The impact of anthropogenic chemicals on the effectiveness of assisted reproductive technologies
Aim. To analyze the relationship between the level of anthropogenic chemicals in female patients and the results of infertility treatment using ART.Frankevich V.E., Syrkasheva A.G., Dolgushina N.V.
Materials and methods. The study included 300 infertile women, who applied to the Center for infertility treatment using ART. Inductively coupled plasma mass spectrometry (ICP-MS) was used to detect heavy metals concentration (mercury, lead, cadmium) in the blood of patients, chromatography-mass spectrometry was used to analyze the level of bisphenol A (BPA). A conventional scale was developed to estimate the total pollutant concentrations in patients. ROC analysis was used to estimate threshold value affecting the likelihood of pregnancy (a score = 5 points) Then the patients were stratified into groups depending on pollutant concentrations. Group 1 included 72 patients, who had high pollutant concentrations. Group 2 included 227 patients, who had low pollutant concentrations.
Results. The clinical and anamnestic characteristics did not differ in the comparison groups. Comparison of embryological parameters showed a significant blastulation rates decline in the group of patients with a high pollutant concedntrations. Absence of embryonic cleavage was in 17.8% of women in group 1 compared to 10.1% in group 2, p=0.0644. Assessment of clinical outcomes of ART cycles showed decreased rates of clinical pregnancy onset and births, increased incidence of early reproductive losses in the group of patients with high pollutant concentrations.
Conclusion. High pollutant concentrations in the bodies of infertile patients is associated with poor embryo quality and decline in the effectiveness of ART programs.
Keywords
The negative impact of environmental pollutants on human health is a relevant problem in the modern world [1, 2]. According to the World Health Organization (WHO), over one fourth of the disease burden in the world and more than half of diseases among children are attributable to environmental factors [3]. The widespread distribution of pollutants, their adverse impact on the environment, biosphere parameters and human health are of great concern for the scientific community.
Environmental pollution (soil, air, water pollution) is understood as qualitative and quantitative changes in its components: increased concentrations of substances specific for the biosphere, the content of biological components, physical factors, or new unspecific components that have an adverse effect on ecosystems and human health [4]. In terms of impact on human reproductive health, the substances that are emitted into the biosphere by human activity or anthropogenic chemicals play the most important role.
The human reproductive system is more vulnerable to the effects of AHV compared to the somatic systems. First, many anthropogenic chemicals are endocrine disruptors, i.e. they can alter the various hormones that regulate the functions of the reproductive system. Secondly, they cause direct damage to reproductive tissues. Thirdly, anthropogenic chemicals negatively affect mitotic cell division, and especially reduction division, leading to disruption of oogenesis, spermatogenesis, and early embryonic development. Some studies showed the negative impact of anthropogenic chemicals on reproductive health [5–7], however, the analysis of only individual substances is a significant drawback. The study of the effects of anthropogenic chemicals on reproductive health is an important goal of scientific research.
The aim of the study was to analyze the relationship between the level of anthropogenic chemicals in female patients and the results of infertility treatment using ART.
Materials and methods
The prospective study included 300 married couples, who applied to the Center for infertility treatment using ART in the period from 2017 to 2018. All patients had no contraindications for treatment.
The inclusion criteria were: normal karyotype of both spouses, fertile or subfertile sperm of the spouse, woman's age from 18 to 39 years, inclusively, woman's body mass index (BMI) from 19 to 25 kg/m2 inclusively. Exclusion criteria were: the use of donor gametes or surrogacy, as well as obtaining 3 or less oocytes on the day of transvaginal ovarian puncture. All patients had permanent residence in Moscow for the last 5 years.
All married couples included in the study were examined according to the Order No. 107n of 30.08.2012 of the Ministry of Health of Russia “About the use of assisted reproductive technologies, contraindications and limitation for their use” [3].
Ovarian stimulation was performed according to the protocol for gonadotropin-releasing hormone antagonists, the dose of gonadotropins was selected individually by the doctor in charge of the patient’s treatment. Transvaginal puncture, embryonic stage, embryo transfer into the uterine cavity, luteal phase and post-transfer period support in all patients was performed according to the standard protocol [8]. Fertilization of oocytes was carried out using intracytoplasmic sperm injection in oocytes.
Venous blood collection was performed on the day of transvaginal puncture, then the samples were cryopreserved at t=-70°C. Pollutant levels (mercury, lead, cadmium, bisphenol A) were detected using mass spectrometry.
Visualization of gestational sac in the uterine cavity 3 weeks after embryo transfer showed clinical pregnancy.
Statistical analysis
Statistica 12 software package (USA) was used for statistical analysis. The data with abnormal distribution were presented as median (interquartile range). For statistical analysis, χ2-test was used for comparison of categorical variables. Mann–Whitney U-test and Kruskal–Wallis test were used for comparison of differences in medians (for abnormal data distribution). A χ2-test was performed after construction of contingency tables. Fisher's exact test was used for testing small samples. To compare the binary data, a measure of comparative risk was the relative risk (RR) with 95% confidence interval (95% CI).
The differences between the values were considered to be statistically significant at р˂0.05.
The study was approved by the Ethics Committee of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. All patients under the study have signed informed concent.
Results
The patients included in the study were middle-aged women with a normal BMI and ovarian reserve. Median age was 31 years (29–34), BMI – 21.6 kg/m2 (20.4–23.5), anti-Müllerian hormone (AMH) level was 3.2 ng/ml (1.9–5.8). Lead, cadmium, mercury and bisphenol A levels in the blood were measured in all patients. A conditional scale was developed to assess the total level of pollutants in the body. The score of 1 point was used for the substance level exceeding the median value, 2 points – when it exceeded the upper quartile and 3 points for ≥ 97.5 percentile. Thus, the assessment score of pollutant levels in each patient had a certain number of points (Table 1).
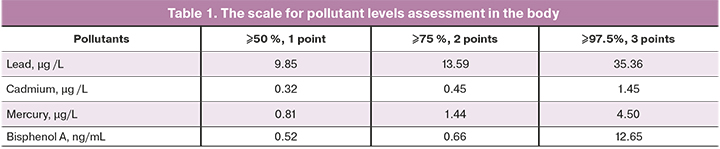
The median value scored 3 points, the interquartile range was 2–4 points, minimal value was 0 point and maximal value was 9 points. The number of points for the levels of heavy metals had a positive relationship (p<0.05), but had no correlation with the number of points for the level of bisphenol A. ROC analysis was used to identify threshold values that affected the chances of pregnancy onset (5 points). Then the patients were divided into groups depending on the level of pollutants: group 1 consisted of 73 patients with 5 or more points, group 2 consisted of 227 patients with 4 or less points.
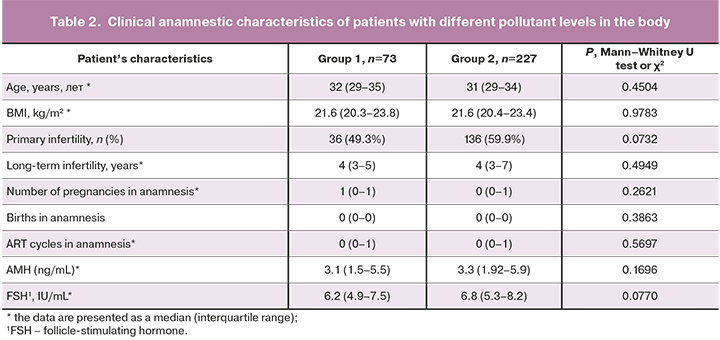
The analysis of clinical anamnestic characteristics did not show statistically significant differences between the groups (Table 2).
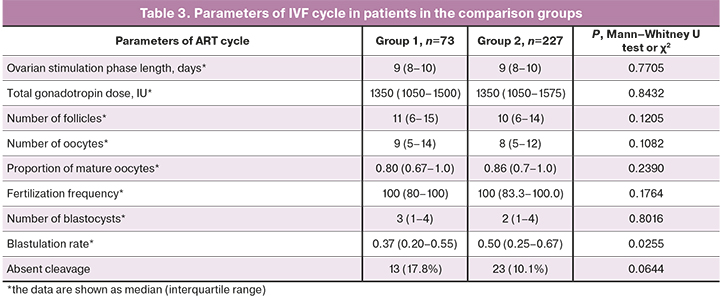
Further, the parameters of the ovarian stimulation cycle were analyzed. There were no differences in the duration of ovarian stimulation and the total dose of gonadotropins.
Comparison of embryological parameters showed a borderline significant blastulation rates decline in the group of patients with a high pollutant levels. Absent cleavage was in 17.8% of women in group 1 compared to 10.1% of women in group 2, р=0.644, RR=1.6 (95% CI, 0.98; 2.59) (Table 3).
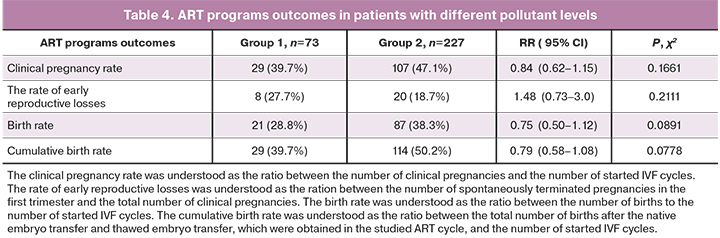
Assessment of clinical outcomes of ART cycles showed a tendency towards reduced clinical pregnancy and birth rates, increased rate of early reproductive losses in the group of patients with high pollutant levels (Table 4). Despite the absence of statistically significant differences between the groups, the birth rate in the group with high pollutant levels was 28.8%, compared to 38.3% in the group women low pollutant levels (delta 9.5%).
Discussion
This study is characterized by determination of levels of different pollutants (metals/organic compounds) in the blood of infertile patients, who applied for infertility treatment using ART programs.
A positive correlation was noted between the levels of heavy metals (i.e. mercury, lead and cadmium) in the same patients. This may be due to the genetic predisposition to heavy metal accumulation (since metals have a long period of elimination from the body).
At the same time, it should be noted that there was no connection between heavy metals and bisphenol A. The increased exposure to bisphenol A is more likely to be related to lifestyle rather than to genetic characteristics of the body.
Based on this study, a conditional scale was developed to assess the total pollutant levels (heavy metals and bisphenol A) in a patient’s body.
Determination of threshold scores made it possible to divide the patients into groups depending on low and high pollutant levels in the body. Assessment of the embryonic stage showed decreased embryo quality in the group of women with high pollutant levels. The negative impact of anthropogenic organic chemicals on oocytes and embryos (induction of apoptosis, impairment of mitotic cell division and reduction division) have been shown in animal models [9]. A similar effect is also expected in humans, although the pathogenetic mechanisms of anthropogenic chemicals exposure are still poorly understood. [10].
Assessment of clinical outcomes of IVF cycles showed a tendency towards reduced clinical pregnancy and birth rates in the group of patients with high pollutant levels, although the differences did not reach statistical significance. The obtained data correlated with the published data: the studies showed the effect of anthropogenic chemicals on different aspects of embryonic stage, sperm parameters or steroid hormone levels, however a direct relationship between the level of anthropogenic chemical and clinical outcomes have not been registered [11]. The lack of a clear statistical relationship between the level of anthropogenic chemicals and IVF outcomes complicates calculation of threshold levels for individual substances. However, most researchers are of the opinion that anthropogenic chemicals may have a toxic effect even in small concentrations. [12]. The data obtained in this study confirm a toxic effect of anthropogenic chemicals on human’s reproductive system, especially with the combined effects of several substances.
Conclusion
High pollutant levels in the bodies of infertile patients is associated with reduced embryo quality and decline in the effectiveness of ART programs.
References
- Казанцева Е.В., Долгушина Н.В., Ильченко И.Н. Влияние антропогенных химических веществ на течение беременности. Акушерство и гинекология. 2013; 2: 10-7. [Kazantseva E.V., Dolgushina N.V., Ilchenko N.V. Impact of the pollutants on pregnancy. Akusherstvo i ginekologiia/Obstetrics and Gynecology. 2013; 2: 10-7 (in Russian)].
- Долгушина Н.В., Казанцева Е.В., Пивоварова Л.В. Влияние антропогенных химических веществ на массу тела новорожденных. Акушерство и гинекология. 2013; 12: 58-64. [Dolgushina N.V., Kazantseva E.V., Pivovarova L.V. Impact of the pollutants on the newborns weight. Akusherstvo i ginekologiia/Obstetrics and Gynecology. 2013; 12: 58-64 (in Russian)].
- Всемирная организация здравоохранения. Окружающая среда и социальные детерминанты здоровья. 2017. [WHO. Environment and social determinants of health. 2017].
- Чебышев Н.В., Филиппова А.В. Основы экологии. М.: Новая Волна; 2004. 335с. [Chebyshev N.V., Filippova A.V. Ecology. 2004. 335 p. (in Russian)].
- Poormoosavi S.M., Behmanesh M.A., Janati S., Najafzadehvarzi H. Level of bisphenol A in follicular fluid and serum and oocyte morphology in patients undergoing IVF treatment. J. Family Reprod. Health. 2019; 13(3): 154-9.
- Paoli D., Pallotti F., Dima A.P., Albani E., Alviggi C., Causio F. et al. Phthalates and bisphenol A: presence in blood serum assisted reproduction techniques. Toxics. 2020; 8(4): 91. https://dx.doi.org/10.3390/toxics8040091.
- Pizzol D., Foresta C., Garolla A., Demurtas J., Trott M., Bertoldo A. et al. Pollutants and sperm quality: a systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2021; 28(4): 4095-103. https://dx.doi.org/10.1007/s11356-020-11589-z.
- Сыркашева А.Г., Долгушина Н.В., Макарова Н.П., Агаршева М.А., Ковальская Е.В. Исходы программ вспомогательных репродуктивных технологий у пациенток с дисморфизмами ооцитов. Акушерство и гинекология. 2015; 7: 56-62. [Syrkasheva A.G., Dolgushina N.V., Makarova N.P., Kovalskaya E.V., Agarsheva M.A. IVF outcomes in patient with oocyte dysmorphisms. Akusherstvo i ginekologiia/Obstetrics and Gynecology. 2015; 7: 56-62 (in Russian)].
- Liao B.Q., Liu C.B., Xie S.J., Liu Y., Deng Y.B., He S.W. et al. Effects of fine particulate matter (PM(2.5)) on ovarian function and embryo quality in mice. Environ. Int. 2020; 135: 105338. https://dx.doi.org/10.1016/j.envint.2019.105338.
- Chianese R., Troisi J., Richards S., Scafuro M., Fasano S., Guida M. et al. Bisphenol A in reproduction: epigenetic effects. Curr. Med. Chem. 2018; 25(6): 748-70. https://dx.doi.org/10.2174/0929867324666171009121001.
- Hornstein M.D. Lifestyle and IVF outcomes. Reprod. Sci. 2016; 23(12): 1626-9. https://dx.doi.org/10.1177/1933719116667226.
- Rattan S., Zhou C., Chiang C., Mahalingam S., Brehm E., Flaws J.A. Exposure to endocrine disruptors during adulthood: consequences for female fertility. J. Endocrinol. 2017; 233(3): R109-29. https://dx.doi.org/10.1530/JOE-17-0023.
Received 20.05.2021
Accepted 04.06.2021
About the Authors
Vladimir E. Frankevich, PhD, Head of Department of Systems Biology in Reproduction, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. Tel.: +7(495)438-07-88. E-mail: v_frankevich@oparina4.ru. 4 Oparina str., 117997, Moscow, Russia.Anastasia G. Syrkasheva, PhD, Senior Researcher of the IVF Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: a_syrkasheva@oparina4.ru. 4 Oparina str., 117997, Moscow, Russia.
Nataliya V. Dolgushina, Dr. Med. Sci., Professor, Deputy Director – Head of the Department of Research Administration, V.I. Kulakov National Medical Research Center
for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: n_dolgushina@oparina4.ru. 4 Oparina str., 117997, Moscow, Russia.
For citation: Frankevich V.E., Syrkasheva A.G., Dolgushina N.V. The impact of anthropogenic chemicals on the effectiveness of assisted reproductive technologies.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 7: 102-106 (in Russian)
https://dx.doi.org/10.18565/aig.2021.7.102-106



