Opportunities for noninvasive diagnosis of liver damage in pregnant women with preeclampsia and HELLP syndrome
Objective. To develop a comprehensive non-invasive diagnosis of liver damage in pregnant women.Fedyunina I.A., Strizhakov A.N., Timokhina E.V., Aslanov A.G.
Subjects and methods. A prospective examination was made in 117 pregnant women who were divided into two groups: a study group included women whose pregnancy was complicated by preeclampsia (PE) and HELLP syndrome; a control group consisted of 40 women with uncomplicated pregnancy. Liver function was evaluated using the authors’ designed score scale based on the serum biochemical parameters that most fully reflected the involvement of the liver in metabolic processes. The non-invasive procedure of a “Fibrotest” was first used in pregnant women in order to detect structural changes in liver tissue.
Results. All women in the study group were observed to have changes in liver function of varying degrees of severity. As PE increased, the functional state of the liver progressively deteriorated up to an absolute decrease in its function. The detected liver functional changes in PE and HELLP syndrome were accompanied by morphostructural rearrangement in the organ, which is confirmed by Fibrotest results.
Conclusion. The authors’ proposed comprehensive assessment of the liver condition using the score scale and the Fibrotest procedure makes it possible to timely detect the extent of liver damage, to choose rational obstetric tactics, to evaluate the efficiency of therapy, and to follow up the reversal of pathological changes in the organ in the postpartum period.
Keywords
Acute liver failure in obstetric patients constantly attracts the attention of researchers from various specialties, as this disease results in severe consequences for the mother and fetus [1]. In most cases acute renal failure in pregnant women and women who have just given birth is caused by acute fatty liver dystrophy, HELLP syndrome, as well as the consequences of septic and hemorrhagic shock [1, 2]. One of the most serious complications of hepatic disease in pregnancy is HELLP syndrome which is a variant of thrombotic microangiopathy; its clinical manifestations are free hemolysis in blood serum and urine, increased levels of hepatic enzymes, and thrombocytopenia [3]. Thrombotic microangiopathy which is caused by thrombosis of arterioles and capillaries leads to fibrin deposition in the hepatic sinuses, stenosis of the hepatic artery and, as a result, a decrease in portal blood flow and ischemic damage to the organ [3, 4]. Therefore, the function of the liver is impaired due to serious morphological changes, which determine the outcome and long-term consequences of HELLP syndrome.
The high incidence of the near miss condition, as well as fatal outcomes associated with severe preeclampsia and HELLP syndrome, is due to the fast development of this complication, rapidly progressing liver failure, and also late diagnosis and underestimation of the severity of the woman’s condition [4–6].
Medication therapy and detoxification methods have not been proven to be effective in patients with advanced liver failure associated with preeclampsia and HELLP syndrome, therefore, obstetric tactics in this situation consist in timely delivery. Due to this fact, it is necessary to reveal even minor clinical and laboratory manifestations of liver damage in pregnant women.
Biopsy is known to be the gold standard for diagnosing the severity of liver damage; however, this technique is limited in use in pregnant women due to possible technical difficulties during the procedure and the risk of intra-abdominal bleeding [7].
The search for new non-invasive tests is relevant today; these tests can be safe and easily used in routine obstetric practice, allowing clinicians to assess both functional and structural changes in the organ. One of these tests is “Fibrotest” (Biopredictive, France) which determines indirect biochemical markers of liver fibrosis in the blood serum and reflects the presence and severity of morphological changes in the liver tissue [8, 9]. In our study, we evaluated the possibility of using this method in pregnant women with complicated pregnancy.
Liver function is usually assessed on the basis of biochemical indicators, namely, markers of cytolytic, cholestatic syndrome, as well as liver cell failure. The most sensitive markers of hepatic dysfunction are still searched for. In order to provide the most complete and comprehensive assessment of liver function, we developed a score scale based on 10 biochemical parameters of blood serum which best reflect the participation of the liver in all metabolic processes.
The objective of the study was to develop comprehensive non-invasive methods for diagnosing liver damage in pregnant women.
Materials and methods
A comprehensive prospective study of 117 pregnant women was conducted at the maternity hospital of S.S. Yudin State Clinical Hospital in the period from 2019 to 2020.
Pregnant women with preeclampsia and HELLP syndrome composed the main group (n=77), which was divided into three subgroups: the 1st subgroup consisted of patients with moderate preeclampsia (n=38), the 2nd subgroup included the patients with severe preeclampsia (n=27), and the 3rd subgroup consisted of patients with HELLP syndrome (n=12). The division of patients into subgroups was based on the criteria described in the clinical recommendations of the Ministry of Health of the Russian Federation dated June 7, 2016 “Hypertensive Disorders in Pregnancy, Labor and Postpartum Period. Preeclampsia. Eclampsia”.
The control group consisted of women with a normal course of pregnancy (n=40).
Patients with a previous history of the diseases of the liver and hepatobiliary system prior to pregnancy were excluded from the study.
The analysis of the average age of the patients and the average gestational age revealed no statistically significant differences between the patients of the main and control groups.
All pregnant women underwent a comprehensive clinical, laboratory and instrumental examination in accordance with the Order of the Ministry of Health of the Russian Federation dated November 01, 2012 No. 572n “On Medical Regulations for Providing Medical Care in Obstetrics and Gynecology”.
The functional state of the liver was routinely assessed by a detailed biochemical study of blood serum for the main markers, which are indicators of liver dysfunction. In order to assess the protein synthetic function of the liver, the concentration of total protein, albumin, and fibrinogen in the serum was evaluated. Participation in carbohydrate and fat metabolism was evaluated by determining the level of glucose, urea, and total cholesterol. Liver function in the processes of transamination and deamination was evaluated using the level of hepatic transaminases. Damage to the membranes and intracellular structures of hepatocytes was assessed on the basis of the levels of transaminases, alkaline phosphatase (ALP), lactate dehydrogenase (LDH), total and indirect bilirubin.
On the basis of a comprehensive biochemical blood test, we developed a score system that allows us to evaluate liver function on a scale ranging from the absence of impairments to absolute liver dysfunction (Table 1). The degrees of liver dysfunction were divided according to the International Classification of Functioning, Disability and Health (WHO, 2001) [10], where a decrease in organ function by 0–4% corresponds to the absence of disorders, a decrease in function by 5–24% – to slight disorders, a decrease in function by 25–49% – to moderate disorders, by 50–95% – to severe disorders, by 95–100% – to absolute disorders.
Thus, all the results of the biochemical study were ranked from slight to absolute liver dysfunction according to the scale.
The values of biochemical parameters that are within the reference range were considered as the absence of liver function disorders (0–4%).
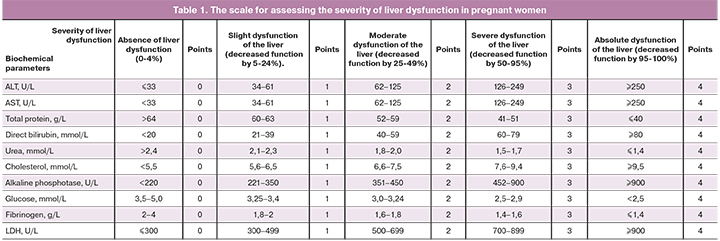
Taking into account that HELLP syndrome leads to the development of severe liver failure in pregnant women, the biochemical parameters of liver function in pregnant women with HELLP syndrome were regarded as absolute liver dysfunction (95–100%) (Table 1).
The reference value for ALT is the level below 33 U/L and was conditionally defined by us as one norm. The average ALT value in the group with HELLP syndrome was 178.7 (17.3), which is approximately 5 norms. Thus, ALT values above 161.1 U/L, or exceeding 5 norms, were regarded as absolute liver dysfunction (95-100% decrease in organ function).
ALT values corresponding to 25–49% of the indicators of absolute liver dysfunction are classified as moderate liver dysfunction (Table 1). ALT values corresponding to 5–24% of the indicators of absolute impairment are classified as slight liver dysfunction, and values corresponding to 50–94% are classified as severe liver dysfunction.
All biochemical parameters were distributed using the same principle based on the scale (Table 1).
Moreover, assessment of the severity of liver dysfunction was based on a score system, where the value of each biochemical marker is ranked from 0 to 4 points. The level of the biochemical indicator corresponding to the absence of liver dysfunction was assessed as 0 points, slight liver dysfunction as 1 point, moderate liver dysfunction as 2 points, severe liver dysfunction as 3 points, and absolute liver dysfunction as 4 points.
Thus, the sum of points from 0 to 2 corresponds to the absence of liver dysfunction, from 3 to 19 points refers to slight liver dysfunction, from 20 to 29 points corresponds to moderate liver dysfunction, from 30 to 37 points refers to severe liver dysfunction, and from 38 to 40 points refers to absolute liver dysfunction.
In our study, we used the FibroTest technique in pregnant women for the first time to detect structural changes in the liver tissue associated with a complicated course of pregnancy. The FibroTest technique consists in calculating the degree of histological changes in the liver according to a patented algorithm (Biopredictive, France), based on serological markers of liver fibrosis (total bilirubin, haptoglobin, alpha-2-macroglobulin, apolipoprotein A1, gamma-glutamyltranspeptidase) and clinical parameters (height, weight, age, sex), followed by conversion of the obtained numerical values into the generally recognized METAVIR system, reflecting the four stages of fibrosis in the liver (F0–F4). Venous blood was obtained from women on an empty stomach; biochemical analysis of blood serum was performed in the clinical and diagnostic laboratory of the maternity hospital of S.S. Yudin State Clinical Hospital, and the FibroTest technique was used in the INVITRO laboratory.
Statistical analysis
The statistical analysis of the results was performed using the program STATISTICA 13.3 (StatSoft. Inc).
Arithmetic mean (M) and standard deviation (SD) were used to represent the quantitative data. Student’s t-test was calculated to compare the average values, and the results were compared with the critical value. The difference in the results was considered as statistically significant at the level of p<0.05.
Results and discussion
The liver function was evaluated on the basis of a comprehensive biochemical study of blood serum and indicators that best reflect the participation of the liver in protein, carbohydrate, and fat metabolism. The results are presented in Table 2.
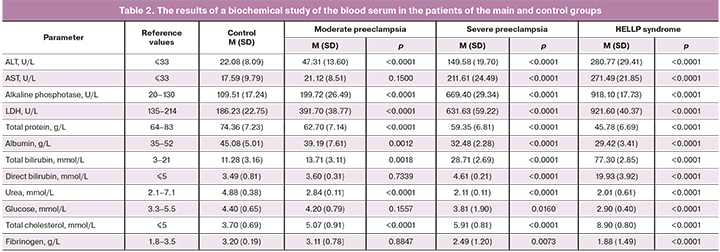
All subgroups of the main group showed an increase in ALT and ALP which are markers of cytolytic syndrome, as well as LDH, which is a marker of hemolysis and hepatic cytolysis. This indicator in the group with HELLP syndrome showed a significant increase of almost 9 times in comparison with the control group and amounted to 921.6 (40.4) U/L.
LDH is not known to be highly specific to hepatic tissue, because it is found in many other organs, such as the heart, lungs, etc. However, an increase in this enzyme in combination with a significant increase in transaminases in the blood serum indicates the hepatic genesis of the lesion.
ALT and AST indicators also demonstrate that the liver can participate in transamination and deamination reactions.
An increase in enzyme ALP which is tightly bound to the hepatocyte membrane results from hepatotoxicity, and possibly from damage to the liver parenchyma. The average values of this enzyme in patients with moderate preeclampsia were twice higher than those in the group of patients with normal course of pregnancy. The level of this enzyme in the group of patients with severe preeclampsia was 6 times higher than in the control group. The highest values of this enzyme were observed in women with HELLP syndrome and amounted to 918.1 (17.7) U/L, which was 9 times higher than the average values of the control group.
Thus, an increase in the level of ALT (cytosolic enzyme) in the blood serum, as well as enzymes associated with various structures of hepatocytes, namely, ALP, LDH, and AST, is a clinical manifestation of cytolytic syndrome; the severity of cytolysis and the extent of liver cell damage correlate with the severity of preeclampsia.
A progressive decrease in total protein, albumin, fibrinogen, urea, and glucose associated with increasing severity of preeclampsia suggests liver cell failure and a decrease in protein synthesis and detoxifying functions of the liver.
Taking into account the fact that most of the biochemical markers of liver damage are not specific to the liver tissue and can be found in other organs, we have proposed a comprehensive approach to determine a number of indicators that best reflect the participation of the liver in metabolic processes and are markers of the main syndromes of liver damage, such as cytolytic, cholestatic, and liver cell failure.
In this regard, we developed a scale and a system for evaluating liver function using 10 biochemical markers of liver damage. These markers, namely, total protein, ALT, AST, ALP, LDH, total bilirubin, cholesterol, urea, glucose, and fibrinogen, were observed in most patients of the main group (Table 1).
The liver function of women in the control and main groups was evaluated using the scale.
 All women in the control group (n=40) had 0–2 points, which corresponded to the absence of liver function disorders.
All women in the control group (n=40) had 0–2 points, which corresponded to the absence of liver function disorders.
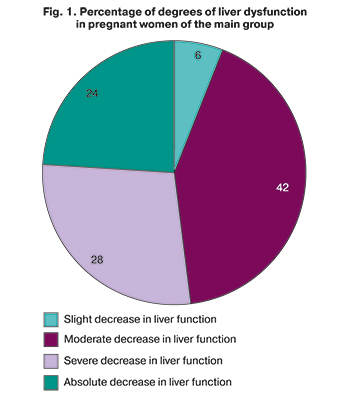
All women of the main group had changes in liver function of varying degrees of severity (Fig. 1).
In most cases (42%), patients of the main group had indicators of liver function that corresponded to moderate disorders. Severe and absolute liver dysfunction was diagnosed in 28 and 24% of cases, respectively. Only 6% of patients in the main group were diagnosed with slight changes in liver function.
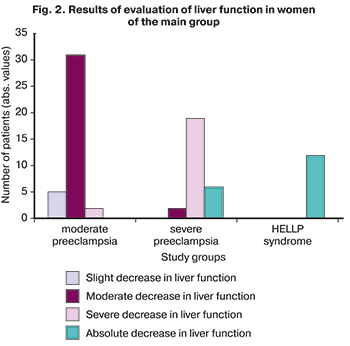
The group of patients with moderate preeclampsia showed changes in liver function, ranging from slight to severe. In most cases, patients with moderate preeclampsia had moderate liver dysfunction (Fig. 2).
Patients with severe preeclampsia had deviations in the biochemical parameters of liver function, which corresponded to moderate or absolute dysfunction (Fig. 2).
Absolute liver dysfunction was observed in 100% of women with HELLP syndrome (Fig. 2).
 Morphostructural changes in the liver in women with complicated pregnancy and liver dysfunction of various severity were evaluated using the FibroTest technique.
Morphostructural changes in the liver in women with complicated pregnancy and liver dysfunction of various severity were evaluated using the FibroTest technique.
There were changes typical for the F1 stage of the METAVIR system in 8 patients (40%) in the subgroup with moderate preeclampsia; these changes could be suggestive of the initial changes in the hepatic tissue. The remaining 12 patients (60%) with moderate preeclampsia showed F0 degree of the histological index scale using the FibroTest technique; this indicator proves that there were no morphostructural changes in the liver. Thus, there is hypoxic damage to hepatocytes and their death followed by the formation of the connective tissue and fibrosis in patients with moderate preeclampsia.
Patients with severe preeclampsia showed more severe structural changes in the hepatic tissue. Thus, F1 stage was detected in 12 patients (60%) with severe preeclampsia, and F2 stage was detected in 8 (40%) patients.
The most severe morphostructural changes in hepatic tissue were observed in the subgroup of patients with HELLP syndrome, where 4 patients (33%) had the results of the FibroTest technique corresponding to the F1 stage, and 6 patients (50%) had results corresponding to the F2 stage.
Advanced fibrosis with multiple porto-central septa without cirrhosis (METAVIR, F3-stage) was detected in 2 (17%) patients of this subgroup. Thus, organic irreversible changes of varying severity were observed in all patients of this subgroup.
Therefore, our study proves that there is a decrease in liver function even in patients with moderate preeclampsia. Along with the increase in degree of preeclampsia, the functional state of the liver progressively deteriorates, up to an absolute decrease in its function. It is worth noting that progressive decrease in liver function which is accompanied by an increase in the severity of preeclampsia is probably associated with damage to the organ parenchyma due to microangiopathy and the formation of microthrombi, as well as hypoxic damage to hepatocytes and multiple hemorrhages in the hepatic tissue.
The scale of assessment of liver dysfunction developed by us makes it possible to objectively identify the severity of the dysfunction. The most severe impairment of liver function was found in women with severe preeclampsia and HELLP syndrome.
Impaired liver function (from moderate to absolute) in severe preeclampsia and HELLP syndrome is accompanied by morphostructural changes in the organ, and it was confirmed by the results of the FibroTest technique.
Severe and absolute impairments of liver function undoubtedly require changes in obstetric tactics and performing urgent delivery. Based on the fact that women with preeclampsia and HELLP syndrome have severe changes in the liver tissue corresponding to the F2–F3 stages using the METAVIR scale, such women need outpatient dynamic monitoring of liver function in the postpartum period.
Conclusion
Thus, early detection of preclinical signs of liver failure in pregnant women with preeclampsia is extremely important. The use of scale proposed by us makes it possible to conduct an early comprehensive assessment of the liver condition in pregnant women with preeclampsia and to rank patients according to the degree of functional impairment, namely, from a slight decrease in organ function to an absolute one. It is recommended to combine the biochemical assessment of the degree of liver dysfunction with the study of morphostructural changes using the non-invasive FibroTest technique to obtain a more complete picture of the liver condition and the severity of the woman’s condition. The obtained results should be taken into account when choosing obstetric tactics. Thus, if there is a slight dysfunction of the liver, it is possible to include hepatoprotectors in the complex therapy of preeclampsia with the subsequent dynamic control of the organ function using the scale. The progression of liver failure will contribute to a timely decision on early delivery.
Taking into account that damage to the liver in preeclampsia and HELLP syndrome is not limited to functional changes, but can be often accompanied by structural changes in the organ of various degrees of severity, it is possible to use the FibroTest technique for a more complete assessment of the damage to the liver in pregnant women with preeclampsia. It is obvious that in some cases, pregnant women with pathological processes in the liver accompanied by the development of preeclampsia require a long recovery after delivery; therefore, it is advisable to monitor the biochemical parameters of liver function in the postpartum period and, if necessary, to correct liver dysfunction with medications.
References
- Куликов А.В., Шифман Е.М., Спирин А.В. Печеночная патология в акушерстве. Российский медицинский журнал. 2014; 20(2): 37-44. [Kulikov A.V., Shifman E.M., Spirin A.V. Hepatic pathology in obstetrics. Russian medical journal. 2014; 20(2): 37-44. (in Russian)].
- Министерство здравоохранения Российской Федерации. Гипертензивные расстройства во время беременности, в родах и послеродовом периоде. Преэклампсия. Эклампсия. Клинические рекомендации (протокол лечения). М.; 2016. [Ministry of Health of the Russian Federation. Hypertensive disorders during pregnancy, childbirth and the puerperium. Preeclampsia. Eclampsia. Clinical guidelines (Treatment protocol). M.; 2016. (in Russian)].
- Макацария А.Д., Бицадзе В.О., Хизроева Д.Х., Акиньшина С.В. Тромботические микроангиопатии в акушерской практике. М.: ГЭОТАР-Медиа; 2017. 304 с. [Makatsaria A.D., Bitsadze V.O., Khizroeva D.Kh., Akinshina S.V. Thrombotic microangiopathies in obstetric practice. M.: GEOTAR-Media; 2017. 304 p. (in Russian)].
- Тимохина Е.В., Стрижаков А.Н., Белоусова В.С., Асланов А.Г., Богомазова И.М., Афанасьева Н.В., Самойлова Ю.А., Ибрагимова С.М., Кечина А.М. HELLP-синдром как жизнеугрожающее состояние: современные особенности течения. Акушерство, гинекология и репродукция. 2019; 13(1): 35-42. [Timokhina E.V., Strizhakov A.N., Belousova V.S., Aslanov A.G., Bogomazova I.M., Afanasyeva N.V., Samoilova Yu.A., Ibragimova S.M., Kechina A.M. HELLP syndrome as a life-threatening condition: modern features of the course. Obstetrics, gynecology and reproduction. 2019; 13 (1): 35-42. (in Russian)].
- Стрижаков А.Н., Тимохина Е.В., Федюнина И.А., Игнатко И.В., Асланов А.Г., Тернова Д.Ю., Пицхелаури Е.Г. Биохимические маркеры поражения печени при HELLP-синдроме. Вопросы гинекологии, акушерства и перинатологии. 2019; 18(4): 59-65. [Strizhakov A.N., Timokhina E.V., Fedyunina I.A., Ignatko I.V., Aslanov A.G., Ternova D.Yu., Pitskhelauri E.G. Biochemical markers of liver damage in HELLP syndrome. Questions of gynecology, obstetrics and perinatology. 2019; 18 (4): 59-65. (in Russian)].
- Ивашкин В.Т., Маевская М.В., Павлов Ч.С., Сиволап Ю.П., Луньков В.Д., Жаркова М.С., Масленников Р.В. Клинические рекомендации Российского общества по изучению печени по ведению взрослых пациентов с алкогольной болезнью печени. Российский журнал гастроэнтерологии, гепатологии, колопроктологии. 2017; 27(6): 20-40. [Ivashkin V.T., Maevskaya M.V., Pavlov Ch.S., Sivolap Yu.P., Lunkov V.D., Zharkova M.S., Maslennikov R.V. Clinical guidelines of the Russian Society for the Study of the Liver for Management adult patients with alcoholic liver disease. Russian journal of gastroenterology, hepatology, coloproctology. 2017; 27(6): 20-40. (in Russian)].
- Вялов С.С. Скрининговые методы выявления фиброза печени. Архивъ внутренней медицины. 2012; 3: 20-6. [Vyalov S.S. Screening methods for detecting liver fibrosis. Archives of internal medicine. 2012; 3: 20-6. (in Russin)].
- Boursier J., Vergniol J., Guillet A., Hiriart J.-B., et al. Diagnostic accuracy and prognostic significance of blood fibrosis tests and liver stiffness measurement by FibroScan in non-alcoholic fatty liver disease. J. Hepatol. 2016; 65(3): 570-8. https://dx.doi.org/10.1016/j.jhep.2016.04.023.
- Волынец Г.В., Евлюхина Н.Н., Филин А.В., и др. Определение степени нарушения структуры печени и выраженности портальной гипертензии у детей. Экспериментальная и клиническая гастроэнтерология. 2015; 1: 28-35. [Volynets G.V., Evlyukhina N.N., Filin A.V., Surkov A.N., Potapov A.S., Shavrov A.A., Zelikovich E.I. Determination of the degree of liver structure disturbance and severity of portal hypertension in children. Experimental and clinical gastroenterology. 2015; 1: 28-35. (in Russian)].
Received 03.11.2020
Accepted 08.06.2021
About the Authors
Irina A. Fedyunina, PhD, assistant of the Department of Obstetrics, Gynecology and Perinatology of the Medical Faculty, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University). Tel.: +7(499)782-30-45. E-mail: irina.fedjunina@mail.ru. ORCID: 0000-0002-9661-5338.119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Elena V. Timokhina, Dr. Med. Sci., Professor of the Department of Obstetrics, Gynecology and Perinatology of the Medical Faculty, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University). Tel.: +7(499)782-30-45. E-mail: elena.timokhina@mail.ru. ORCID: 0000-0001-6628-0023.
119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Alexander N. Strizhakov, Academician of the Russian Academy of Sciences, Professor, Head of the Department of Obstetrics, Gynecology and Perinatology of the Medical Faculty I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University). Tel.: +7(499)782-30-45. ORCID: 0000-0001-7718-7465.
119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Alexander G. Aslanov, PhD, associate professor of the Department of Obstetrics, Gynecology and Perinatology of the Medical Faculty, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University). Tel.: +7(499)782-30-45. 119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
For citation: Fedyunina I.A., Strizhakov A.N., Timokhina E.V., Aslanov A.G. Opportunities for noninvasive diagnosis of liver damage in pregnant women
with preeclampsia and HELLP syndrome.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 6: 73-79 (in Russian)
https://dx.doi.org/10.18565/aig.2021.6.73-79



