Impact of obesity and excessive gestational weight gain on birth outcomes
Khodzhaeva Z.S., Tmoshina I.V., Degtyareva E.I., Snetkova N.V., Potapova A.A.
Background. Fat metabolism disorders in reproductive-aged women are becoming a pandemic and are one of the most important causes of maternal and perinatal morbidity and mortality. In addition, clarifying the contribution of gestational weight gain to birth outcomes will also promote the optimization of obstetric tactics. Material and methods. A total of 179 pregnant women were examined and delivered, divided into 4 groups and subgroups according to initial body weight and normal/excessive gestational weight gain. The data obtained were entered into the Microsoft Excel database. The results were statistically processed using the IBM SPSS Statistics 22 software package. Results. The most vulnerable group of patients with premorbid obesity (group III) was identified in terms of intranatal and neonatal complications. The same group was noted to have the highest incidence of delivery complications and birth trauma, which requires that the obstetric tactics should be revised to more actively manage the labor process. Conclusion. The findings require the elaboration of differentiated approaches to managing childbirth depending on the degree of obesity and gestational weight gain, which will improve obstetric care quality and obstetric and perinatal indicators.
Keywords
Abnormalities in fat metabolism among women of reproductive age have the nature of a pandemic, they are one of the most important causes of maternal and perinatal morbidity and mortality, and therefore, it is an acute problem of modern obstetrics, which requires a reassessment of existing traditional medical approaches [1, 2]. The role of gestational weight gain among women, depending on the initial body weight in the development of complications of pregnancy, childbirth and the postpartum period, requires a detailed research.
The purpose of this research is to study the effect of obesity and excessive gestational weight gain on labor outcomes.
Materials and Methods
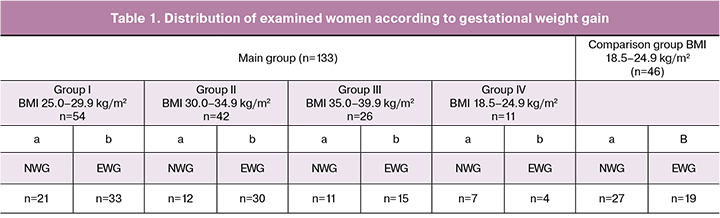
During the research, a total of 179 pregnant women were examined and delivered. The main group included 133 pregnant women, the body mass index (BMI) of whom was 25 kg / m2 and more by the time of pregnancy. There were 46 pregnant women with a body mass index BMI (18.5-24.9 kg/m2) in the comparison group. The pregnant women of the main group were divided into 4 groups according to BMI: group I – overweight (BMI 25-29.9 kg/m2, n=54), group II - I degree obesity (BMI 30-34.9 kg/m2, n=42), group III - II degree obesity (BMI 35-39.9 kg/m2, n=26), group IV - III degree obesity (BMI 40 kg/m2 and more, n=11).
The inclusion criteria were baseline excess body weight or degree I to III obesity for the main group, normal BMI for the comparison group, term pregnancy (gestational age 37-41 weeks), age 20-40 years, informed consent for participation in the research, local ethical committee authorization.
Exclusion criteria were endocrine diseases, including diabetes mellitus, severe extra genital pathology, multiple pregnancies and pregnancy as a result of IVF.
Anamnestic, anthropometric, obstetric and laboratory methods were used in the research.
In order to study the effect of weight gain on the outcome of labor, all the pregnant women within their groups were divided into two subgroups: with normal weight gain (NWG) and excessive weight gain (EWG) (Table 1).
The obtained data were entered into the Microsoft Excel database. All statistical procedureswere performed using IBM SPSS Statistics 22 software package.
Results
The number of primiparous women was the largest in group I (n=22, 40.7%), and multiparous women prevailed in the comparison group (n=35, 76.1%), group II (n=33, 76.7%) and group IV (n=8, 72.7%). At the same time, the differences were not statistically significant. The majority of first-time mothers were in the comparison group (65.2%), group I (64.8%) and group IV (63.6%). The number of patients with repeated deliveries was higher in group II, (n=25, 58.1%). The differences were statistically significant (p<0.05).
The outcome analysis of previous pregnancies revealed the highest incidence of abortions (n=6) among women in group IV (54.5%); the termination of the previous pregnancy was carried out at 16-20 weeks due to multiple malformations in the fetus in 27.3% of cases. One patient of this group had antenatal fetal death at 34 weeks gestation in her obstetric history. The differences were statistically significant (p<0.05).
The number of miscarriages in the obstetric history was 4 (8.6%) in the comparison group and it was 5 (9.3%), 10 (23.3%), 4 (16%) and 1 (9.1%) in groups I, II, III and IV, respectively. It should be noted that the highest frequency of miscarriages was observed in group II, among patients with I degree obesity (p<0.05).
Three patients from the comparison group had non-developing pregnancy in the obstetric history (6.5%), whereas non-developing pregnancy was observed in patients with fat metabolism disorder from groups I, II, III and IV in 9 (16.7%), 6 (14), 4 (16%) and 2 (18.2%) cases, respectively. The differences were statistically insignificant.
Taking into consideration the important prognostic influence of the initial state of the cervix on the course and outcome of labor, we evaluated the maturity of the cervix according to the Bishop score. Thus, the mature cervix of the uterus was statistically more common among pregnant women of all the groups with NWG and only in 5-7% in groups I and II with EWG. Immature cervix of the uterus was observed in the majority of pregnant women with EWG in all the groups of patients with fat metabolism disorders (p<0.01) (Table 2).
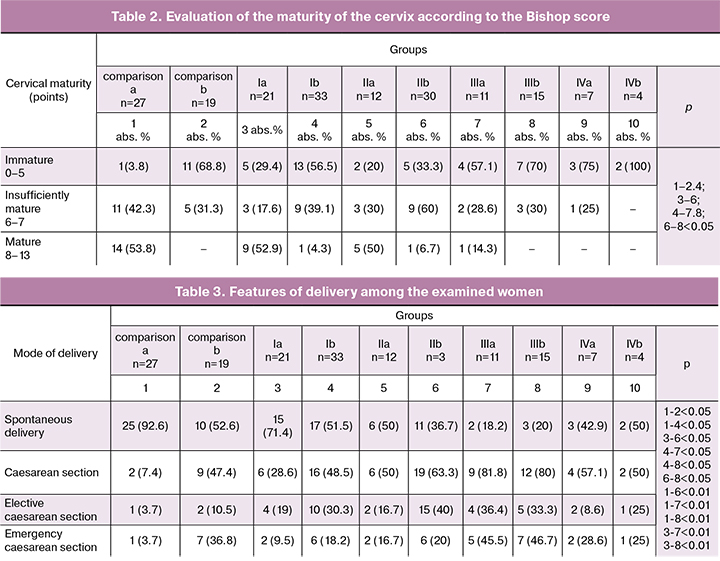
According to Table 2, the unripe cervix of the uterus was observed only in one patient from the comparison group with NWG (3.8%), whereas in all pregnant women from group IVb the cervix was estimated as immature. When comparing subgroups of each group with NWG and EWG during pregnancy, significant intra-group differences were noted: there were less patients with «mature» birth canals in the subgroups b, however there were more pregnant women with «immature» and «insufficiently mature» birth canals (p< 0.05).
The rate of induction was significantly higher in all subgroups with EWG. In the comparison subgroups it was 3.7% for NWG and 15.8% for EWG, in group I - 4.8% and 21.2%; in group II - 8.3% and 26.6%, in group III - 9.1% and 33.3%; in group IV - 14.3% and 25%, respectively. The most frequent induction was in group III with II degree obesity with EWG, it was 33.3% (p<0, 05).
Failure to progress in labour was observed in all subgroups with EWG except group III: in the comparison group it was 3% with NWG and 26% with EWG, in group I it was 3% and 14%, in group II it was 3% and 18%, in group IV it was 14% and 25%, respectively (p<0.05). It is worth noting that in group III the frequency of failure to progress in labour did not depend on gestational weight gain (18% and 21%, respectively) and developed with the cervix dilation to 5 cm. In addition, in groups III and IV with EWG the failure to progress in labour developed during epidural anesthesia and it was not the subject of medical correction (26.7% and 25%, respectively). When the cervix was dilated more than 5 cm, the failure to progress in labour was often observed in case of EWG, in the comparison group, in groups I and II.
All cases of failure to progress in labour were observed in patients from groups III and IV when the cervix was not dilated to 4 cm. Analyzing the features of the appearance of late failure to progress in labour, attention was drawn to the fact that most frequently (16% of cases), it occurred in the subgroup with EWG of the comparison group (p<0.05). The conducted correlation analysis showed that there is a strong connection between the insufficient maturity of the birth canal and the early onset of failure to progress in labour (p<0.05).
The frequency of delivery through the natural birth canal for subgroups with NWG of the comparison group and group I was 92.6% and 71.4%, respectively. In subgroups with EWG of the same groups the incidence of spontaneous delivery was statistically significantly lower: 52.6% and 51.5%, respectively (p<0.05) (Table 3).
Emergency caesarean section was the predominant mode of delivery in patients with EWG. Thus, the frequency of emergency caesarean section within this group was 10 times higher up to 36.8% among patients with EWG compared to the women with NWG (3.7%, p<0,01). The same situation was observed in the patients with excessive weight (group I). The frequency of emergency cesarean section among women with EWG of this group was twice greater than in the subgroup with NWG (18.2% and 9.5%, respectively, p<0.05); in group II with I degree obesity the indices were 33% and 50%, respectively (p<0.05). Only in group III with II degree obesity the frequency of emergency caesarean section did not depend on gestational weight gain and was 45% and 47%, respectively. In group IV all the cases of abdominal delivery were performed according to the plan.
The clinically narrow pelvis in all the groups complicated the birth process only in patients with EWG with a frequency of 16%, even in the comparison group and reached its maximum value of 28.6% in subgroup IVa.
Intra-group analysis of newborns body weight in the subgroups of the main groups showed significant differences: children in the subgroups of all the groups with fat metabolism disorders and EWG during pregnancy were significantly higher than in the subgroups of the same groups with NWG: group Ia - 3327.7 ± 382.5 g, Ib - 3634.2 ± 470.3 g (p<0.05); in group IIa — 3390.5 ± 417.8 g, in group IIb - 3582.5 ± 414.9 g (p<0.05); in group IIIa - 3391.9 ± 487.9 g, IIIb - 3670.4 ± 664.3 g (p<0.05); in group IVa - 3644.3 ± 478.6 g, IVb - 3906.3 ± 290.7 g (p<0.05).
According to the analysis of the growth rates of newborns, significant differences were found between the subgroup IVb in which the length of the newborn was the largest - 53.3 ± 1.7 cm and the comparison subgroups a and b, Ia and IIa, which differed statistically significantly from this parameter ( p<0.05).
Assessment of newborns according to the Apgar score at 5 minutes was statistically significantly different between the subgroups of the comparison group: a (8.9 ± 0.3 points) and b (8.1 ± 1.6 points), p<0.01. Thus, EWG during pregnancy in patients with initially normal body weight influences the state of the newborn most significantly..
Birth trauma was not observed in the subgroup a of the comparison group, groups Ia, IIa; the frequency was more in the subgroup IVa – 28.6% (p<0.01). It should be noted that in the comparison group, groups I and II, birth injuries were observed only in newborn subgroups with EWG during pregnancy and in groups III and IV the birth trauma did not correlate to the birth weight increase: in the comparison group b – 5.3%, in group Ib - 6%, IIb – 3.3%, IIIа – 9.1%, IIIb – 6.7%, р<0.05.
In studying birth traumas structure it was observed that the most common injury was the Cephalohematoma. It was diagnosed in women of the comparison group, groups I, III and IV. Fracture of the collarbone was diagnosed in two cases in groups I and II. In addition, in group III there was a hemorrhage in the adrenal glands (one case) and in group IV there was an injury of the brachial plexus, which caused Erba paralysis (one case).
The uncomplicated course of the postpartum period occurred in 70.7% of patients in the subgroup a of the comparison group and in 68.4% of patients in the subgroup b of the comparison; in 42.9% of cases in subgroup Ia and in 72.7% in subgroup Ib, 58.3% in subgroup IIa and 76.7% in subgroup IIb, in 36.4% in subgroup IIIa and in 40% in subgroup IIIb, in 28.6% in subgroup IVa and in 50% in subgroup IVb. The difference in subgroups was statistically significant (p<0.05).
Analysis of the lactation function showed the dependence of its normal development on the increase in body weight. The normal development of lactation was statistically more frequent in women with NWG in group Ia – 76.2%, Ib – 60.6% and group IIa – 66.7%, IIb - 50% (р<0.05).
Lochiometer complicated the course of the postpartum period in all subgroups, with the exception of the comparison subgroup a and group IIa. It was statistically significantly more frequent in group IV, subgroup with EWG - 25%.
Sub-involution of the uterus was diagnosted in the subgroup Ib (3%), IIb (3.3%), IIIa (9.1%), IIIb (6.7%), IVa (14.3%), IVb (25%). This complication occurred only in subgroups with EWG during pregnancy of women with EWG and I degree obesity and in patients with II and III degree obesity, there was no dependence on weight gain (p<0.05).
Endometritis was not observed in patients of the comparison subgroups Ia and IIa. Its frequency was in the subgroup Ib - 3%, IIb – 6.6%, IIIа – 9.1%, IIIb – 13.4%, IVа – 14.3%, IVb - 25%. According to this research the frequency of endometritis tends to increase with an increase in the initial weight gain and EWG and which was particularly demonstrative for group IV.
In addition, a significant impact of EWG is noted in the occurrence of the lochiometers, endometritis and sub-unvolution of the uterus in comparison groups and group I. This complication occurred only in groups with EWG (p<0.05). But in groups with initial obesity (II, III, IV) there was no significant effect of weight gain on the incidence of these complications.
Conclusion
Gestational EWG affects all stages of the birth process, even with initially normal weight gain, beginning with the immaturity of the birth canal by the end of the full term of pregnancy, the inadequate efficiency of induction, which was the trigger in the development of the early primary WLA (most often in groups with II and III degrees obesity). Thus, in subgroups with EWG of all groups, in most cases «immature» and «insufficiently mature» birth canals were observed (p<0.05). In addition, among the patients who were delivered by caesarean section the rate of immaturity of the birth canal was significantly higher in all subgroups. The results of our research revealed the most vulnerable group of patients with premorbid obesity (group III) in terms of intranatal complications. In the same group the highest frequency of complications in childbirth and birth injury was noted, which requires a revision of obstetric tactics in favor of more active management of the birth process. According to our research, it is required to develop different approaches to the management of childbirth, depending on both the degree of disturbance of fat metabolism and the nature of gestational weight gain, which will improve the quality of obstetric care and improve obstetric and perinatal indicators.
References
- Fuchs F., Senat M.V., Rey E., Balayla J., Chaillet N., Bouyer J., Audibert F. Impact of maternal obesity on the incidence of pregnancy complications in France and Canada. Sci. Rep. 2017; 7(1): 10859.
- Vinturache A., McKeating A., Daly N., Sheehan S., Turner M. Maternal body mass index and the prevalence of spontaneous and elective preterm deliveries in an Irish obstetric population: a retrospective cohort study. BMJ Open. 2017; 7(10): e015258.
- Mitchell A.M., Porter K., Christian L.M. Examination of the role of obesity in the association between childhood trauma and inflammation during pregnancy. Health Psychol. 2018; 37(2): 114-24.
- Nagl M., Steinig J., Klinitzke G., Stepan H., Kersting A. Childhood maltreatment and pre-pregnancy obesity: a comparison of obese, overweight, and normal weight pregnant women. Arch. Womens Ment. Health. 2016; 19(2): 355-65.
- Cosson E., Cussac-Pillegand C., Benbara A., Pharisien I., Nguyen M.T., Chiheb S. et al. Pregnancy adverse outcomes related to pregravid body mass index and gestational weight gain, according to the presence or not of gestational diabetes mellitus: A retrospective observational study. Diabetes Metab. 2016; 42(1): 38-46.
- Barquiel B., Herranz L., Meneses D., Moreno Ó., Hillman N., Burgos M.Á., Bartha J.L. Optimal gestational weight gain for women with gestational diabetes and morbid obesity. Matern. Child Health J. 2018;22(9): 1297-305.
Received 05.03.2018
Accepted 20.04.2018
About the Authors
Khodzhaeva, Zulfiya S., M.D., Ph.D., Professor, Head of High Risk Pregnancy Department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: zkhodjaeva@mail.ruTimoshina, Irina V., Ph.D., Researcher of High Risk Pregnancy Department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: i_timoshina@oparina4.ru
Degtyareva, Elena I., Ph.D., Researcher of High Risk Pregnancy Department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: e_degtyareva@oparina4.ru
Snetkova, Nina K., the postgraduate student of High Risk Pregnancy Department, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: n_snetkova@oparina4.ru
Potapova, Alyona A., clinical resident, National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov,
Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: Alyona.5_5_4__Zd@mail.ru 8 960 574 66 44
For citations: Khodzhaeva Z.S., Tmoshina I.V., Degtyareva E.I., Snetkova N.V., Potapova A.A. Impact of obesity and excessive gestational weight gain on birth outcomes. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (9): 62-6. (in Russian)
https://dx.doi.org/10.18565/aig.2018.9.62-66