic and diagnostic purposes: 153/290 (52.76%) underwent point/multifocal biopsy, and 25/290 (8.62%) patients received LLETZ treatment. Additionally, 81 patients (27.93%) underwent cervical electroconization, while 200 patients (69%) were treated with argon plasma coagulation (APC). Laser vaporization (LV) was performed in 58 patients (20%), and 5/290 (1,72%) patients underwent diathermoelectrocoagulation (DEC). Three patients (1.03%) underwent cervical polypectomy and 109 patients (37.59%) underwent endocervical curettage. Operations on the body of the uterus included aspiration from the uterine cavity (pipelle biopsy) in 27/290 (9.31%), office hysteroscopy in 19/290 (6.55%), and insertion and removal of an intrauterine device (IUD) in 0. Patients in group 1 did not undergo a single biopsy of the vaginal vault.
In 44/44 (100%) cases in group 2, the genital tract was treated with solutions cavitated using LFUS. Therapeutic and diagnostic procedures of the cervix: point/multifocal biopsy was performed in 17/44 (38.64%), LLETZ in 2/44 (4.55%), cervical electroconization in 20/44 (45.45%), APC of the cervix in 37/44 (84.09%), LV of the cervix in 0, DEC of the cervix in 3/44 (6.82%), polypectomy of the cervix in 2/44 (4.55%), and endocervical curettage in 28/44 (63.64%) patients. Surgeries on the body of the uterus included aspirate from the uterine cavity (pipelle biopsy) in 3/44 (6.82%), office hysteroscopy (0), insertion and removal of the IUD (0. In group 2, vaginal vault biopsy was performed in 2/44 (4.55%) cases.
In group 3, in 28/30 (93.33%) patients, the genital tract was treated with solutions cavitated using LFUS. Therapeutic and diagnostic procedures of the cervix: point/multifocal biopsy in 14/30 (46.67%), LLETZ – in 3/30 (10%), cervical electroconization in 11/30 (36.67%), APC of the cervix in 27/30 (90%), cervical LV in 1/30 (3.33%), cervical DEC in 1/30 (3.33%), cervical polypectomy in 0, and endocervical curettage in 20/30 (66.67%). Operations on the body of the uterus included aspiration from the uterine cavity (pipelle biopsy) in 11/30 (36.67%) patients; office hysteroscopy, 0; insertion and removal of the IUD, 0. In group 3, vaginal vault biopsy was performed in 1/30 (3.33%) patients.
Discussion
The use of LFUS-generated solutions was lowest in group 3, i.e., in 28/30 (93.3%) patients, compared to patients in groups 1 and 2 (Table 2). Several studies have described a therapeutic approach to gynecological diseases using LFUS, which is widely used in Russia and other countries with impressive results [8–13]. In the cervical pathology office, this technique is often used before surgery to prevent postoperative infection and inflammation, especially in women with a history of cervicitis and vaginitis. These findings suggest that inflammatory diseases of the female reproductive system are more prevalent in women of reproductive age, making the use of LFUS particularly beneficial in this patient population. In older women, the use of local estrogens in addition to LFUS may be necessary to accelerate tissue repair [13]. We did not find significant differences in the frequency of cervical biopsy (spot or multifocal), cervical electroconization, and therapeutic and diagnostic endocervical curettage, as well as in the incidence of manipulations such as pipelle biopsy (aspiration from the uterine cavity), insertion and removal of the IUD, and biopsy of the vaginal vault. This indicates a high frequency of diagnostic procedures (e.g., cervical biopsy) to confirm the diagnosis and determine the extent of surgical treatment in patients of different age groups. It should also be noted that a high percentage of cervical curettages were performed immediately after electroconization or LLETZ, as described in the 2020 clinical guidelines, regardless of patient age [14]. LLETZ was performed much less frequently (group 1, 8.62%; group 2, 4.55%; and group 3, 10%) than cervical electroconization (group 1, 27.93%; group 2, 45.45%; group 3, 36.67%) in all age groups. This trend is determined only by the choice of surgeon performing the operation, taking into account the diagnosis, additional examination data, and patient age. The literature data indicate comparable effectiveness for both procedures [15].
Cervical electroconization was performed least frequently in women in group 1, in favor of LLETZ. This may be due to the desire of physitioans to perform manipulations in the operating room to preserve the length of cervical canal for the subsequent implementation of reproductive function, prevention of isthmic cervical insufficiency, and pretrm birth [16].
Cervical APC was most often performed in women group 3 – 90% compared to group 1 – 69%. It should be noted that, basically, the use of this type of energy was required for hemostasis, and taking into account the fact that patients in group 3 more often underwent operations with the removal of a large volume of tissue, these figures are logical and understandable. Another reason for the low percentage of cervical APC use in group 1 was the choice in favor of cervical LV (in group 1 – 20%; group 3 – 3.33%). According to the literature, laser vaporization of the cervix is increasingly common in young patients [17].
In group 2, hemostasis was most often performed using cervical DEC (6.82%) compared to group 1 (1.72%) and group 3 (3.33%). In the case of capillary bleeding, hemostasis can be performed with an argon plasma torch, penetrating 3 mm into the tissue depth; argon effectively stops bleeding and does not cause additional damage to the underlying stroma and surrounding tissues. Jet bleeding should be stopped using a ball electrode in the appropriate mode (DEC) because in this case, an impact to a depth of more than 3 mm is required [18]. It can be assumed that patients in group 1 developed capillary bleeding more often after manipulation than those in group 2 (jet). In general, the authors demonstrated the active use of a variety of diagnostic and treatment methods in patients at the cervical and endometrial pathology office. Patients with cervical pathology are treated more often than those with endometrial pathology, which is explained by the growth of CIN I in the Ural region [19] and the good work of the administrative resources of the metropolis in routing patients with precancerous cervical pathology.
According to the results of pipelle biopsy, uterine pathology (mainly endometrial hyperplasia) was found only in 17/290 (5.86%) women in the first group, in 2/44 (4.55%) women in the second group, and in none of the women in the third group.
This indicates that patients with endometrial pathology are most often referred to the hospital for hysteroscopy not only for diagnosis but also for therapeutic purposes. Due to the frequent detection of occlusion of the cervical canal in postmenopausal women over 60 years of age, they do not undergo a pipelle biopsy.
Polypectomy in outpatient settings was performed significantly more often in group 2 (4.55%) than in groups 1 (1.1%) and 3 (0%). We can conclude that a polyp in the lower third of the cervical canal (a polyp of the upper 2/3 of the cervical canal is removed during hysteroscopy) is more often found in women aged 45–59 years than in younger people (up to 44 years) or women over 60 years of age [18].
Conclusion
In the cervical and endometrial pathology office, 78.6% of the patients were young women aged 18–44 years, mainly with cervical diseases. The standard of diagnosis of cervical pathology is observed regardless of age: first biopsy, then excision, or cervical electroconization. In the cervical pathology office, in 93.3–100% of cases, in patients of all ages, prior to surgical treatment, the tissue was treated with a solution cavitated by LFUS. Cervical electroconization was most commonly used (45.5%) to treat precancerous cervical conditions in women aged 45–59 years. Ablative procedures (cervical APC and LV) are most frequently used for hemostasis and less commonly for treating CIN I.
References
- Доброхотова Ю.Э., Боровкова Е.И. Вакцинация от вируса папилломы человека: доказательная база эффективности и безопасности. Гинекология. 2021; 23(2):125-30. [Dobrokhotova Yu.E., Borovkova E.I. Human papillomavirus vaccination: Evidence base for efficacy and safety. Gynecology. 2021; 23(2): 125-30. (in Russian)]. https://dx.doi.org/10.26442/20795696.2021.2.200742.
- Роговская С.И., Шабалова И.П., Улумбекова Г.Э., Короленкова Л.И., Бебнева Т.Н., Гущин А.Е., Кира Е.Ф., Кондриков Н.И., Кононова И.Н., Ледина А.В., Лешкина Г.В., Мингалева Н.В., Могиревская О.А., Подзолкова Н.М., Полонская Н.Ю., Смирнов В.В., Фириченко С.В., Шипулина О.Ю. Организационные вопросы профилактики рака шейки матки в России. ОРГЗДРАВ: новости, мнения, обучение. Вестник ВШОУЗ. 2021; 7(4): 16-31. [Rogovskaya S.I., Shabalova I.P., Ulumbekova G.E., Korolenkova L.I., Bebneva T.N., Gushchin A.E., Kira E.F., Kondrikov N.I., Kononova I.N., Ledina A.V., Leshkina G.V., Mingaleva N.V., Mogirevsklaya O.A., Podzolkova N.M., Polonskaya N.Yu., Smirnov V.V., Firichenko S.V., Shipulina O.Yu. The cervical cancer prevention in Russia. HEALTHCARE MANAGEMENT: News, Views, Education. Bulletin of VSHOUZ. 2021; 7(4): 16-31. (in Russian)]. https://dx.doi.org/10.33029/2411-8621-2021-7-4-16-31.
- Короленкова Л.И. Влияние морфологических особенностей цервикального канцерогенеза на эффективность диагностики и лечения CIN III и микроинвазивного рака шейки матки. Opinion Leader. 2018: S1: 80-5. [Korolenkova L.I. Influence of morphological features of cervical carcinogenesis on the efficiency of diagnosis and treatment of CIN III and microinvasive cervical cancer. Opinion Leader. 2018: S1: 80-5. (in Russian)].
- Mayadev J.S., Ke G., Mahantshetty U., Pereira M.D., Tarnawski R., Toita T. Global challenges of radiotherapy for the treatment of locally advanced cervical cancer. Int. J. Gynecol. Cancer. 2022; 32(3): 436-45. https://dx.doi.org/10.1136/ijgc-2021-003001.
- Селякова М.С., Агеева Т.А., Савченко С.В., Якимова А.В. Особенности иммуногистохимических характеристик диспластического многослойного плоского эпителия шейки матки у женщин разных возрастных групп. Уральский медицинский журнал. 2018; (2): 43-7. [Seliakova M.S., Ageeva T.A., Savchenko S.V., Yakimova A.V. Features and immunohistochemical characteristics displastic squamous epithelium of the cervix in women of different age groups. Ural Medical Journal. 2018; (2): 43-7. (in Russian)].
- Клинышкова Т.В., Турчанинов Д.В., Фролова Н.Б. Клинико-эпидемиологические аспекты рака тела матки с позиции профилактики рецидивирования гиперплазии эндометрия. Акушерство и гинекология. 2020; 1: 135-40. [Klinyshkova T.V., Turchaninov D.V., Frolova N.B. Clinical and epidemiological aspects of corpus uteri cancer in the context of prevention of recurrent endometrial hyperplasia. Obstetrics and Gynecology. 2020; (1): 135-40. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.1.135-140.
- Тен А.Р., Обоскалова Т.А., Воронцова А.В. Рецепция эндометрия на фоне гормональной терапии у женщин репродуктивного возраста, перенесших аномальное маточное кровотечение, обусловленное овуляторными нарушениями. Гинекология. 2022; 24(4): 283-8. [Ten A.R., Oboskalova T.A., Vorontsova A.V. Endometrial receptivity during hormonal therapy in women of reproductive age with abnormal uterine bleeding due to ovulatory disorders. Gynecology. 2022; 24(4): 283-8. (in Russian)]. https://dx.doi.org/10.26442/20795696.2022.4.201746.
- Фириченко С.В., Попова Е.О., Смирнова С.О. Хронический неспецифический цервицит. Акушерство и гинекология. 2023; 7: 135-46. [Firichenko S.V., Popova E.O., Smirnova S.O. Chronic nonspecific cervicitis. Obstetrics and Gynecology. 2023; (7): 135-46 (in Russian)]. https://dx.doi.org/10.18565/aig.2022.233.
- Маковская Д.С., Аполихина И.А., Горбунова Е.А., Саидова А.С., Тетерина Т.А., Бычкова А.Е. Консервативные методы лечения декубитальных язв у женщин с пролапсом тазовых органов. Медицинский оппонент. 2023; 2(22): 67-74. [Makovskaya D.S., Apolikhina I.A., Gorbunova E.A., Saidova A.S., Teterina T.A., Bychkova A.E. Conservative treatments of decubitus ulcers in women with pelvic organ prolapse. Medical Opponent. 2023; 2(22): 67-74. (in Russian)].
- Добренькая Г.С., Скобцов А.В., Бахина Н.В. Ультразвуковой контроль лечения хронического эндометрита УЗ-кавитацией полости матки. Universum: медицина и фармакология. 2022; 12(94): 4-6. [Dobrenkaya G.S., Skobtsov A.V., Bakhina N.V. Ultrasonic control of the treatment of chronic endometritis by US cavitation of the uterine cavity. Universum: Medicine & pharmacology. 2022; 12(94): 4-6. (in Russian)]. https://dx.doi.org/10.32743/UniMed.2022.94.12.14702.
- Каттаходжаева М.Х., Кудратова Д.Ш., Кодырова З.Н. Влияние ультразвуковой кавитации на микробиоценоз влагалища женщин, страдающих рецидивирующим кольпитом. Central Asian Journal of Medical and Natural Science. 2023; 4(3): 191-7. [Kattakhodzhaeva M.Kh., Kudratova D.Sh., Kodyrova Z.N. Influence of ultrasonic cavitation on vaginal microbiocenosis of women suffering from recurrent colpitis. Central Asian Journal of Medical and Natural Science. 2023; 4(3): 191-7. (in Russian)].
- Сорокин Ю.А., Гизингер О.А., Радзинский В.Е. Клинико-иммунологическое обоснование ультразвуковой кавитации в комплексном лечении бесплодия при хроническом эндометрите. Гинекология. 2022; 24(5): 355-61. [Sorokin Yu.A., Gizinger O.A., Radzinsky V.E. A clinical and immunological rationale for ultrasonic cavitation use in the complex treatment of infertility in chronic endometritis. Gynecology. 2022; 24(5): 355-61. (in Russian)]. https://dx.doi.org/10.26442/20795696.2022.5.201866.
- Буянова С.Н., Щукина Н.А., Петросян Е.И., Дуб Н.В. Ультразвуковая кавитация как этап предоперационной подготовки у пациенток с рубцовой деформацией шейки матки. Акушерство и гинекология. 2020; 4 (Приложение): 36-7. [Buyanova S.N., Shchukina N.A., Petrosyan E.I., Dub N.V. Ultrasound cavitation as a stage of preoperative preparation in patients with scar deformation of the cervix. Obstetrics and gynecology. 2020; 4 (Suppl): 36-7. (in Russian)].
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Цервикальная интраэпителиальная неоплазия, эрозия и эктропион шейки матки. 2020. [Ministry of Health of the Russian Federation. Clinical guidelines. Cervical intraepithelial neoplasia, erosion and cervical ectropion. 2020. (in Russian)].
- Basu P., Taghavi K., Hu S.Y., Mogri S., Joshi S. Management of cervical premalignant lesions. Curr. Probl. Cancer. 2018; 42(2): 129-36. https://dx.doi.org/10.1016/j.currproblcancer.2018.01.010.
- Santesso N., Mustafa R.A., Wiercioch W., Kehar R., Gandhi S., Chen Y. et al. Systematic reviews and meta-analyses of benefits and harms of cryotherapy, LEEP, and cold knife conization to treat cervical intraepithelial neoplasia. Int. J. Gynaecol. Obstet. 2016; 132(3): 266-71. https://dx.doi.org/10.1016/j.ijgo.2015.07.026.
- Юминова А.В., Тен А.Р. Исходы лазерной вапоризации и фотодинамической терапии при заболеваниях шейки матки. Colloquium-Journal. 2018; 13-2(24): 40-3. [Yuminova A.V., Ten A.R. Results of laser vaporization and photodynamic therapy for cervical diseases. Colloquium-Journal. 2018; 13-2(24): 40-3. (in Russian)].
- Роговская С.И., Подзолкова В.Н., Куликов А.Г., Бебнева Т.Н. и др. Физические методы лечения в амбулаторной практике акушера-гинеколога. Кавитированные растворы. Радиоволна. Аргоновая плазма. Руководство для врачей. М.; 2020. 100с. [Rogovskaya S.I., Podzolkova V.N., Kulikov A.G., Bebneva T.N. et al. Physical treatments in the outpatient practice of an obstetrician-gynecologist. Cavitated solutions. Radio wave. Argon plasma. A guide for doctors. Moscow; 2020. 100p. (in Russian)].
- Севостьянова О.Ю., Обоскалова Т.А., Чумарная Т.В., Росюк Е.А., Беломестнов С.Р., Севостьянова Н.Е. Эпидемиологические особенности заболеваемости цервикальной интраэпителиальной неоплазией в современном мегаполисе. Опухоли женской репродуктивной системы. 2023; 19(1): 112-9. [Sevostyanova O.Yu., Oboskalova T.A., Chumarnaya T.V., Rosyuk E.A., Belomestnov S.R., Sevostyanova N.E. Epidemiological features of the incidence of cervical intraepithelial neoplasia in the modern megapolis. Tumors of female reproductive system. 2023; 19(1): 112-9. (in Russian)]. https://dx.doi.org/10.17650/1994-4098-2023-19-1-112-119.
Received 14.01.2024
Accepted 27.04.2024
About the Authors
Elena A. Rosyuk, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repina str., 3, +7(902)26-56-385, elenakdc@yandex.ru, https://orcid.org/0000-0003-1303-3955Tatyana A. Oboskalova, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia,
620028, Russia, Yekaterinburg, Repina str., 3, +7(912)28-37-631, oboskalova.tat@yandex.ru, https://orcid.org/ 0000-0003-0711-7896
Tatyana E. Verba, Obstetrician-Gynecologist at the Gynecological Department, Yekaterinburg Clinical Perinatal Center,
620137, Russia, Yekaterinburg, Komvuzovskaya str., 3, +7(904)38-11-130.
Irina V. Salimova, Head of the Polyclinic, Yekaterinburg Clinical Perinatal Center, 620137, Russia, Yekaterinburg, Komvuzovskaya str., 3, +7(902)26-23-508.
Alena V. Tureeva, Head of the Gynecological Department, Yekaterinburg Clinical Perinatal Center, 620137, Russia, Yekaterinburg, Komvuzovskaya str., 3, +7(912)67-86-000.