Проблема современного мира – ожирение – является неинфекционной эпидемией. Лиц с избыточной массой тела и ожирением в мире уже больше, чем людей с недостатком веса. Треть населения Земли имеют избыточную массу тела, больше половины из них – женщины. Алиментарно-конституциональное ожирение – полиэтиологичное заболевание. К явным причинам, его вызывающим, относят поступление избытка калорий с пищей (за счет простых углеводов и жиров), недостаточное употребление чистой воды, нарушение режима питания, дефицит физической активности, нарушение сна, замедление метаболизма с возрастом, дисбаланс витаминов и микроэлементов. Поколение 1990-х гг. входит в репродуктивный возраст, молодые люди привыкли к питанию с преобладанием в рационе полуфабрикатов, консервов и сублимированных продуктов, что плохо насыщает, провоцирует есть больше; как результат, происходит накопление жира в организме. Ожирение достоверно снижает репродуктивный потенциал женщин и мужчин [1–3]. Известно, что при ожирении существует прямая зависимость между увеличением массы тела и тяжестью овариальных нарушений, сопровождающихся ановуляцией, неполноценностью лютеиновой фазы и снижением фертильности [4, 5]. Риск развития невынашивания, преэклампсии и гипертензионных расстройств, патологии плаценты, гестационного сахарного диабета у беременных с ожирением выше, чем в популяции. Важно, чтобы все специалисты здравоохранения проводили разъяснительную работу и конкретные мероприятия, направленные на снижение распространенности ожирения. Остро встает вопрос проведения прегравидарной подготовки женщин с ожирением с учетом патогенетических особенностей формирования болезни.
Цель исследования – определить эффективность комплексной программы прегравидарной подготовки на основании изучения особенностей течения беременности у женщин с ожирением.
Материалы и методы
Научная работа проводилась в клинике ФГБОУ ВО «Пермский государственный медицинский университет им. академика Е.А. Вагнера» Минздрава России, Городском перинатальном центре «Городской больницы им. М.А. Тверье». Обследовано 118 женщин репродуктивного возраста, постоянно проживающих в г. Перми (табл. 1). Всем женщинам проводилась оценка антропометрических данных, определялся индекс массы тела (ИМТ), который рассчитывали как отношение веса (кг) к росту (м) в квадрате, рассчитывался коэффициент К (отношение окружности талии (ОТ) в сантиметрах к окружности бедер (ОБ) в сантиметрах). При К менее 0,8 выставлялся гиноидный тип ожирения, при К более 0,8 – диагноз андроидного (висцеро-абдоминального) типа ожирения.
Критерии включения в исследование для женщин основной и групп сравнения: андроидный (висцерально-абдоминальный) тип ожирения (К более 0,8), ИМТ от 30 до 45 кг/м2, отсутствие острого инфекционного процесса, отсутствие противопоказаний для назначения медикаментозной терапии ожирения.
Критериями исключения для пациенток основной группы и группы сравнения были: содержание гемоглобина в крови менее 110 г/л и/или наличие у пациентки клинических проявлений железодефицитной анемии, экстрагенитальная патология в стадии декомпенсации, тиреотоксикоз, противопоказания к назначению препарата «Редуксин Форте» (в соответствии с инструкцией по применению препарата), отказ от участия в исследовании. В течение 1 месяца 4 пациентки из основной группы отказались от участия в связи со сменой места жительства и по семейным обстоятельствам.
Критериями включения в контрольную группу пациенток были: нормальная масса тела (ИМТ от 20 до 25 кг/м2), отсутствие экстрагенитальной патологии или компенсация хронического состояния, отсутствие инфекционного процесса любой локализации.
Разработана программа прегравидарной подготовки, которую применяли пациенткам основной группы.
Консультации по питанию проводились врачом-диетологом в групповом режиме в рамках «Школы правильного питания».
Консультации врача лечебной физкультуры и спортивной медицины проводились в групповом режиме с рекомендациями по оптимальному режиму физической нагрузки (не менее 10 000 шагов в сутки, не менее 30 минут в день аэробной нагрузки), с учетом лишнего веса.
Рекомендации по питьевому режиму: 1500,0 мл чистой воды в сутки.
Консультации врача акушера-гинеколога с назначением следующих витаминов и микроэлементов: холекальциферола 1500 МЕ в сутки, фолиевой кислоты 1000 мкг в сутки, препаратов йода 150 мкг в сутки.
Проводилась медикаментозная терапия ожирения комплексным препаратом сибутрамин+метформин однократно утром (препарат «Редуксин Форте») в течение 3 месяцев с одновременным назначением контрацептивных препаратов.
При определении низкого содержания ферритина (менее 20 мкг/мл) назначались препараты железа 100 мкг в сутки в течение 2 месяцев.
Женщин наблюдали на фоне данной программы в течение 6 месяцев, фиксировали все нежелательные явления: время возникновения, тяжесть, корреляция с лечением, исходы.
Всем женщинам основной группы определяли содержание 25-гидроксихолекальциферола (25-(OH)-D) в сыворотке крови иммуноэлектрохемилюминесцентным методом (CMIA) на анализаторе Abbott Architect 2000. За нормальный уровень насыщения принимали содержание 25-(OH)-D от 32 до 50 нг/мл, при его содержании от 31 до 20 нг/мл определяли недостаток, ниже 20 нг/мл – дефицит [6]. Уровень сывороточного ферритина определяли на автоматическом анализаторе Alisei Q. S. (SEAC, Италия) методом твердофазного иммуноферментного анализа.
Исследование одобрено решением этического комитета Пермского государственного медицинского университета №2 от 27.02.2017.
Получено информированное согласие каждой женщины, участвующей в исследовании.
Результаты и обсуждение
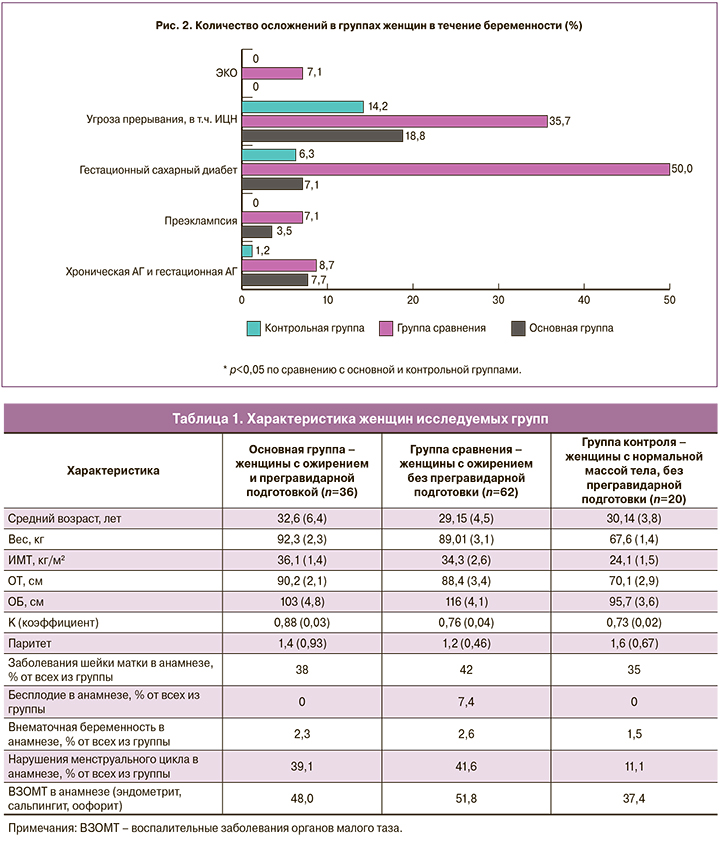
 Все пациентки основной группы и группы сравнения имели висцеро-абдоминальное распределение жира (100%). Этот жир располагается внутри брюшной полости, имеет большее количество жировых клеток на единицу массы ткани, большую плотность адренорецепторов, рецепторов к глюкокортикоидам и андрогенам. Пациентки с ожирением в анамнезе имели нарушения менструального цикла в 3,5 раза чаще, чем женщины с нормальной массой тела (табл. 1). Встречаемость хронических воспалительных заболеваний органов малого таза и заболеваний шейки матки не отличалась в группах. Первичное бесплодие выявлено только в группе сравнения (табл. 1).
Все пациентки основной группы и группы сравнения имели висцеро-абдоминальное распределение жира (100%). Этот жир располагается внутри брюшной полости, имеет большее количество жировых клеток на единицу массы ткани, большую плотность адренорецепторов, рецепторов к глюкокортикоидам и андрогенам. Пациентки с ожирением в анамнезе имели нарушения менструального цикла в 3,5 раза чаще, чем женщины с нормальной массой тела (табл. 1). Встречаемость хронических воспалительных заболеваний органов малого таза и заболеваний шейки матки не отличалась в группах. Первичное бесплодие выявлено только в группе сравнения (табл. 1).
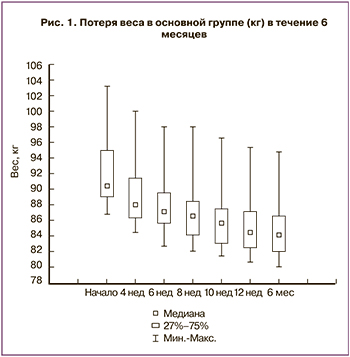
Через 3 месяца снижение массы тела произошло у всех пациенток основной группы во время прегравидарной подготовки (рис. 1). Средняя потеря веса составила 7,52 кг (min – 3,5 кг; max – 11,8 кг). Потеря общего веса пациенток основной группы составила 8,3% от первоначального общего веса. Окружность талии уменьшилась в среднем на 8,4 (3,9) см. Известно, что снижение массы тела за счет жировой ткани способствует улучшению показателей метаболизма, повышается чувствительность тканей к инсулину [7]. На фоне медикаментозной коррекции веса нежелательных явлений у пациенток не выявлено. Однако отмечены кратковременные побочные эффекты через 2 дня после приема препаратов у 6/36 (16,5%) пациенток в виде сухости во рту, которая нивелировалась самостоятельно к концу первой недели приема препарата при соблюдении питьевого режима (2000 мл в сутки). Других побочных явлений не обнаружено.
Через полгода наблюдения из основной группы забеременели 26/36 (81%) женщин, остальные 6/36 (19%) отказались от участия в исследовании по объективным для них причинам (отказ от репродуктивных планов, использование контрацептивных средств). В группе сравнения самостоятельно забеременели 32/62 (51,6%) женщины, а 2/62 (3,2%) женщины отказались от участия в исследовании. В группе сравнения 14/62 (8,7%) женщин имели самопроизвольное прерывание беременности на раннем сроке, 4/62 (2,5%) пациенток – неразвивающуюся беременность. В группе пациенток с прегравидарной подготовкой случаев потерь беременности не выявлено. Из литературы известно, что окислительный стресс на фоне ожирения способен индуцировать эндотелиальную дисфункцию, а недостаточная децидуализация стромы эндометрия способствует неполной или слабой инвазии цитотрофобласта. Как следствие, эти изменения могут приводить к гибели эмбриона, отслойке трофобласта [8].
В группе сравнения 4/62 (6,5%) женщины с ожирением без прегравидарной подготовки забеременели благодаря экстракорпоральному оплодотворению (ЭКО), имея диагноз «бесплодие» (рис. 2). Причинами бесплодия послужили: трубный фактор – 3/62 (4,8%) и мужской фактор – 1/62 (1,6%).
Ожирение во время беременности приводит к нарушению синтеза и функции цитокинов в жировой ткани. В условиях сопутствующего субклинического воспаления и оксидативного стресса происходят дальнейшие нарушения функции адипоцитов и макрофагов жировой ткани, а также выработка провоспалительных цитокинов, что приводит к формированию процессов эндотелиальной дисфункции. Нами установлено, что у пациенток без прегравидарной подготовки течение беременности чаще осложнялось патологическими состояниями (рис. 2). Угроза невынашивания беременности развилась у 10/32 (34,4%) женщин, в том числе с формированием истмико-цервикальной недостаточности. Этот показатель оказался выше в 2 раза, чем в группе женщин с программой прегравидарной подготовки – 7/36 (19,4%).
Дизрегуляция продукции гормонов жировой ткани вызывает нарушение функции ß-клеток поджелудочной железы, инсулиновых рецепторов, что обусловливает развитие инсулинорезистентности [9, 10]. В группе сравнения (женщины без прегравидарной подготовки) в течение беременности развился гестационный сахарный диабет у 16/32 (50%) женщин, и только у 4/36 (11,1%) – в основной группе. Гипертензионные расстройства при беременности в группах женщин с ожирением встречались примерно с одинаковой частотой, а у женщин с нормальной массой тела выявлен единичный случай (рис. 2).
При изучении осложнений беременности, связанных с фетоплацентарным комплексом, оказалось, что во всех группах преобладали плацентарные нарушения (рис. 3). Данные осложнения встречались у 8/36 (22,2%) пациенток после проведенной прегравидарной подготовки и у 20/32 (62,6%) без подготовки к беременности. Следует отметить, что в группе женщин без ожирения также выявлены нарушения фетоплацентарного кровотока, в частности, преждевременное созревание плаценты диагностировано у 3/20 (15%) женщин.
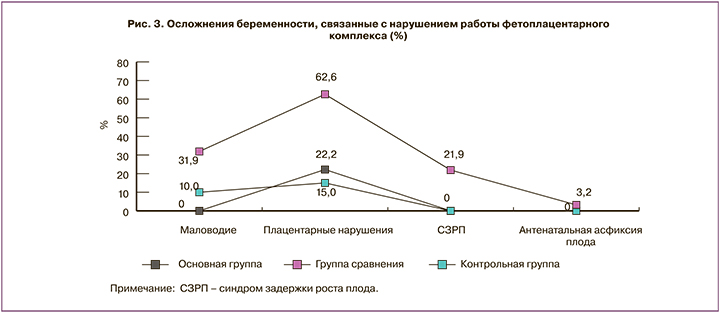
В группе сравнения выявлена внутриутробная гибель плода у 2/62 (3,2%) беременных. Избыточное содержание жировой ткани значимо нарушает процессы гормональной регуляции фертильной функции, вызывая морфологические изменения в эндометрии при имплантации и формировании системы «мать–плацента–плод» [11].
Крайне важна прегравидарная подготовка для ликвидации дисбаланса витаминов и минералов у женщин накануне беременности. В группе пациенток, не принимавших фолиевую кислоту, йод, препараты железа, витамин D3 на этапе преконцепции, во время гестации диагностированы железодефицитная анемия (ЖДА) у 44/62 (71,0%), гипотиреоз – у 13/62 (21,0%) беременных. Врожденных пороков развития во всех группах не выявлено. Дефицит фолатов, особенно в преконцепцию и на ранних стадиях беременности, существенно повышает риск возникновения врожденных пороков (в том числе дефекта нервной трубки), гипотрофии и недоношенности, а также увеличивает риск выкидыша и таких осложнений беременности, как преэклампсия [6, 13].
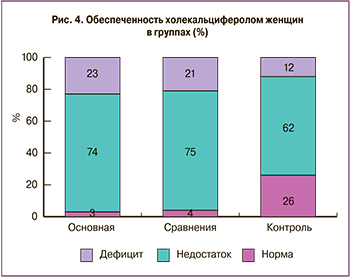 Следует подчеркнуть, что назначение в комплексной подготовке к беременности холекальциферола явилось обоснованным ввиду обнаружения гиповитаминоза D практически у всех женщин (рис. 4).
Следует подчеркнуть, что назначение в комплексной подготовке к беременности холекальциферола явилось обоснованным ввиду обнаружения гиповитаминоза D практически у всех женщин (рис. 4).
Пациентки с ожирением имели дефицит или недостаток витамина D3 (холекальциферола): в основной группе – 60/62 (96,8%), группе сравнения – 30/32 (93,7%). 15/20 (75%) женщин с нормальной массой тела имели низкое обеспечение этим витамином. Поэтому считаем необходимым прием витамина D3 в период подготовки к беременности, вынашивания и грудного вскармливания [14]. Воздействие витамина D на фетальное программирование, регуляцию генов объясняет широкий круг полезных свойств для здоровья человека этого вещества. Достаточное содержание холекальциферола улучшает функции опорно-двигательной системы, снижает риск развития хронических заболеваний, включая рак, аутоиммунных заболеваний, инфекционных болезней, сахарного диабета 2 типа, нейрокогнитивных нарушений [15]. Кроме того, достаточный уровень витамина D способствует нормализации процессов регуляции овуляции, имплантации плодного яйца, функции эндометрия, поддерживает высокую чувствительность тканей к гормональным воздействиям [16].
В программе прегравидарной подготовки для снижения веса был назначен комплексный препарат «Редуксин Форте», сочетающий сибутрамин и метформин. Сибутрамин стимулирует чувство насыщения, нормализует пищевое поведение, усиливает термогенез, а метформин повышает чувствительность периферических тканей к инсулину. Данная комбинация за счет объединения разнонаправленных плейотропных эффектов компонентов позволит повысить эффективность и безопасность терапии ожирения за счет комплексного многофакторного воздействия, при этом сможет увеличить приверженность к терапии за счет простого понятного режима дозирования и удобного способа применения. Женщины детородного возраста с ИМТ≥30 кг/м2 должны получать информацию о рисках, связанных с ожирением, во время беременности и родов. Им необходима помощь в снижении веса до наступления беременности. Поэтапную работу по изменению образа жизни следует проводить во время консультаций по планированию семьи. Вес, ИМТ, ОТ необходимо контролировать регулярно.
Заключение
Предложенная нами программа прегравидарной подготовки с медикаментозной коррекцией ожирения, включающей комплексный препарат «Редуксин Форте», особенно для женщин с висцеро-абдоминальным типом ожирения, витамин D3, йод, фолиевую кислоту и рекомендации по модификации образа жизни, значимо профилактирует гестационные осложнения.
В группе женщин, получавших прегравидарную подготовку, отмечено снижение массы тела и отсутствие репродуктивных потерь. Наш опыт показал, что реже были выявлены плацентарная недостаточность, гестационный сахарный диабет, ЖДА и гипотиреоз по сравнению с группой женщин без прегравидарной подготовки.