Заболевания шейки матки, ассоциированные с вирусом папилломы человека (ВПЧ), являются важной медико-социальной проблемой, что связано, с одной стороны, с доказанной ролью данного возбудителя в генезе рака шейки матки (РШМ), его значительной распространенностью, а с другой стороны, с возможностью профилактики, ранней диагностики и лечения вызванных им заболеваний [1].
Так, согласно исследованиям рабочей группы Всемирной организации здравоохранения (ВОЗ), папилломавирусная инфекция (ПВИ) признана одной из самой распространенной в мире [2, 3], в том числе и в Российской Федерации [4, 5].
Особого внимания заслуживает группа женщин репродуктивного возраста, в которой отмечены рост заболеваемости и «омоложение» злокачественной ВПЧ-ассоциированной патологии шейки матки [6]. В частности, за последние 10 лет частота РШМ у женщин до 40 лет возросла на 64,2%, в группе до 29 лет – на 150% [7].
Известно, что РШМ у беременных встречается значительно чаще других злокачественных опухолей [8].
Как правило, наличие ПВИ у беременных сочетается с различными видами урогенитальных инфекций и сопровождается изменением местного иммунитета. Частота развития гестационных осложнений и неблагоприятных исходов беременности при ПВИ достоверно выше при наличии клинических проявлений заболевания. Следовательно, необходимость дифференцированного подхода к проведению прегравидарной подготовки и ведению беременности у женщин с ПВИ очевидна [6].
В литературе имеются разноречивые мнения о течении беременности и родов после хирургического лечения шейки матки [9], однако большинство исследователей отмечает, что более чем у 50% женщин с любыми инвазивными вмешательствами в анамнезе имеются различные осложнения гестационного периода и родов [7, 10]. В доступных источниках нет акцентов на необходимость мониторинга цервикального статуса у данной группы пациенток, что является основой профилактики невынашивания беременности при анатомически неполноценной шейке матки.
Цель исследования: провести анализ течения беременности с оценкой цервикального статуса и родов у пациенток, пролеченных ранее по поводу различных форм ВПЧ-ассоциированной патологии.
Материал и методы исследования
Проведен анализ течения беременности и родов у 128 пациенток, имевших в анамнезе ВПЧ-ассоциированную цервикальную патологию с использованием различных лечебных методик.
Обследуемые были разделены на 2 группы. Первую группу (N1=56) составили женщины с наступившей беременностью, пролеченные ранее по поводу цервикальных интраэпителиальных неоплазий (ЦИН) I-. Ретроспективно мы разделили данную группу пациенток на 2 подгруппы: подгруппа N1A – 30 пациенток, в отношении которых при предшествующем лечении была выбрана консервативная тактика (53,6%) и подгруппа N1В – 26 женщин, подвергшиеся ранее радиоволновому деструктивному лечению (46,4%). Вторую группу (N2=72) составили беременные, которым по поводу плоскоклеточных изменений высокой степени была проведена конизация шейки матки.
Всем пациенткам выполнялось обязательное обследование в соответствии с порядком оказания помощи, определенным приказом 572н, включающее:
- общеклиническое исследование (изучение жалоб, анамнеза, менструальной и детородной функции, симптомов заболевания, характера сопутствующей гинекологической и экстрагенитальной патологии, наличия факторов риска прерывания беременности);
- общий осмотр и гинекологическое исследование;
- лабораторная диагностика: микроскопия отделяемого нижнего отдела генитального тракта; жидкостная цитология.
- инструментальные методы исследования – ультразвуковое исследование.
Статистическая обработка полученных результатов проводилась с использованием программы Microsoft Excel 2010, Statistica 10.0. Для оценки показателей применялись критерий χ2 и критерий Стьюдента для долей. Различие между сравниваемыми величинами признавали статистически значимыми при вероятности ошибки p<0,05.
Результаты и их обсуждение
При анализе возрастного состава в группах обследованных установлено, что возраст беременных женщин, вошедших в исследование, колеблется от 17 до 45 лет. Средний возраст обследованных в группе N1 оказался равным 27,9±0,7 года, причем пик наступления беременности (50%) приходился на возрастной интервал 26–30 лет. В группе N2 беременность наступила в возрасте 31–35 лет – 51,4% женщин, а средний возраст составил 32,4±1,2 года, что достоверно больше (р=0,01), чем в группе N1. Достоверно значимое преобладание беременностей у пациенток с ВПЧ-ассоциированными ЦИН-I, по-видимому, обусловлено их более молодым возрастом и, соответственно, желанием реализовать репродуктивную функцию (р=0,0002).
Сравнение фертильного анамнеза показало, что больше половины женщин были первобеременными (51,6%), но в группе N1 они составили 62,5%, а в группе N2 – 40,3%, что достоверно реже (р<0,05), и, по-видимому, также ассоциировано с возрастом пациенток.
Анализ исхода предыдущих беременностей не выявил принципиальных различий в частоте медицинских абортов, неразвивающейся и внематочной беременности по группам. В то же время обращал на себя внимание тот факт, что самопроизвольный выкидыш достоверно чаще (р=0,01) встречался в группе N2 (12,5% в группе N1 и 23,6% в группе N2). Следует отметить, что различалась также частота поздних выкидышей, причем в группе N1 их число было достоверно (р=0,0004) меньше – 3,6% (в группе N2 – 13,9%).
В собственном исследовании распределение пациенток второй группы в зависимости от метода хирургического лечения цервикальной патологии представлено следующим образом: 43 (59,7%) женщины перенесли электрорадиоволновую конизацию, а у 29 (40,3%) обследованных применялась радиоволновая конизация. Следует отметить, что каждая из методик сочеталась или не сочеталась с фотодинамической терапией.
В нашем исследовании проанализирован временной интервал между лечением и наступлением беременности у пациенток второй группы. Выяснилось, что пик наступления беременности (66,7%) достоверно (р<0,05) приходился на период от 1,5 до 2 лет от проведенного хирургического вмешательства.
При настоящей беременности всем женщинам проводили динамическое наблюдение за состоянием шейки матки.
У всех 128 пациенток с наступившей беременностью обследование и лечение инфекций, передающихся половым путем, с контролем эффективности было проведено в прегравидарном периоде.
При анализе данных микроскопии отделяемого нижнего отдела генитального тракта установлено, что беременные с различными формами ВПЧ-ассоциированной цервикальной патологии подгруппы N1В, подвергшиеся ранее радиоволновой деструкции, так же, как и пациентки второй группы N2, перенесшие конизацию шейки матки, имели более благополучную бактериоскопическую картину влагалищного биотопа в сравнении с пациентками подгруппы N1А без физиохирургического воздействия в анамнезе. Так, сравнительный анализ состояния биоценоза нижнего отдела гениталий выявил достоверное преобладание (р<0,05) состояния нормоценоза у пациенток подгруппы N1В и группы N2 в сравнении с беременными подгруппы N1А, не имевшими физиохирургического воздействия на патологически трансформированный цервикальный эпителий. В собственных исследованиях различий результатов цитологического исследования в группах беременных не было (р>0,05).
У всех беременных нами были оценены в динамике (с 10-й по 22-ю неделю гестации с интервалом 12–14 дней) эхографические параметры состояния шейки матки, включающие измерение длины, ширины цервикального канала, отношение длины шейки матки к ее диаметру на уровне внутреннего зева и определение особенностей ее эхоструктуры.
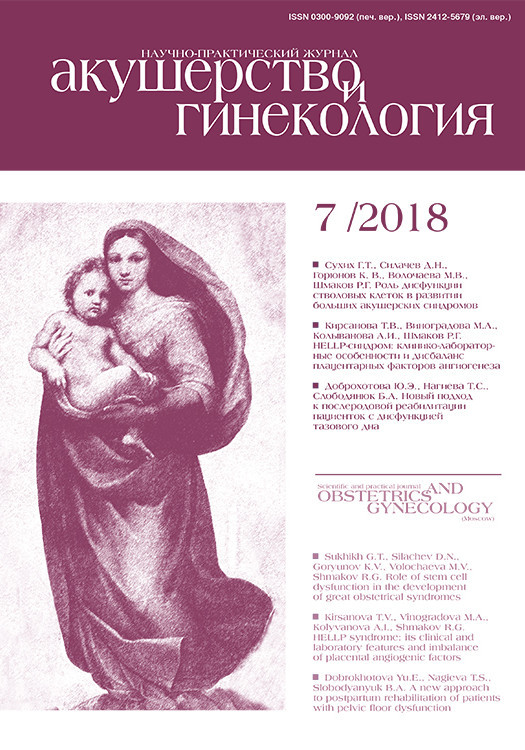
У беременных с доброкачественными ВПЧ-ассоциированными цервикальными состояниями длина шейки матки во II триместре составила 36±4 мм. Динамика изменений длины шейки матки в зависимости от срока беременности в подгруппе N1 представлена на рис. 1.
У 3 женщин (5,3%) данной группы была диагностирована истмико-цервикальная недостаточность, им был проведен серкляж по МсDonald и назначен микронизированный прогестерон.
Ширина цервикального канала в среднем составила 2,4±0,8 мм.
Прогностическим признаком угрозы прерывания беременности считали снижение отношения длины шейки матки к ее диаметру на уровне внутреннего зева до 1,16±0,04 при норме, равной 1,53±0,03. В собственном наблюдении в первой группе беременных данный показатель составил 1,64.
Изменения эхоструктуры ткани шейки матки, предшествующие ее укорочению, эхографически проявляющиеся в виде мелких жидкостных включений и ярких штриховых сигналов, в наших исследованиях диагностированы у 1 беременной (1,8%) группы N1.
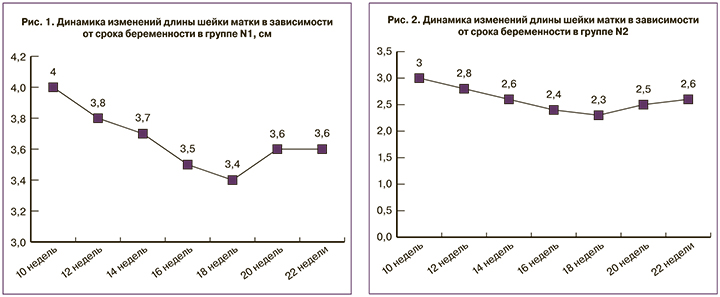
Средняя длина шейки матки в группе беременных, перенесших ранее хирургическое лечение тяжелых ВПЧ-ассоциированных заболеваний шейки матки, была достоверно (р<0,01) меньше, чем в группе N1, и составила 26,2±3,4 мм. Истмико-цервикальная недостаточность диагностирована у 15 (20,8%) беременных группы N2, что достоверно (р<0,05) в 3,9 раза чаще, чем у пациенток группы N1. Наиболее выраженное укорочение шейки матки так же, как и в группе N1, имело место в сроки от 16 до 18 недель (рис. 2).
Ширина цервикального канала также значительно превысила (р<0,01) этот показатель в первой группе. Отношение длины шейки матки к диаметру на уровне внутреннего зева в группе N2 было ниже (р<0,05), чем в группе N1, и составило 1,23. Что касается структурных изменений шейки матки, то эхографические признаки, предшествующие истмико-цервикальной недостаточности, наблюдались у 21 беременной (29,2%).
13 пациенткам группы N2 при выявлении истмико-цервикальной недостаточности проводили хирургическую коррекцию в виде серкляжа по МсDonald, вводили силиконовые пессарии доктора Арабин и назначали микронизированный прогестерон. Двум пациенткам в связи с отсутствием технических возможностей наложения швов вследствие резкого укорочения влагалищной порции шейки матки лечение истмико-цервикальной недостаточности ограничили введением серкляжного пессария и назначением микронизированного прогестерона.
Исходы беременности в нашем исследовании были следующими: беременность у 41 (73,2%) женщины первой группы завершилась своевременными родами, из них у 8 (19,5%) путем кесарева сечения. Показаниями к оперативному родоразрешению в данной группе беременных были декомпенсированная фетоплацентарная недостаточность (2 пациентки – 25%), упорная первичная слабость родовой деятельности (2 женщины – 25%), сопутствующая соматическая патология (2 женщины – 25%), несостоятельность рубца на матке после кесарева сечения (1 женщина – 12,5%) и клинически узкий таз (1 женщина – 12,5%).
В группе N2 своевременными родами завершилось 28 беременностей (38,9%), что значительно реже (р<0,05), чем в первой группе. Из них у 21 (71,4%) женщины роды произошли через естественные родовые пути, а у 7 (28,6%) путем кесарева сечения, что несколько выше в сравнении с группой N1. У 3 женщин операция кесарева сечения была выполнена по поводу дистоции шейки матки, у 1 – из-за отсутствия биологической готовности шейки матки к родам при преждевременном разрыве плодных оболочек, у 1 беременной – в связи с декомпенсированной фетоплацентарной недостаточностью. У 2 пациенток показанием к оперативному родоразрешению была рубцовая деформация шейки матки после конизации.
Также заслуживает внимания достоверное (р<0,05) превышение в группе N2 как поздних, так и ранних выкидышей: в группе N1 они имели место у 5 (8,9%) и у 4 (7,2%) женщин, тогда как в группе N2 – в 15 (20,9%) и 13 случаях (18,0%) соответственно.
Преждевременные роды также достоверно чаще (р<0,05) встречалисьу пациенток группы N2 – у 16 (22,2%) пациенток по сравнению с женщинами из группы N1 –у 5 (8,9%) пациенток.
Таким образом, при появлении у пациенток симптомов угрозы прерывания беременности необходимо комплексное лечение, направленное на сохранение беременности: коррекция микробиоценоза влагалища, применение серкляжа по МсDonald и введение пессария доктора Арабин, использование микронизированного прогестерона. Применяемая терапия позволяет добиться прогрессирования беременности до срока родов.
Заключение
У женщин после физиохирургического лечения по поводу интраэпителиальных поражений высокой степени риск преждевременных родов (р<0,05) выше, чем у пациенток после лечения цервикальных состояний ЦИН-I. Истмико-цервикальная недостаточность, установленная по эхографическим параметрам шейки маки, в 3,9 раза чаще (р<0,05) имеет место после оперативного вмешательства на шейке матки. Наиболее выраженное укорочение шейки матки при ВПЧ-ассоциированной эпителиальной патологии наблюдается в сроки 16–18 недель беременности, в связи с чем необходим динамический контроль ультразвуковых признаков истмико-цервикальной недостаточности каждые 10–14 дней с 10-й по 22-ю неделю гестации с целью своевременного решения вопроса о ее коррекции.