Совершенствование медицинских технологий позволило разработать методы преодоления бесплодия при заболеваниях репродуктивной системы, которые ранее считались практически приговором в отношении реализации детородной функции. К такой патологии, несомненно, относится эндометриоидная болезнь (ЭБ), проявляющая себя, как хроническое, системное, прогрессирующее, рецидивирующее заболевание с генетическими девиациями и эпигенетическими особенностями, определяющими аномальное функционирование иммунобиологического надзора, проангиогенный и воспалительный паттерны [1, 2]. Несмотря на отсутствие ясного понимания путей формирования эндометриоза, повышение эффективности комплексного персонифицированного лечения значительно увеличило количество беременных женщин группы высокого риска, при отсутствии общепризнанных отработанных периконцепционных превентивных мероприятий, направленных на оптимизацию как ключевых ранних гестационных событий (нидацию, инвазию, плацентацию), так и поздних сроков беременности [3]. Более высокие гестационные риски при ЭБ, в первую очередь, связаны с системным воспалением, на фоне которого наступает беременность, а также обусловлены исходным негативным влиянием эндометриоза на анатомо-функциональное состояние репродуктивной системы, как на периферическом (снижение овариального резерва, рецептивности эутопического эндометрия, нарушение анатомии половых органов и др.), так и центральном уровнях (дисфункция системы «гипоталамус-гипофиз») с нарушением реципрокных связей [4].
Многочисленные исследования и практические наблюдения свидетельствуют о разнонаправленном влиянии беременности на течение эндометриоза. В работах [5, 6] отмечается позитивная роль беременности в уменьшении активности эндометриоза, прогрессировании процесса, клинических проявлений. Однако, в других исследованиях [7, 8] высказывается противоположное мнение, основанное на данных об отсутствии регресса эндометриоидных гетеротопий; увеличении частоты и объема эндометриом при беременности, ведущих к формированию абсцесса или разрыва кисты яичника [9]; повышении риска перфорации различных тканей и органов (сосудов, аппендикса, кишечника, мочевого пузыря), приводящей к спонтанному массивному кровотечению в период гестации [10]. Ряд авторов отмечает, что значительное число наблюдений прогрессирования эндометриоза во время беременности не учитывается статистически, в связи с отсутствием объективной доказательной базы, ограниченными возможностями инвазивных исследований при беременности [11, 12]. Обратной стороной проблемы является влияние ЭБ на течение самой беременности, что реализуется в росте частоты ранних репродуктивных потерь, преждевременных родов, плацентарной недостаточности и плацента-ассоциированной патологии плода, преждевременной отслойки нормально расположенной плаценты, аномалий плаценты, ее расположения и прикрепления, родоразрешения путем операции кесарева сечения [13, 14]. Тактика врача при данных осложнениях беременности отработана и представлена в клинических рекомендациях. Однако сложности диагностики и своевременной тактики сохраняются при редких осложнениях ЭБ у беременных, проявляющихся жизнеугрожающими состояниями, в частности, массивными кровотечениями вследствие перфорации в области расположения эндометриоидных гетеротопий.
В информационных базах данных PubMed, Scopus, eLibrary.Ru, Medline, Cochrane, Hinari представлены единичные наблюдения внутрибрюшного кровотечения у беременных, обусловленного активностью эндометриоидного процесса [10, 15–20]. В связи с отсутствием четких рекомендаций по дифференциальной диагностике и тактике ведения данных пациенток, каждый подтвержденный случай представляет научно-практический интерес.
Представленное клиническое наблюдение демонстрирует сложность диагностики и благоприятный исход у беременной с внутрибрюшным кровотечением вследствие ЭБ.
Клиническое наблюдение
Пациентка М., 35 лет, обратилась в приемное отделение перинатального центра ГБУЗ «СОКБ им. В.Д. Середавина» 24.09.2022 в 00:30 ч. с жалобами на тянущие боли внизу живота, беспокоящие с 21.00 ч. 23.09.2022 и усиливающиеся в течение последнего часа. Акушерско-гинекологический анамнез: менструации с 13 лет, регулярные, болезненные, умеренные, по 4 дня, через 28 дней. Первый день последней менструации: 17.02.2022. Половая жизнь с 17 лет, применение методов контрацепции отрицает. В течение 10 лет страдает хроническим пиелонефритом.
В 2020 г. при выполнении ультразвукового исследования (УЗИ) малого таза в рамках обследования по поводу первичного бесплодия и хронической тазовой боли диагностировано анэхогенное образование правого яичника с густой мелкодисперсной взвесью, размерами 5×4,5 см, аваскулярное в режиме цветового допплеровского картирования. В этом же году в гинекологическом отделении ГБУЗ «СОКБ им. В.Д. Середавина» проведено оперативное лечение с лапароскопической визуализацией: интраоперационно обнаружено объемное образование правого яичника, размерами 6×5 см с плотной темно-синей капсулой и густым содержимым шоколадного цвета, мелкие эндометриоидные гетеротопии багрового цвета на париетальной брюшине малого таза, единичные спайки с правой боковой поверхностью таза, задним листком широкой связки матки. Выполнена энуклеация капсулы кисты правого яичника, каутеризация единичных очагов эндометриоза, адгезиолизис. Согласно гистологическому заключению – эндометриоидная киста. В послеоперационном периоде назначены прогестагены в циклическом режиме.
Настоящая беременность 1-я, самопроизвольная. На учете в женской консультации с 7–8 недель беременности, I и II триместр – без особенностей.
Общее состояние удовлетворительное. Голова не болит, зрение ясное. Температура тела 36,6°С. Тошноту, рвоту и изжогу отрицает. Язык влажный, чистый. Кожные покровы бледно-розовые, чистые. Телосложение правильное, нормостеническое, индекс массы тела 26 кг/м2. Тоны сердца ясные, ритмичные, шумов нет. АД 117/78 мм рт. ст. (D=S). Пульс 74 уд. в мин. Дыхание везикулярное, частота дыхательных движений 15 в мин. Живот овоидной формы, увеличен за счет беременной матки, соответствующей 32 неделям беременности, мягкий, безболезненный при пальпации во всех отделах, участвует в акте дыхания. Симптомы раздражения брюшины – отрицательные. Селезенка и печень не увеличены. Симптом покалачивания отрицательный с обеих сторон. Молочные железы мягкие, безболезненные. Отеков нет. Периферические вены не расширены. Физиологические отправления в норме. Матка в нормотонусе, с четкими контурами, безболезненная при пальпации во всех отделах и при шевелениях плода. Окружность живота 86 см, высота дна матки – 31 см. Размеры таза в норме. Положение плода продольное, предлежание тазовое. Тоны плода ясные, ритмичные, 137–144 уд. в мин. По данным УЗИ: беременность по фетометрии 32 недели 1 день, тазовое предлежание плода; ультразвуковая допплерография – фето-плацентарный и маточно-плацентарный кровотоки в норме; цервикометрия – длина сомкнутой части цервикального канала 28 мм, внутренний зев закрыт; кардиотокография (КТГ) – нормальный тип кривой по критериям FIGO. Выполнены общий анализ крови (лейкоциты 15,3×109/л, эритроциты 4,26×1012/л, гематокрит 34,7%, тромбоциты 235×109/л, гемоглобин 121 г/л, нейтрофилы 81,2%, лимфоциты 9,9×109/л), коагулограмма (АЧТВ 24,3 сек., МНО 1,07, ПТИ 89,8%), общий анализ мочи (цвет соломенно-желтый, лейкоциты 1–3 (1/мкл), эпителий плоский 1–3 (1/мкл), белок – не обнаружен). Госпитализирована в отделение патологии беременности с предварительным диагнозом: «Беременность 32 недели. Тазовое предлежание плода. Угрожающие преждевременные роды. Хронический пиелонефрит, ремиссия. Миома матки. Наружный генитальный эндометриоз. Первичное бесплодие в течение 7 лет». Назначена токолитическая терапия (нифедипин по 20 мг перорально каждые 4 ч.), профилактика респираторного дистресс-синдрома плода (дексаметазон 8 мг внутримышечно № 3).
25.09.2022 в 14.00 ч. на обходе дежурного врача предъявляет жалобы на выраженные боли внизу живота, больше в правой подвздошной области, дискомфорт в правой поясничной области. Объективный статус и данные влагалищного исследования – без изменений. С целью дифференциальной диагностики с острой хирургической патологией (острый аппендицит, тромбоз сосудов таза, кишечная непроходимость, обострение хронического пиелонефрита, почечная колика) и исключения акушерской патологии (разрыв матки, преждевременная отслойка нормально расположенной плаценты) начат диагностический поиск. Выполнено по cito УЗИ органов брюшной полости (признаки диффузных изменений паренхимы печени, обнаружено незначительное количество свободной жидкости в брюшной полости по правому флангу межпетельно до 39 мм, по левому – 29 мм, в селезеночном углу – 16 мм, по ребрам матки отмечается расширение вен до 8 мм), почек (признаки хронического пиелонефрита); плацентография (данных за отслойку плаценты не выявлено), КТГ (нормальный тип кривой по критериям FIGO), общий анализ крови (лейкоциты 13,3×109/л, эритроциты 3,55×1012/л, гемоглобин 103 г/л, гематокрит 29,9%, нейтрофилы 71,1%), биохимический анализ крови (общий белок 65,1 г/л, СРБ 10,2 мг/л, общий билирубин 6,1 мкмоль/л, билирубин прямой 1,8 мкмоль/л, АСТ 12,3 Ед/л, АЛТ 16,8 Ед/л., креатинин 59,9 мкмоль/л, мочевая кислота 134,2 мкмоль/л, альфа-амилаза общая 46,1 Ед/л), общий анализ мочи (белок – отр., эпителий плоский 5–6–6 1/мкл), эпителий переходный 2–1 (1/мкл), лейкоциты 2–3 (1/мкл)). Проведена консультация хирурга: убедительных данных за острую хирургическую патологию нет. Принимая во внимание стабильную гемодинамику, отсутствие данных за хирургическую патологию на момент осмотра, рекомендовано: УЗИ органов брюшной полости с оценкой уровня свободной жидкости, контроль витальных функций, общих анализов крови и мочи через 2–4 ч с повторной консультацией хирурга, КТГ, спазмолитическая терапия. При ухудшении состояния беременной, нестабильной гемодинамике, изменении клинико-лабораторных показателей, нарастании объема свободной жидкости в брюшной полости – своевременно решить вопрос о диагностической лапаротомии, при экстренной акушерской ситуации – своевременно решить вопрос о родоразрешении путем операции кесарева сечения в неотложном порядке.
В 16.00 ч 25.09.2022 пациентка отмечает улучшение состояния на фоне стабильной гемодинамики, жалобы на боли внизу живота уменьшились. В 18:00 ч 25.09.2022 отмечает резкое усиление болей внизу живота, вызван хирург. По данным УЗИ в динамике: свободная жидкость в брюшной полости до 31 мм по левому флангу под селезенкой, в малом тазу за маткой 5 мм. В общем анализе крови – гемоглобин 92 г/л, лейкоциты 12,1×109/л, тромбоциты 219×109/л. По КТГ – нормальный тип кривой. Тошноты, рвоты, изжоги нет. Общее состояние средней степени тяжести. Сознание ясное. Кожные покровы бледно-розовые, чистые. Язык влажный, чистый. Температура тела 36,7°С. Тоны сердца ясные, АД 112/71 мм рт. ст. (D=S), Пульс 95 уд. в мин. Акроцианоза нет. Дыхание везикулярное, частота дыхательных движений 16 в мин. Отеков нет. Живот увеличен за счет беременной матки, не вздут, симметричный, мягкий при пальпации, участвует в акте дыхания, отмечается болезненность в правой подвздошной области. Симптомы раздражения брюшины – положительные. Перистальтика выслушивается, активная. Матка в нормотонусе, с четкими контурами, безболезненная при пальпации во всех отделах. Тоны плода приглушены, ритмичные, до 160 уд./мин. Шевеления плода ощущает хорошо. Симптом поколачивания отрицательный с обеих сторон. Мочеиспускание свободное, безболезненное. Диурез достаточный. Воды не отходили. Выделения из половых путей светлые, слизистые. Выставлен диагноз: «Беременность 32 недели. Тазовое предлежание плода. Внутрибрюшное кровотечение. Угрожающие преждевременные роды. Хронический пиелонефрит, ремиссия. Миома матки. Наружный генитальный эндометриоз. Первичное бесплодие в течение 7 лет». Принимая во внимание клинические и лабораторные данные, свидетельствующие о наличии внутрибрюшного кровотечения (снижение уровня гемоглобина со 121 до 92 г/л, по данным УЗИ – нарастание свободной жидкости в брюшной полости до 31 мм по левому флангу под селезенкой, в малом тазу за маткой 5 мм), выполнены – лапаротомия, кесарево сечение в нижнем сегменте матки, ревизия органов брюшной полости, дренирование малого таза. Обезболивание – эндотрахеальная анестезия.
Выполнена нижнесрединная лапаротомия. В брюшной полости обнаружено 970 мл жидкой крови со сгустками. Проведена реинфузия отмытых эритроцитов с применением аппарата Sell Saver. Матка увеличена до 32 недель беременности, серозный покров ее не изменен. Интраоперационный диагноз: Внутрибрюшное кровотечение. Операция кесарева сечения выполнена без осложнений. Извлечен плод мужского пола массой 2090 г, длиной 46 см, с оценкой по шкале Апгар 7–8–8 баллов, с признаками морфофункциональной незрелости. Совместно с хирургом произведена полная ревизия органов брюшной полости. Разрез на коже продлен с обходом пупка. По задней стенке матки определяются спайки, подпаян сальник и петли кишечника, справа и слева от матки имеются варикозно-расширенные вены, единичные эндометриоидные гетеротопии. Широкая связка матки справа имбибирована кровью, определяются узлы варикозно-расширенной вены, из которой подсачивает кровь – источник кровотечения. С целью гемостаза наложена гемостатическая губка. Кровотечение остановлено. Произведена эксцизионная биопсия ткани в области перфорации варикозно-расширенной вены. Травматических повреждений внутренних органов не выявлено, брюшная полость санирована, произведено дренирование малого таза через контрапертуру в правой подвздошной области. Контроль гемостаза – кровотечения нет. Моча по катетеру светлая, 150 мл. Общая кровопотеря составила 1470 мл (970 мл за счет интраабдоминального кровотечения, 500 мл – кесарево сечение). Проведены мероприятия по коррекции гиповолемии.
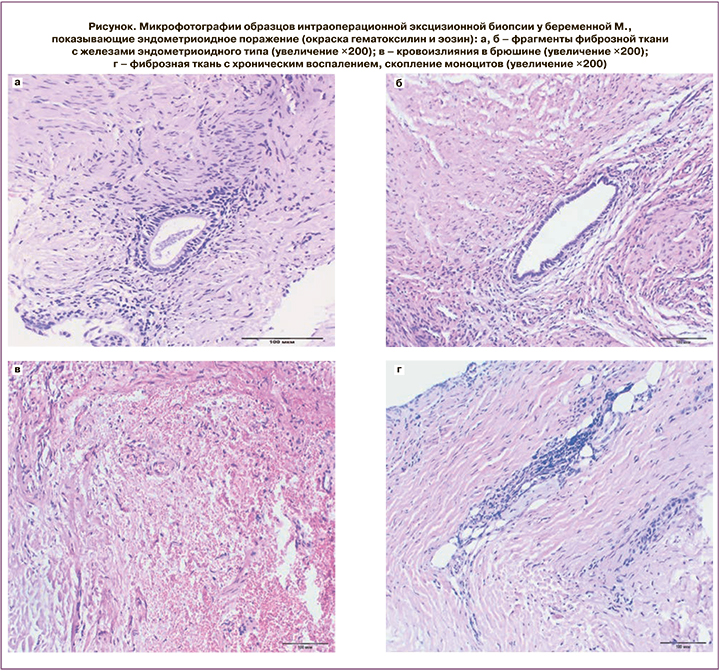
Гистопатологическое исследование образцов эксцизионной биопсии выявило эндометриоидное поражение (рисунок).
В послеоперационном периоде диагностирована постгеморрагическая анемия средней степени тяжести, в связи с чем, пациентка парентерально получала препараты железа. Дренаж удален на 3-и сутки.
Обсуждение
Клинический пример спонтанного интраабдоминального кровотечения в III триместре гестации вследствие активности ЭБ на фоне беременности демонстрирует стертость клинической симптоматики, обуславливает сложность диагностики и выбора тактики ведения пациентки с редким осложнением и отсутствием ясного понимания клиницистами проблемы «эндометриоз и беременность». Золотым стандартом для постановки диагноза остается визуальный осмотр (лапароскопия, лапаротомия) и гистопатологическое исследование биоптатов.
На современном этапе развития акушерства оказание ургентной медицинской помощи беременным предусматривает возможность проведения лапароскопической операции при наличии экстренных показаний на любом сроке беременности, включая III триместр. Однако, в клинической практике в данные сроки гестации лапароскопия применяется крайне редко из-за технических особенностей, связанных со сроком беременности и большими размерами матки. Данное наблюдение вносит свой вклад в подтверждение положения о том, что эндометриоз – это не локальный патологический процесс (у данной пациентки эндометриоидная киста яичника была удалена за 2 года до наступления беременности), а хроническая, прогрессирующая, рецидивирующая болезнь с индивидуальными особенностями течения во время беременности [18, 19]. По данным многолетних наблюдений [18], более чем у половины пациенток, рецидив эндометриоза после оперативного лечения наступает к концу 2-го года. Проблема эндометриоза сложна и многогранна, как с патофизиологической, так и с клинической точек зрения. И в системных обзорах литературы, наряду с акцентом на осложнения эмбрио- (фето-) плацентарного комплекса, указывается на возможность внутрибрюшного кровотечения в III триместре беременности [4, 15–17, 20]. Данный случай относится именно к этой категории клинических наблюдений, где эндометриоз является главным фактором реализации спонтанного гемоперитонеума; при этом клинико-морфологическая диагностика ЭБ имела место до наступления настоящей беременности. Известно, что в III триместре беременности происходит гормональная перестройка, эволюционно закрепленная необходимостью подготовки организма беременной к родам; при этом возможно изменение чувствительности эндометриоидных гетеротопий к изменяющемуся соотношению эстрогены/прогестерон и может сопровождаться отторжением высоковаскуляризированных очагов эндометриоидной ткани с геморрагиями, некрозом и последующей перфорацией рядом расположенных сосудов (в данном случае – перфорация сосудистой стенки варикознорасширенной маточной вены) и развитием спонтанного гемоперитонеума [9, 17, 18].
Можно предположить, что наступление спонтанной беременности и ее относительно благоприятное течение связано с хирургическим лечением эндометриомы яичника, что способствовало коррекции иммунного, провоспалительного, ангиогенного статусов, нормализации связей в системе «гипоталамус-гипофиз-яичники», рецептивности эндометрия, неосложненному течению периконцепционного этапа с формированием полноценной системы «мать-плацента-плод».
Дифференциальная диагностика болевого синдрома на фоне клинико- лабораторных данных воспалительного характера (лейкоциты 15,3×109/л, нейтрофилы 81,2%, СРБ 10,2 мг/л, положительный симптом раздражения брюшины), ассоциированного с активностью ЭБ и, в итоге, с развитием перфорации стенки варикозноизмененного сосуда, проводилась с острым аппендицитом, тромбозом вен таза, кишечной непроходимостью, обострением хронического пиелонефрита, почечной коликой, с такими акушерскими осложнениями, как разрыв матки, преждевременная отслойка нормально расположенной плаценты и угрожающие преждевременные роды. Необходимо учитывать сложность постановки диагноза, так как трудности диагностики связаны с низкой информативностью ультразвуковых методов в поиске источника кровотечения. Ведение пациентки потребовало междисциплинарного взаимодействия врачей акушеров-гинекологов, хирургов, терапевтов, анестезиологов-реаниматологов.
Заключение
Эндометриоз остается «болезнью загадок и предположений» не только в этиопатогенетическом плане, но и в рамках клинической проблемы «ЭБ и беременность». Сохраняет свою актуальность накопление знаний и опыта при ведении беременных женщин, страдающих данной патологией, в силу отсутствия четких критериев персонального влияния, как беременности на клинические проявления эндометриоза, так и ЭБ на течение гестации, что сопряжено с развитием жизнеугрожающих осложнений в виде интраабдоминального кровотечения, требующего своевременной активной акушерской и хирургической тактики с целью избежания критического акушерского состояния, материнской и перинатальной смертности.