Influence of nonablative radiofrequency on the expression of connective tissue proteins in the urogenital tract in patients with vaginal relaxation syndrome during the postpartum period
Objective. To determine the influence of radiofrequency (RF) on the mRNA expression of connective tissue proteins in the genital tract in patients with vaginal relaxation syndrome during the postpartum period.Dobrokhotova Yu.E., Nagieva T.S., Ilyina I.Yu., Kareva E.N., Kochina N.A., Zragus E.V., Dobrova A.B., Shakhmartova I.A., Krasnoshchok E.V.
Subjects and methods. Thirty patients who had undergone a cycle of radiofrequency vulvovaginal tightening according to the standard protocol took part in the study 2 months following childbirth. The results were assessed a month after the end of the cycle. The mRNA and protein expression of collagen genesis was analyzed by real-time PCR.
Results. During the treatment performed, the expression of decorin mRNA decreased by 9.7 times (p = 0.02), collagen type III by 6.2 times (p = 0.03), and matrix metalloproteinase type II by 1.3 times (p = 0.03).
Conclusion. Our findings confirm the influence of RF on the expression of genital tract connective tissue proteins in patients with pelvic floor dysfunction in the postpartum period.
Keywords
Decreased physiological tone of the vaginal walls, vaginal “laxity”, “relaxation” is a syndrome that attracts more and more attention of researchers, primarily due to the development of instrumental methods of intimate lifting. There is no standard definition for vaginal “laxity” [1]. Vaginal delivery can cause a decrease in sensitivity and sexual satisfaction during intercourse, vaginal gapping, air entering the vagina, which may be associated with objective changes in the structure and function of the pelvic floor in the postpartum period [2]. The etiological relationship between the vaginal delivery and vaginal “laxity” is not completely clear, however, a childbirth can lead to pelvic floor injuries, in particular, levator muscles, which may together contribute to vaginal overstretching and an increase in the length of the genital gap surrounded by interlocking bundles of puborectalis muscles [3, 4]. A number of authors isolate the overstretching of the introitus from genital prolapse, in which there is a displacement of the pelvic organs, provoking symptoms of pelvic floor dysfunction (PFD) [5]. Other researchers consider the loss of physiological tonus by the walls of the vagina as part of the manifestations of PFD [6]. If genitourinary disorders are characteristic of women during the menopausal period, vaginal relaxation syndrome is diagnosed in all age groups. The frequency of occurrence of vaginal „laxity”, according to the literature, varies widely, namely from 2% to 48% [7]. The issue of the true incidence of this state remains open [8]. Minimally invasive methods of treatment, including those based on local exposure to various types of energy, are gaining more and more popularity in the treatment of vaginal laxity symptoms and stress urinary incontinence. RF devices that emit high-frequency focused electromagnetic waves are used in medicine to generate thermal energy in the underlying layers of the vaginal walls connective tissue. Under the action of heat, protein denaturation occurs, the spirals of the collagen molecule are progressively reduced and the strength of fibrils increases; neocollagenogenesis is stimulated, activity of growth factors increases, tissue microcirculation improves [9-12]. A recent review of scientific publications on the correction of vaginal relaxation syndrome using various types of energy, demonstrates positive results that last from 4 weeks to 12 months [13]. However, the relationship between changes in the intensity of collagenogenesis in the connective tissue of the urogenital tract and clinical improvement in patients undergoing RF therapy remains controversial.
The aim of our study is to determine the effect of focused radiofrequency exposure on the mRNA expression of vaginal connective tissue proteins involved in collagenogenesis and neoangiogenesis in patients with vaginal relaxation syndrome in the postpartum period.
Materials and Methods
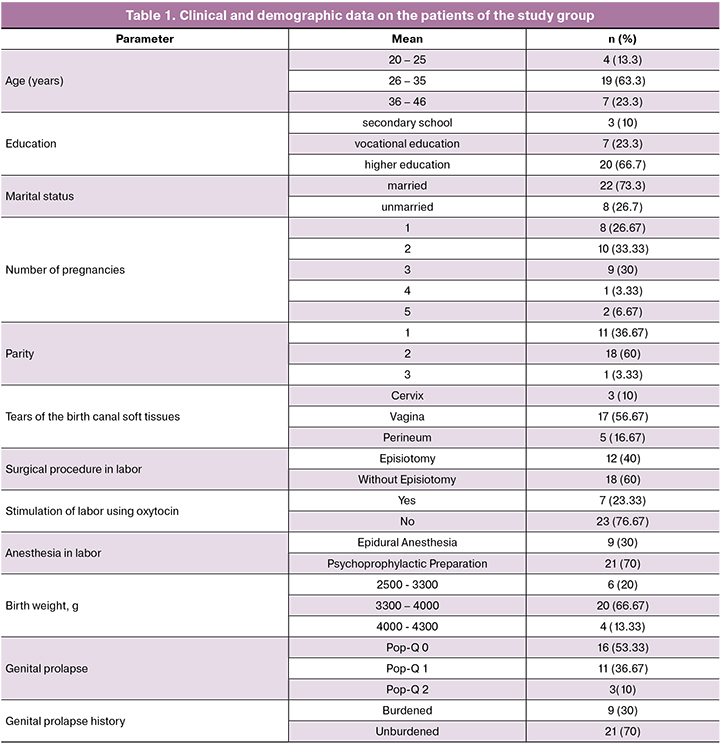
Thirty patients of reproductive age participated in the study. The average age of the patients was 31.69 (4.97) years. The study was conducted on the basis of Maternity Hospital №1 and the Department of Women’s Health at the Clinical Diagnostic Center MEDSI, Moscow. Inclusion criteria were the patient’s desire to participate in the study, the presence of PFD symptoms, persisting for two months after vaginal delivery. Exclusion criteria were pregnancy, genital prolapse (according to Pelvic Organ Prolapse Quantification System – POP-Q, stage III and higher), severe extragenital pathology, anomalies in the development of the genitourinary system, clinically significant gynecological diseases, a history of pelvic organs operations, acute inflammatory diseases of the pelvic organs and urogenital tract, oncological diseases, skin diseases in the active phase, sexually transmitted diseases. The basic information about the patients is presented in Table 1.
Research methods included analysis of complaints and medical history data, standard clinical and laboratory examination, gynecological examination, perineometry, real-time study of biopsy samples of the vaginal walls using polymerase chain reaction (PCR). Dynamic monitoring and evaluation of the results were carried out before the first procedure (two months after birth) and one month after the end of the therapeutic course.
Patients’ complaints about the foreign body sensation in the vagina, dragging pain in the lower abdomen, impaired urination related to stress urinary incontinence, the feeling of incomplete bladder emptying, dryness and discomfort during sexual intercourse, air entering the vagina during exercise and intercourse were interpreted by us as the symptoms of a vaginal relaxation syndrome. A standard clinical and laboratory examination involved an objective examination, a bimanual vaginal and abdominal examination; analysis of the results of colposcopy, cytological examination of smears from the vaginal portion of the cervix, smears on the flora, bacteriological examination of the vaginal discharge.
Patients underwent focused non-ablative radiofrequency (RF) exposure on the vulvar and vaginal tissues. Ten patients did not appear for follow-up examination one month after the end of the course of procedures, for reasons not related to the study. Questioning of these patients took place remotely (by phone). The method of RF exposure suggested a course of three procedures with an interval of seven days on an Exilis apparatus using Ultra Femme 360° technology (BTL, Czech Republic - Great Britain). The average duration of one procedure was 20 minutes. During the procedure, the patients were in the gynecological chair. Focused radio wave radiation with a frequency of up to 3 MHz was directed to the target tissue. Previously, a small amount of cooling gel was applied to the working zones. The technique included superficial (vulvar and perineal region) and intravaginal technique using tip-electrodes. The impact on the tissue was carried out by close contact of the tip with the surface of the treated areas. We followed the methodology described in the official manufacturer’s instructions, taking into account the specific technical parameters of the procedure.
The expression of matrix RNA (mRNA) of collagens type 1 and 3, vascular growth factor (VEGF), transforming growth factor (TGF-β), decorin, matrix metalloproteinases (MMP-2, MMP-9) and their tissue inhibitors (TIMP-1, TIMP-2) were evaluated using the PCR method. The specimen of the vaginal posterior wall with dimensions of about 0.3 x 0.3 cm was collected with scalpel (before and after the treatment). The sample was placed in an eppendorf tube with IntactRNA solution (EVROGEN) and stored at a temperature of –20 °С. Isolation of mRNA from vaginal tissue was performed using the AmpliPrim RIBO-prep kit in accordance with the manufacturer’s instructions. Obtaining cDNA on the mRNA matrix was carried out using the Revert-L reagent kit according to official instructions. A reagent kit for PCR „Reactive 2.5x reaction mixture for real-time PCR” in the presence of SYBR Green 1 was used on an iCycler iQ5 real-time PCR device (BioRad, Germany). The control gene was Gapdh, a housekeeping gene.
Statistical data processing and analysis of the results were performed using the Microsoft Excel tables, Statistica 7.0 software package. Distribution of normality of clinical and demographic parameters, introitus length, muscle contraction strength, mRNA expression values of collagenogenesis proteins, complaints associated with PFD were checked using the Kolmogorov-Smirnov test. In the normal distribution of data, parametric statistics methods were used.
In order to dynamically evaluate complaints associated with PFD, the McNamara test was used in patients before and after the treatment to compare the frequencies of qualitative binary signs in two dependent groups. To compare the results of perineometry, measuring the length of the introitus before and after the treatment with determining the level of statistical significance of the obtained data, we used the t-test for two dependent samples.
For distributions that differed from normal, we used methods of nonparametric statistics. An analysis of the PCR results for the statistical significance of the obtained differences in the expression of matrix proteins before and after the treatment was carried out using the Wilcoxon criterion. The expression of collagenogenesis proteins was evaluated by counting the number of copies of mRNA. We used the deltaCt method for the relative determination of the number of copies using the formula (1/2) ^ deltaCt, where deltaCt = Ct (of the studied gene) - Ct (GAPDH) and 2 ^ (- deltadeltaCt), where deltadeltaCt = deltaCt (sample of the vaginal wall obtained after RF exposure) - deltaCt (sample taken prior to initiation of therapy).
Results
During the course of the procedures, there were no cases of burns in the area of exposure, acyclic blood discharge from the genital tract, pain and/or discomfort. Subjective improvement was noted by 22 patients (73.3%). A decrease in the vaginal gapping one month after the end of the third RF lifting procedure was recorded in 14 patients (p = 0.07). The average length of the introitus before and after the treatment was 3.51 (0.53) cm and 3.40 (0.51) cm, respectively (p = 0.05).
An objective assessment of the state of the perineal muscles by perineometry showed an increase in the force of muscle contraction in patients after the treatment - 8.0 (2.32) mmHg, compared with the measurement recorded before the treatment - 5.47 (2.22) mmHg (p <0.001).
A dynamic assessment of patients’ complaints demonstrated a statistically significant relief of a number of symptoms of the relaxed vagina after the course of RF procedures (Table 2).
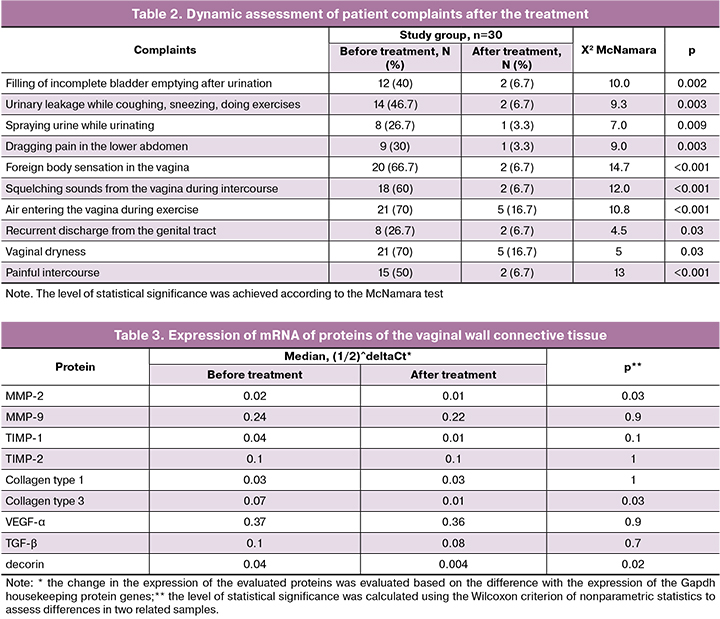
Table 3 shows the data on the changes in the mRNA expression of collagenogenesis and neoangiogenesis proteins in the obtained vaginal samples. As can be seen from the presented data, a statistically significant decrease in mRNA expression was observed only in relation to type 3 collagen, MMP - 2 and decorin.
Discussion
A thorough analysis of complaints two months after delivery and at the end of the rehabilitation program demonstrated the relief of a number of the PFD symptoms: a feeling of incomplete bladder emptying, spraying urine during urination, foreign body sensation in the vagina, „squelching sounds” during intercourse; vaginal dryness, pain and discomfort during intercourse, air entering the vagina during exercise. The improvement of the functional state of the levator muscles is indicated by the results of perineometry recorded one month after the third RF exposure procedure. These changes, as well as a decrease in the vaginal gapping in the patients, contribute to higher tightness of the vagina, the elimination of the vaginal laxity symptoms.
The study of mRNA expression of proteins involved in collagenogenesis using PCR revealed a statistically significant decrease in the expression of decorin, MMP-2 and collagen and type 3 mRNA, p <0.05. An increase in decorin mRNA expression is observed in patients with stress urinary incontinence and genital prolapse, which is confirmed by the literature [14]. An increase in the expression of decorin correlates with a decrease in the structural ordering of collagen and elastin fibrils. [15]. The decrease in the expression of this protein, recorded in our study, can determine the clinical improvement of the vulvovaginal area.
The expression of metalloproteinases mRNA increases with approaching labor and is maximal at the time of labor, which is necessary for enzymatic damage to the integrity of the fetal membranes. Subsequently, in the farther postpartum period, the expression of MMP-2 and MMP-9 progressively decreases to the initial level. A decrease in the expression of MMP-2 mRNA after our course of RF exposure may indicate the predominance of collagen synthesis processes over the decomposition reaction catalyzed by these metalloproteases [16]. MMP-9 exhibits a marked increase in expression in response to an inflammatory reaction. The anti-inflammatory therapeutic effect of RF exposure suggests a decrease in the expression of this protein in the studied patients. However, the absence of a statistically significant change in the expression of MMP-9 mRNA, along with TIMP-1 and TIMP-2, which we recorded, is probably due to the dynamic balance of the activation processes of metalloproteinases and their inhibitors in tissues.
In the connective tissue of the urogenital tract, collagen type 1 and 3 predominates. Type I collagen determines the mechanical strength of tissues, while type III collagen determines the elastic properties of tissues and their stretching [17]. Decreased expression of type III collagen mRNA determines an increase in the ratio of type I collagen to type III collagen, which is a prognostically favorable factor in reducing the risk of genital prolapse in patients with initial manifestations of PFD [18].
The literature provides conflicting data on the correlation between the symptoms of PFD and the expression of the collagen, mRNA, VEGF-α, TGF-β in the connective tissue of the urogenital tract [18-21]. In our study, there was no statistically significant change in the expression of VEGF-α mRNA that regulates the process of neoangiogenesis. The level of TGF-β mRNA expression, which plays a key role in the regulation of the intercellular matrix of connective tissue and its components by stimulating the biosynthesis of elastin protein by fibroblasts [22], also turned out to be relatively stable. Probably, a longer observation period is required to record changes in the mRNA expression of these proteins.
Changes in the mucous membrane of the vagina and vulvar tissues in the form of a lifting effect and improved tissue perfusion, in our opinion, can be associated with the thermal effect of RF procedures and the dosed mechanical effect of the working electrode. Dosed tissues overstretching and pressure exerted on them can affect the expression of matrix proteins and directly the synthetic activity of fibroblasts [14].
Clinical improvement in patients with PFD is an integral result of morphological and functional changes in the perineal tissue and vulvovaginal area. In our opinion, it is not advisable to associate such a positive effect entirely with the changes in the intensity of the collagen and other intercellular matrix proteins metabolism, in view of the dynamic balance and genetic determinism of the processes of decomposition and synthesis of connective tissue proteins. Features of biochemical processes that occur in a woman’s organism during pregnancy, childbirth and the postpartum period make it difficult to interpret our data on patients in the general population.
Conclusion
The number of patients significantly limits the statistical power of the results. But even at this stage it can be argued that focused RF exposure can affect the expression of matrix proteins in the connective tissue of the urogenital tract in patients with PFD in the postpartum period. It is necessary to continue the study of the expression of proteins metabolism in the connective tissue of the vulvovaginal region to determine their role in the clinical improvement of the pelvic floor, including the use of instrumental techniques on the basis of various types of energy. In our opinion, a search and study of new markers and research methods are required, with a longer observation period and an increase in the statistical power and quality of clinical trials.
References
- Pauls R.N., Fellner A.N., Davila G.W. Vaginal laxity: a poorly understood quality of life problem; a survey of physician members of the International Urogynecological Association (IUGA). Int. Urogynecol. J. 2012; 23(10): 1435-48.
- Thibault-Gagnon S., Yusuf S., Langer S., Wong V., Shek K., Dietz H. Do women notice the impact of childbirth-related levator trauma on pelvic floor and sexual function? Results of an observational ultrasound study. Int. Urogynecol. J. 2014; 25(10): 1389-98.
- Dietz H., Wilson P., Milsomc I. Maternal birth trauma: why should it matter to urogynaecologists? Curr. Opin. Obstet. Gynecol. 2016; 28(5): 441-8.
- Kamisan Atan I., Gerges B., Shek K., Dietz H.P. The association between vaginal childbirth and hiatal dimensions: a retrospective observational study in a tertiary urogynaecological centre. Br. J. Obstet. Gynaecol. 2015; 122(6): 867-72.
- Sekiguchi Y., Utsugisawa Y., Azekosi Y., Kinjo M., Song M., Kubota Y. et al. Laxity of the vaginal introitus after childbirth: nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfaction using low-energy radiofrequency thermal therapy. J. Womens Health (Larchmt). 2013; 22(9): 775-81. https://doi.org/10.1089/jwh.2012.4123.
- .Dietz H.P., Stankiewicz M., Atan I.K., Ferreira C.W., Socha M. Vaginal laxity: what does this symptom mean? Int. Urogynecol. J. 2018; 29(5): 723-8. https://doi.org/10.1007 / s00192-017-34260.
- Shobeiri S.A., Kerkhof M.H., Minassian V.A., Bazi T.; IUGA Research and Development Committee. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int. Urogynecol. J. 2019; 30(3): 371-6. https://doi.org/10.1007/s00192-018-3830-0.
- Rowen T.S. Editorial Comment on “Self-reported vaginal laxity-prevalence, impact, and associated symptoms in women attending a urogynecology cinic”. J. Sex. Med. 2018; 15(11): 1659-60.
- Leibaschoff G., Gonzales Izasa P., Cardona J.L., Miklos J.R., Moore R.D. Transcutaneous temperature controlled radiofrequency for the treatment of menopausal vaginal/genitourinary symptoms. Surg. Technol. Int. 2016; 29: 149-59.
- Alinsod R.M. Temperature controlled radiofrequency for vulvovaginal laxity. Prime. 2015; 3: 16-21.
- Millheiser L.S., Pauls R.N., Herbst S.J., Chen B.H. Radiofrequency treatment of vaginal laxity after vaginal delivery: nonsurgical vaginal tightening. J. Sex. Med. 2010; 7(9): 3088-95.
- Caruth J.C. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg. Technol. Int. 2018; 32: 145-9.
- Gold M., Andriessen A., Bader A., Alinsod R., French E.S., Guerette N. et al. Review and clinical experience exploring evidence, clinical efficacy, and safety regarding nonsurgical treatment of feminine rejuvenation. J. Cosmet. Dermatol. 2018; 17(3): 289-97. https://doi.org/10.1111/jocd.12524.
- Wang S., Lü D., Zhang Z., Jia X., Yang L. Effects of mechanical stretching on the morphology of extracellular polymers and the mRNA expression of collagens and small leucine-rich repeat proteoglycans in vaginal fibroblasts from women with pelvic organ prolapse. PLoS One. 2018; 13(4): e0193456. https://doi.org/10.1371/journal.pone.0193456. eCollection 2018.
- Nallasamy S., Yoshida K., Akins M., Myers K., Iozzo R., Mahendroo M. Steroid hormones are key modulators of tissue mechanical function via regulation of collagen and elastic fibers. Endocrinology. 2017; 158(4): 950-62. https://doi.org/10.1210/en.2016-1930.
- Rahajeng R. The increased of MMP-9 and MMP-2 with the decreased of TIMP-1 on the uterosacral ligament after childbirth. Pan. Afr. Med. J. 2018; 30: 283. https://doi.org/10.11604/pamj.2018.30.283.9905. eCollection 2018.
- Tinelli A., Malvasi A., Rahimi S., Negro R., Vergara D., Martignago R. et al. Age-related pelvic floor modifications and prolapse risk factors in postmenopausal women. Menopause. 2010; 17(1): 204-12.
- Gong R., Xia Z. Collagen changes in pelvic support tissues in women with pelvic organ prolapse. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019; 234: 185-9. https://doi.org/10.1016/j.ejogrb.2019.01.012.
- Rynkevic R., Martins P., Andre A., Parente M., Mascarenhas T., Almeida H., Fernandes A.A. The effect of consecutive pregnancies on the ovine pelvic soft tissues: Link between biomechanical and histological components. Ann. Anat. 2019; 222: 166-72. https://doi.org/10.1016/j.aanat.2018.12.002.
- Bhattarai A., Staat M. Modelling of soft connective tissues to investigate female pelvic floor dysfunctions. Comput. Math. Methods Med. 2018; 2018: 9518076. https://doi.org/10.1155/2018/9518076. eCollection 2018.
- Vetuschi A., Pompili S., Gallone A., D’Alfonso A., Carbone M.G., Carta G. et al. Immunolocalization of advanced glycation end products, mitogen activated protein kinases, and transforming growth factor-β/smads in pelvic organ prolapse. J. Histochem. Cytochem. 2018; 66(9): 673-86. https://doi.org/10.1369/0022155418772798.
- Liu C., Wang Y., Li B.S., Yang Q., Tang J.M., Min J. et al. Role of transforming growth factor β1 in the pathogenesis of pelvic organ prolapse: A potential therapeutic target. Int. J. Mol. Med. 2017; 40(2): 347-56. https://doi.org/10.3892/ijmm.2017.3042.
Received 08.04.2019
Accepted 19.04.2019
About the Authors
Dobrokhotova Yulia E., MD, professor, Head of the Department of Obstetrics and Gynecology of the medical faculty Pirogov Russian National Research Medical University.117997, Russian Federation, Moscow, Ostrovityanova str., 1.
Nagieva Tamara S.K., postgraduate student of the Department of the Obstetrics and Gynecology of the medical faculty Pirogov Russian National Research Medical University.
117997, Russian Federation, Moscow, Ostrovityanova str., 1.
Il’ina Irina Yu., MD, Associate Professor of the Department of Obstetrics and Gynecology of the medical faculty Pirogov Russian National Research Medical University.
117997, Russian Federation, Moscow, Ostrovityanova str., 1.
Kareva Elena N., MD, professor of the Department of Molecular Pharmacology Pirogov Russian National Research Medical University.
117997, Russian Federation, Moscow, Ostrovityanova str., 1.
Kochina Nataliya A., Ph.D, Senior Researcher of the Research Laboratory of Molecular Pharmacology Pirogov Russian National Research Medical University.
117997, Russian Federation, Moscow, Ostrovityanova str., 1.
Zraguz Elena V., obstetrician-gynecologist of the highest category, the head of the 2nd obstetric physiology department Maternity Home number 1.
125480 Russian Federation, Moscow, Vilis Lacis str., 4.
Dobrova Anna B., obstetrician-gynecologist of the first category, the Head of the maternity home branch Maternity Home number 1.
125480 Russian Federation, Moscow, Vilis Lacis str., 4.
Shakhmartova Irina A., the doctor of the highest category, obstetrician-gynecologist, Head of the Women’s Health Department Clinical Diagnostic Center «MEDSI-2».
123242, Russian Federation, Moscow, Krasnaya Presnya str., 16.
Krasnoschok Ekaterina V., the student of the Pirogov Russian National Research Medical University.117997, Russian Federation, Moscow, Ostrovityanova str., 1.
For citation: Dobrokhotova Yu.E., Nagieva T.S., Ilyina I.Yu., Kareva E.N., Kochina N.A.,
Zragus E.V., Dobrova A.B., Shakhmaratova I.A. Krasnoshchok E.V. The effect of radiofrequency non-ablative effects on the expression of connective tissue proteins of the urogenital tract in patients with relaxed vagina syndrome in the postpartum period.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (8): 119-25 (in Russian)
http://dx.doi.org/10.18565/aig.2019.8.119-125