The role of combined oral contraceptives in cervical intraepithelial neoplasia occurrence associated with human papillomavirus infection
Aim: To study the incidence and course of cervical intraepithelial neoplasia (CIN) in women infected with highly oncogenic types of human papillomavirus (HPV) infection, who had indications for taking hormonal contraceptive pills in history.Klyukina L.A., Sosnova E.A., Ischenko A.A.
Materials and methods: The study included 163 women aged 19–45 years with high-risk HPV types (16, 18, 31, 33, 35, 51, 52, 56, 58). The physical status of HPV-16 was evaluated in 81 women with mono-infection. All women underwent examination in Treatment and Rehabilitation Center of the Ministry of Health of Russia in the period from 2020 to May, 2021.
Results: 84 (51.5%) HPV-positive women who had indications for taking hormonal contraceptive pills in history were included in the main group; 79 (48.5%) HPV-positive women who never took hormonal contraception pills were included in the comparison group. It was found that continuous intake of hormonal pills effects the severity of CIN; respectively, in women who took hormonal contraception pills, severe cervical dysplasia was found most often (Н=18.352, р=0.001). Based on the results of the study of three forms of human papillomavirus infection occurrence: episomal, mixed and integrated, it can be assumed that continuous intake of hormonal contraception pills among women with HPV-16 infection in the form of mono-infection, may have effect on the physical status of HPV and accelerate the progression of human papillomavirus infection to the integrated form (Uemp.=88.5, р=0.001).
Conclusion: Thus, it can be assumed that intake of oral hormonal contraceptives may have a negative effect on the course of papillomavirus infection and contribute to development and accelerated progression of CIN. Further studies on this issue will provide development of optimal management tactics for patients taking hormonal contraception pills with purpose of timely diagnosis and reduction of the risk of neoplastic progression and development of invasive forms of cervical cancer.
Keywords
Currently, cervical cancer (CC) incidence among women of reproductive age continues to grow steadily worldwide. According to the data of the world source GLOBOCAN of the International Agency for Research on Cancer (IARC), 604.127 new cases of CC were registered in the world in 2020. In Russia, cervical cancer incidence ranks second among women under the age of 45 years, and cancer mortality ranks first among women in this age group. [1].
Human papillomavirus (HPV) infection is considered to be a major factor of cervical cancerogenensis, and human papilloma virus can cause precancerous lesions and malignant transformation of exocervical (or ectocervical) cells. At the global level, according to the results of epidemiological studies, among 220 known HPV genotypes, 13 high-risk HPV genotypes were detected (4 species of α-genus human papillomaviruses (α-HPVs) 16, 31, 33, 35, 52 and 58, α7-HPVs 18, 39, 45 and 59, α5-HPV51 and α6-HPV56. Their integration into host chromosomes is considered to be a leading cause of carcinogenesis [2–4]. HPV type 16 has the highest cancirogenic potential and is detected in 60% of all cases of CC [2, 5]. HPV has a uniquely life cycle, in which “early” viral proteins (Е1, Е2, Е6, Е7) play a key role [6]. At initial viral penetration, the virus infects the cells of the basal layer of stratified squamous epithelium, but does not penetrate into the underlying layers. Viral genomes are maintained as episomes in the basal layer; at the same time, viral genes expression is tightly controlled as the infected cells migrate to the surface of the epithelial cells [7]. E2 proteins from high-risk HPV regulate replication of viral genome and viral oncogenes Е6 and Е7 transcription [8]. Integration of the virus into the cellular genome is accompanied by disruption of E2 open reading frame, loss of E2 activity, high expression of oncoproteins E6 and E7, and HPV infection progression [9]. Maintenance of the malignant phenotype, genome instability and transformation of primary human keratinocytes are mainly mediated by continuous expression of high risk HPV E6 and E7 proteins.
Thus, cervical infection with high-risk HPV types with subsequent viral integration into the host cell genome is morphologically expressed in the development of pre-invasive epithelial lesions – cervical intraepithelial neoplasia (CIN) or squamous intraepithelial lesions (SIL): low grade squamous intraepithelial lesions (LSIL) and high grade squamous intraepithelial lesion (HSIL) which may progress to invasive cervical cancer.
The period from primary infection to progression to severe grades of CIN takes about several months and may last for several years, and this proves the importance of timely and effective monitoring of women with human papillomavirus infection. However, it is common that the process of transformation into cervical cancer proceeds very rapidly and does not comply with a clear structure of the steps in the formation of carcinogenesis [9]. On the other hand, it is important to bear in mind that women at the age of 15–45 years are sexually active fertile women, and the issue of prevention of unplanned pregnancy is extremely important for them. Therefore, they need effective and safe methods of contraception. Currently, combined oral contraceptives (COCs) remain to be one of the most common prevention method for unplanned pregnancy. According to various estimates, more than 150 million women worldwide take hormonal contraceptive pills, and the percentage of them among women aged 15–49 years is approximately 13% [10]. The issue regarding oncological vigilance in prescribing contraceptives, determining drug exposure duration and dynamic surveillance of women taking oral hormonal contraceptives remains relevant.
The aim of this research was to study the incidence and severity of cervical intraepithelial neoplasia (CIN) in HPV-positive women of reproductive age, who took hormonal contraceptive pills.
Materials and methods
The study was carried out in Treatment and Rehabilitation Center of the Ministry of Health of Russia in the period from 2020 to May, 2021. The study included 163 women aged 19–45 years with HPV. HPV genotyping was performed and high-risk HPV types (16, 18, 31, 33, 35, 51, 52, 56, 58) were detected. The physical status of HPV-16 was evaluated in 81 women with mono infection. Given the fact the patients had indications for taking hormonal contraceptive pills in medical history, they were divided into 2 groups. The main group included 84 (51.5%) HPV-positive women with various duration of oral contraceptive pill use; and the comparison group included 79 (48.5%) HPV-positive women who never took oral hormonal contraceptives.
According to the anamnestic data on taking contraceptives in the main group, all women took combined low-dose monophasic oral contraceptives (30–35 μg ethinylestradiol + gestagen).
Inclusion criteria in the main group were reproductive age, regular menstrual cycle, no more than three sexual partners, absence of sexually transmitted infections in history, chronic inflammatory diseases of the cervix, positive results of high-risk HPV DNA test, histologically verified diagnosis of cervical neoplasia, long-term hormonal contraceptives use (combined oral contraceptives containing up to 35 μg ethinyl estradiol + gestagen) for ≥ 6 months, absence of pathological conditions of the cervix in medical history, absence of high-risk HPV DNA at the time when hormonal contraceptive pills were prescribed, as well as absence of endocrine diseases.
Inclusion criteria in the comparison group were similar to those in the main group with the exception of the use of hormonal contraceptives registered in history.
Obtaining of written informed consent from women was an obligatory condition for participation in the study.
Exclusion criteria were the age of women under 18 and over 45 years, irregular menstrual cycle, more than three sexual partners, presence of sexually transmitted infections, recurrent inflammatory diseases of the cervix, pregnancy, the presence of hormone-related disorders of female reproductive system, endocrine diseases, pathological conditions of the cervix in history, positive results of high-risk HPV DNA test at the time when hormonal contraceptive pills were proscribed for patietns in the main group, woman’s refusal to participate in the study.
Comprehensive examination of women included collection of anamnestic data, gynecological examination, colposcopy, cytological examination of cervical scrapings and histological examination of cervical biopsies to verify the diagnosis and sampling of material for polymerase chain reaction (PCR)-based HPV testing. Epithelial scrapings from the cervical canal were collected with Dacron swabs into 1.5 mL Eppendorf PCR tubes with transport medium.
Multiplex real-time PCR assay was performed for detection and genotyping of high risk HPV using «Amplysens HR HPV genotype-FL»; «AmplySens HR HPV screen-titre-FL». Viral load was calculated in genome equivalents of HPV DNA/105 cells in cervical scrapings. Threshold virus load was considered equal to HPV DNA/105 cells in cervical scrapings. HPV physical status was determined in 81 women diagnosed with HPV type 16 mono infection. Episomal form of the virus was found in the absence of HPV-E6 region and in the presence E1/E2 region, mixed form was found when E6 region was detected in the presence of the E1/E2 region, and integrated form of HPV into human DNA was found when E6 region was detected and the E1/E2 region was absent.
Assessment of the results of histological examination of cervical biopsy specimens from women in both groups was performed to verify the diagnosis of CIN. After laboratory-confirmed CIN, each group was divided into 2 subgroups depending on the disease severity: LSIL (CIN I) and HSIL (CIN II–III). The median age of the women in the main group with verified CIN was 32.3 (4.9) years: 35.1 (6.5) years in the subgroup with LSIL and 31.8 (4.5) years in the subgroup with HSIL. The median age of women in the comparison group with verified CIN was 33.2 (5) years: 28.2 (4.3) years in the subgroup with LSIL and 35.6 (3.5) years in the subgroup with HSIL.
Statistical analysis
Statistical data analysis was performed using statistical packages STATISTICA 6.1 (StatSoft), IBM SPSS Statistics 20.0, as well as Microsoft Office Excel 2010 statistical functions. The samples were tested for the normality of distribution, and it was found that the sampling distributions were not normal. Quantitative data were presented as the median values (Me) and the interquartile range (Q1–Q3). Assessment of statistical significance of differences in distribution of qualitative variables between the studied groups was performed using statistical methods. Chi-squared test (χ2-test) was used for detection of differences between the main and the comparison groups in the incidence rate of HPV16 in women with HSIL; for detection of differences between the main and the comparison groups in the incidence rate of HPV type 16 in the form of mono infection in the subgroup of women with HSIL. The incidence rate of HPV 16 among women with HSIL versus women with LSIL both in the main and in the comparison groups was detected using χ2-test. The odds ratio with 95% CI was assessed to detect statistically significant differences between the 2 groups in the incidence of cervical intraepithelial neoplasia.
The Kruskal–Wallis H-test was used to compare quantitative characteristics of 3 or more independent groups, namely, distribution of the degree of dysplasia and duration of taking oral hormonal contraceptives. Hypothesis testing was performed at critical level of significance p=0.05.
Non-parametric Mann-Whitney U test was used to assess statistical significance of differences between the two independent groups – the main and the comparison groups – in the prevalence of episomal, mixed and integrated forms of HPV type 16 mono infection. Hypothesis testing was performed at р=0.05.
Results and discussion
The results of histological examination of cervical biopsy specimens from women in 2 studied groups are shown in Table 1.
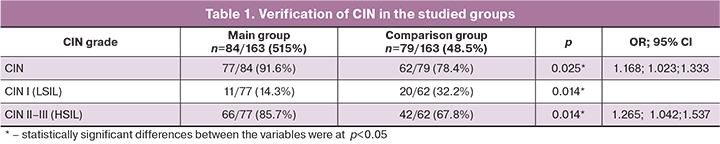
As can be seen in Table 1, comparative analysis showed statistically significant differences in the incidence rate of CIN between the main and the comparison groups (OR 1.168; 95% CI 1.023;1.333; p=0.025).
Analysis of anamnestic data on taking contraceptive pills showed that in the main group the average duration of hormonal contraceptive pills use among women with LSIL was 2 years and 5 months; and among women with HSIL – 3 years and 1 month. Distribution of CIN grades depending on duration of hormonal contraceptive pills use is presented in the Picture.
Table 2 presents the results of comparative analysis of distribution of CIN grades depending on duration of hormonal contraceptive pills use.
A comparative analysis showed significant differences in duration of hormonal contraceptive pills use. Statistically significant relationship between duration of taking hormonal pills and CIN grade was found; in women with HSIL, duration of taking hormonal contraceptives was significantly longer versus women with LSIL – 32 and 28 months, respectively (р=0.001).
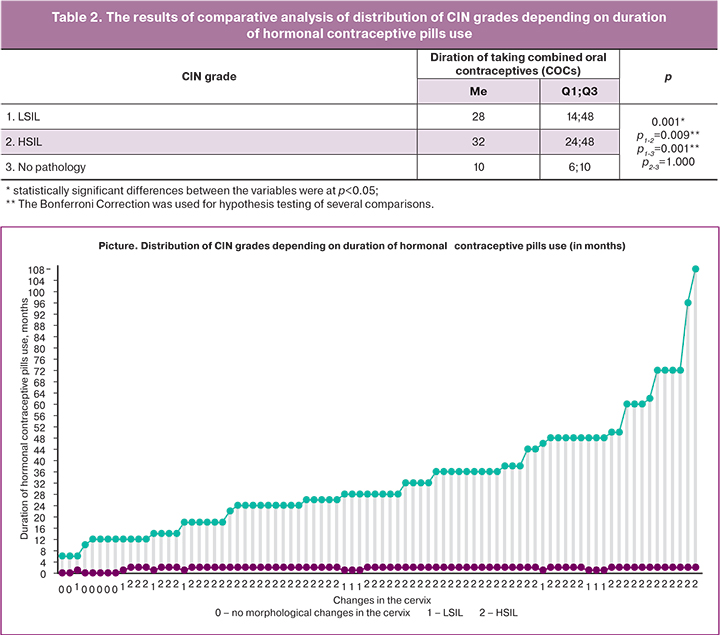
In the process of neoplastic progression, it is important to take into account not only infection with high-risk papillomavirus types, but also a number of other factors that can enhance the aggressive course of this infection contributing to rapid malignant transformation of infected cervical cells. It is probable that hormonal contraception is one of these factors. A possible mechanism underlying the association between COCs use and cervical carcinogenesis can be related to the fact that steroid hormones, both estrogens and progestogens, bind to their receptors in the cervix and change the course of papillomavirus infection inducing the mechanism of oncogenic transformation of infected cells [11]. It can be assumed that combined oral contraceptives use for 3 or more years accelerates progression to CIN in HPV-positive women. The results of our study correlate with the published data in literature: in 2000, the WHO experts, who developed medical eligibility criteria for contraceptive use, established that long-term use of oral contraceptives can accelerate progression of cervical neoplasia to microinvasive carcinoma [12]. Bright P.L. et al. (2011) demonstrated correlation between enlargement of cervical ectopion in size and COCs use within 12 months [13], and therefore, this contributes to multifocal lesions with HPV strains in endocervical crypts [14]. It is important to note that combination of HPV with long-term COCs use should be considered as particularly negative factor. Smith J.S. et al. found that in the presence of HPV the risk of CC increased by 0.9–1.3 times after 5 years of using COCs, and by 2.5 times after 10 years. In contrast, this risk increased by 0.9–1.3 only after ten years of using COCs in the group of HPV-negative women [15]. The attitude of researchers around the world towards HPV genotyping results is controversial. According to foreign authors, J.Sakamoto et al. (2018), Huang et al. (2020), the prevalence rates of HR HPV types vary among women in all countries. However, HPV type 16 dominates in women with high grade CIN. HPV type 16 has the highest carcinogenic potential and causes development of precancerous cervical lesions and invasive forms of cervical cancer in almost 70% of all cases [2, 16]. Correlation between the detection rate of HPV-16 and HPV-18 DNA and the degree of neoplastic changes in the cervix is beyond doubt and increases in direct proportion to the degree of neoplastic cervical epithelium changes reaching 16–32% in cases of LSIL, and 41–67% in cases of HSIL [17]. The results obtained in our study regarding the prevalence of HPV type 16 in women with cervical lesions are consistent with generally accepted data: both in the main and in the comparison groups, HPV type prevailed among women with HSIL versus women with LSIL (Table 3).
The obtained data showed no statistically significant differences between the main group and the comparison group in prevalence of HPV type 16 in the subgroups of women with HSIL (р3=0.44). Moreover, in all studied groups, HPV type 16 was found both in the form of mono infection and in combination with other HPV types. However, in the subgroups of women with HSIL, HPV type 16 prevailed in the form of mono infection. We found no statistically significant differences between the main group and the comparison group in the detection rate of HPV type 16 in the form of mono infection in the subgroups of women with HSIL (р3=0.65). Viral load detection in the main group showed that viral load in women with HSIL was higher versus women with LSIL; a similar trend was observed in the comparison group.
Statistical analysis showed no significant differences between the main and the comparison groups in detection of high viral load for women in the subgroups with HSIL (р3=0.745). Given the fact that cervical epithelium is sensitive to estrogen, it was suggested that the components of oral contraceptives can alter the metabolic activity and cellular proliferation of infected cells in cervical epithelium. Samir R. et al. found that with COCs use, the mechanism of cervical carcinogenesis can be triggered by overproduction of cyclooxygenase-2 and high level of Interleukin-10 (IL-10) [18]. Overexpression of cyclooxygenase-2 is a poor prognostic marker for cervical cancer, which is associated with an increased risk of tumor recurrence and metastasis [19], as it causes suppression of apoptosis and enhancement of tumor invasion to the lymph nodes and parametrium [20]. Investigation of changes in metabolic activity of infected cervical epithelial cells due to the effect of oral contraceptive use showed that the cells actively expressing HPV oncoproteins exhibited elevated level of 16α-hydroxyestrone comparable to that in breast cancer cells. One of major metabolic pathways in malignant transformation of HPV-infected cervical cells involves virus-induced changes in cellular metabolism, and the cells acquire the ability to provide conversion of estradiol to "aggressive metabolite" 16α-hydroxysterone activating oncogene E7 expression, which is responsible for malignant transformation of cervical cells [21].
Currently, most researchers share the view that hormonal contraceptive pills act as promoters of HPV-induced carcinogenesis, since sex steroids have impact on overexpression of HPV 16 oncogenes E6 and E7, which inactivate the function of tumor suppressor protein p53 and retinoblastoma protein, increasing the ability of viral DNA to transform the cells and induce oncogenic transformation of infected cells [11, 22].
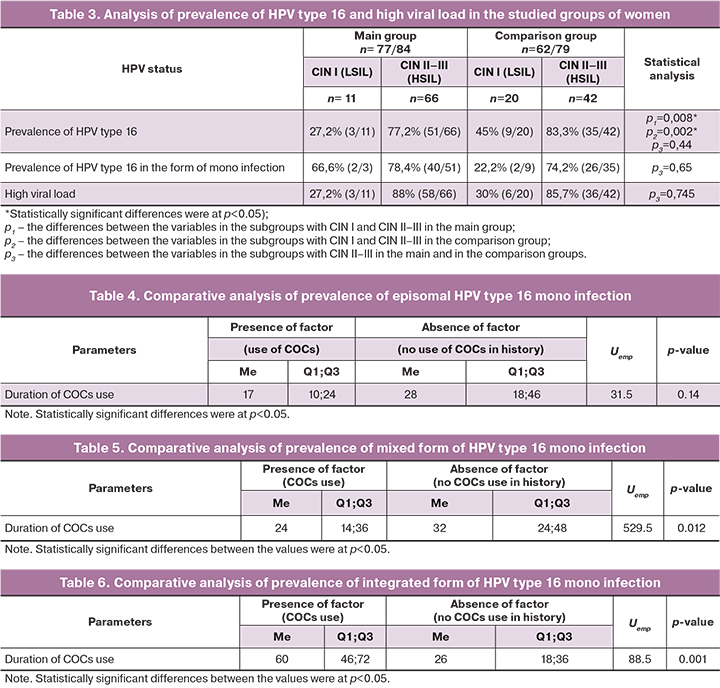
The distribution rate of episomal, mixed and integrated forms of HPV was analyzed in 81 women with HPV type 16 mono infection: in the main group, 4/84 (4.7%) women had no morphological changes in the cervix, 2/84 (2.4%) women had LSIL and 40/84 (47.6%) women had HSIL; in the comparison group, 7/79 (8.8%) women hand no morphological changes in the cervix, 2/79 (2.5%) women had LSIL and 26/79 (33%) women had HSIL. We have performed comparative analysis of prevalence and physical status of episomal, mixed and integrated forms of HPV type16 mono infection in the main group and in the comparison group. The results of comparative analysis of prevalence of episomal form of HPV type 16 mono infection in both groups are presented in Table 4.
No significant differences in prevalence of episomal form of HPV type 16 between the 2 groups were found. Thus, duration of hormonal contraceptive pills use had no effect on development of episomal HPV type 16 mono infection.
The obtained results of comparative analysis of prevalence of mixed presence of integrated and episomal forms of HPV type16 mono infection were different. As shown in Table 5, the presence of mixed form of HPV type 16 mono infection depends on duration of oral contraceptives use (Uemp.=529.5 at р=0.012). Thus, it can be assumed that mixed form of HPV type 16 occurs less often with long-term COCs use.
Prevalence of integrated form of HPV type 16 mono infection depends on duration of hormonal contraceptive pills use (Uemp.=88.5 at р=0.001) (Table 6).
Therefore, according to the results of our study, it can be assumed that long-term use of hormonal contraceptive pills by women infected with HPV type 16 mono infection can affect the physical status of human papillomavirus infection and accelerate its progression to the integrated form.
Conclusion
Detection rate of HSIL in women infected with high-risk HPV types was significantly higher with long-term use of hormonal contraceptive pills. In this regard, the issue of introduction of preventive measures against human papillomavirus infection and cervical cancer into clinical practice, including qualitative and quantitative diagnosis of HPV, cytological examination of cervical scrapings for cancer before prescribing hormonal contraceptive pills as well as dynamic surveillance during the period of using COCs remains relevant. These measures will ensure timely and effective control over possible HPV infection in women with previously HPV-negative tests, the dynamics of this infection course among previously infected patients, who take hormonal contraceptive pills with purpose of decreasing the risks of neoplastic progression and development of invasive forms of cervical cancer.
References
- Белокриницкая Т.Е., Фролова Н.И., Туранова О.В., Плетнева В.А., Шемякина К.Н., Самбуева Н.Б., Мальцева Е.Е. Результаты тестирования на вирус папилломы человека при самостоятельном и врачебном заборе материала. Гинекология. 2017; 19(1): 56-62. [Belokrinitskaya T.E., Frolova N.I., Turanova O.V. et al. Results of human papillomavirus testing on self-collected versus clinician-collected samples. Gynecology. 2017; 19(1): 56-62. (in Russian)].
- Chiantore M.V., Mangino G., Iuliano M., Capriotti L., Di Bonito P., Fiorucci G., Romeo G. Human papillomavirus and carcinogenesis: novel mechanisms of cell communication involving extracellular vesicles. Cytokine Growth Factor Rev. 2020; 51: 92-8. https://dx.doi.org/10.1016/j.cytogfr.2019.12.009.
- Hampson I.N., Oliver A.W., Hampson L. Potential effects of human papillomavirus type substitution, superinfection exclusion and latency on the efficacy of the current L1 prophylactic vaccines. Viruses. 2021; 13: 22. https://dx.doi.org/10.3390/v13010022.
- Sakamoto J., Kamiura S., Okayama K., Okodo M., Shibata T., Osaka Y. et al. Single type infection of human papillomavirus as a cause for high-grade cervical intraepithelial neoplasia and invasive cancer in Japan. Papillomavirus Res. 2018: 6: 46-51. https://dx.doi.org/10.1016/j.pvr.2018.10.001.
- Wang R., Pan W., Jin L., Huang W., Li Y., Wu D. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 2020; 471: 88-102. https://dx.doi.org/10.1016/j.canlet.2019.11.039.
- Steinbach A., Riemer A.B. Immune evasion mechanisms of human papillomavirus: An update. Int. J. Cancer. 2018; 142(2): 224-9. https://dx.doi.org/10.1002/ijc.31027.
- Doorbar J. Molecular biology of human papillomavirus infection and cervical cancer. Clin. Sci. 2006; 110(5): 525-41. https://dx.doi.org/10.1042/cs20050369.
- Tornesello M.L., Buonaguro L., Rossi P.G., Buonaguro F.M. Viral and cellular biomarkers in the diagnosis of cervical intraepithelial neoplasia and cancer. Biomed. Res. Int. 2013; 2013: 1-10. https://dx.doi.org/10.1155/2013/519619.
- Прилепская В.Н., Байрамова Г.Р., Асатурова А.В., Андреев А.О., Перемыкина А.В., Пронина В.А. Современные представления о предикторах и методах профилактики рецидивов цервикальной интраэпителиальной неоплазии после петлевой электроэксцизии. Акушерство и гинекология. 2020; 12: 81-8. [Prilepskaya V.N., Bairamova G.R., Asaturova A.V., Andreyev A.O., Peremykina A.V., Pronina V.A. Сurrent understanding of predictors and methods for preventing recurrent cervical intraepithelial neoplasia after loop electrosurgical excision procedure. Оbstetrics and Gynecology. 2020; 12: 81-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.12.81-88.
- Gonzalez R., Reingold B.K., Gao X., Gaidhu M.P., Tsushima R.G., Unniappan S. Nesfatin-1 exerts a direct, glucose-dependent insulinotropic action on mouse islet beta- and MIN6 cells. J. Endocrinol. 2011; 208(3): R9-R16. https://dx.doi.org/10.1530/joe-10-0492.
- Roura E., Travier N., Waterboer T., de Sanjosé S., Bosch F.X., Pawlita M. et al. The influence of hormonal factors on the risk of developing cervical cancer and pre-cancer: results from the EPIC cohort. PLoS One. 2016; 11(1): e0147029. https://dx.doi.org/10.1371/journal.pone.0147029.
- World Health Organization (WHO). Improving access to quality care in family planning. Medical eligibility criteria for contraceptive use. 2nd ed. WHO; 2000.
- Bright P.L., Norris T.A., Morrison C.S., Wong E.L., Kwok C., Yacobson I. et al. Hormonal contraception and area of cervical ectopy: a longitudinal assessment. Contraception. 2011; 84(5): 512-9. https://dx.doi.org/10.1016/j.contraception.2011.02.002.
- Papoutsis D., Panikkar J., Underwood M., Blundell S., Sahu B., Blackmore J., Reed N. Endocervical crypt involvement by CIN2–3 as a predictor of cytology recurrence after excisional cervical treatment. J. Low. Genit Tract. Dis. 2015; 19(4): 311-8. https://dx.doi.org/10.1097/LGT.0000000000000128.
- Smith J.S., Green J., Berrington de Gonzalez A., Appleby P., Peto J., Plummer M. et al. Cervical cancer and use of hormonal contraceptives: a systematic review. Lancet (London). 2003; 361(9364): 1159-67. https://dx.doi.org/10.1016/s0140-6736 (03)12949-2.
- Rungea A.S., Bernsteina M.E., Lucasa A.N., Tewari K.S. Cervical cancer in Tanzania: A systematic review of current challenges in six domains. Gynecol. Oncol. Rep. 2019; 29: 40-7. Dx.https://dx.doi.org/10.1016/j.gore.2019.05.008.
- Байрамова Г.Р., Баранов И.И., Ежова Л.С., Трофимов Д.Ю., Припутневич Т.В., Амирханян А.С., Старинская А.М. Плоскоклеточные интраэпителиальные поражения шейки матки: возможности ранней диагностики и тактики ведения пациенток. Доктор.Ру. 2019; 11: 61-7. [Bairamova G.R., Baranov I.I., Ezhova L.S., Trofimov D.Yu., Priputnevich T.V., Amirkhanyan A.S., Starinskaya A.M. Squamous Intraepithelial Cervix Lesions: Possible Early Diagnostics and Management. Doctor.Ru. 2019; 11(166): 61-7. (in Russian)]. Pekar G, Hellberg D. https://dx.doi.org/10.31550/1727-2378-2019-166-11-61-67.
- Samir R., Asplund A., Tot T., Pekar G., Hellberg D. Oral contraceptive and progestin-only use correlates to tissue tumor marker expression in women with cervical intraepithelial neoplasia. Contraception. 2012; 85(3): 288-93. https://dx.doi.org/10.1016/j.contraception.2011.09.001.
- Young J.L., Jazaeri A.A., Darus C.J., Modesitt S.C. Cyclooxygenase-2 in cervical neoplasia: a review. Gynecol Oncol. 2008; 109: 140-5. https://dx.doi.org/10.1016/j.ygyno.2008.01.008.
- Ryu H.S., Chang K.H., Yang H.W., Kim M.S., Kwon H.C., Oh K.S. High cyclooxygenase-2 expression in stage IB cervical cancer with lymph node metastasis or parametrial invasion. Gynecol. Oncol. 2000; 76(3): 320-5. https://dx.doi.org/10.1006/gyno.1999.5690.
- Киселев В.И., Ашрафян Л.А., Бударина С.О., Киселев О.И., Пальцев М.А., Кулаков В.И., Прилепская В.Н. Этиологическая роль вируса папилломы человека в развитии рака шейки матки: генетические и патогенетические механизмы, возможности терапии и профилактики. Consilium medicum. Гинекология. 2004; 6(4): 174-80. [Kiselev V.I., Ashrafyan L.A., Budarina S.O. et al. Etiological role of human papillomavirus in the development of cervical cancer: genetic and pathogenetic mechanisms, possibilities of therapy and prevention. Consilium medicum. Ginekologiya. 2004; 6(4). (in Russian)].
- Chung S.H., Wiedmeyer K., Shai A., Korach K.S., Lambert P.F. Requirement for estrogen receptor alpha in a mouse model for human papillomavirus-associated cervical cancer. Cancer Res. 2008; 68(23): 9928-34. https://dx.doi.org/10.1158/0008-5472.can-08-2051.
Received 05.07.2021
Accepted 29.10.2021
About the Authors
Lidia A. Klyukina, post-graduate student of the Department of Obstetrics and Gynecology No. 1, N.V. Sklifosovsky Institute of Clinical Medicine, I.M. SechenovFirst Moscow State Medical University, Ministry of Health of Russia, lidiaklyukina@mail.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Elena A. Sosnova, Dr. Med. Sci., Professor of the Department of Obstetrics and Gynecology No. 1, N.V. Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov
First Moscow State Medical University, Ministry of Health of Russia, sosnova-elena@inbox.ru, https://orcid.org/0000-0002-1732-6870,
119991, Russia, Moscow, Trubetskaya str., 8-2.
Anton A. Ishchenko, Ph.D., Senior Research Associate, Head of the Center for Gynecology and New Reproductive Technologies, Medical and Rehabilitation Center,
Ministry of Health of the Russian Federation, ra2001_2001@mail.ru, 125367, Russia, Moscow, Ivankovskoe highway, 3.
Corresponding author: Lidia A. Klyukina, lidiaklyukina@mail.ru
Author’s contributions: Sosnova E.A., Ischenko A.A., Klyukina L.A. – the concept and design of the study; Klyukina L.A. –material collection and processing, statistical data processing, writing the article; Sosnova E.A., Ischenko A.A. – editing the article.
Conflicts of interest: The authors declare that they have no conflict of interests.
Funding: The study was carried out without any sponsorship.
Patients’ Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Klyukina L.A., Sosnova E.A., Ischenko A.A. The role of combined oral contraceptives in cervical intraepithelial neoplasia occurrence associated with human papillomavirus infection.
Akusherstvo i Gynecologia/ Obstetrics and Gynecology. 2021; 12: 102-109 (in Russian)
https://dx.doi.org/10.18565/aig.2021.12.102-109