COMPARING THE EFFECTIVENESS OF SURGICAL AND CONSERVATIVE MANAGEMENT OF PREGNANT WOMEN WITH ISTHMIC-CERVICAL INSUFFICIENCY AND PROLAPSED FETAL MEMBRANES
Objective. Isthmic-cervical insufficiency (ICI) is the adverse for the prolapsed membrane (PM) is extremely unfavorable in terms of early and very early preterm birth, as well as high levels morbidity. The results of recent studies show that rescue cerclage with the appointed tocolytics and glucocorticoids significantly increases the chances of neonatal survival. At the same time, the enrolment for rescue cerclage at ICI and PM requires a convincing evidence base and further clinical studies.Tskhay V.B., Dudina A.Y., Kochetova E. E., Lobanova T.T., Reodko S.V., Mikhailova A.V., Domracheva M.Y., Konovalov V.N., Bezruk E.V.
To analyze obstetric and perinatal outcomes in pregnant women with ICI after expectant management and bed rest.
Materials and methods. The study included 97 patients with ICI and PM in the gestation period of 19—26 weeks. The first group consisted of 65 pregnant women with active tactics (rescure serclage). The second group of 32 pregnant women underwent conservative management tactics (bed rest). The patients of both groups received traditional courses of antibacterial therapy and prophylaxis of fetal respiratory distress syndrome.
Results and discussion: performance of cerclage by the method of Mac-Donald with the active management of patients with ICI and the PM was conducted with the additional manipulation, including the holding of transabdominal amnioreduction under the control of echography, tight filling the bladder and intracervical introduction of the Foley catheter. The use of active tactics facilitated pregnancy prolongation for 8 weeks(in average), while holding conservative tactics – only for1.5 weeks. In the first group of patients, the delivery period averaged 30,75±5,5 weeks, in the second group – 25,7±1,7 weeks (p < 0.05). In 38,5% of cases with active tactics the pregnancy prolonged till term gestation.
Conclusion. Active management tactics of pregnant women with ICI and PM have significant advantages in comparison with conservative tactics, prolongs pregnancy for a longer period and reduces the level of perinatal losses.
Keywords
Preterm birth is one of the leading causes of neonatal morbidity and mortality. Most adverse perinatal outcomes are associated with extremely preterm births [1–3]. According to K. Costeloeetal, in 2006, the survival of live born babies was 2%for those born at 22 weeks’ gestation, 19% at 23 weeks, 40% at 24 weeks, 66% at 25 weeks, and 77% at 26 weeks [4]. Despite medical-technological advances and achievements in the provision of neonatal care, the mortality, morbidity, and disability of infants born at 24 to 26 weeks’ gestation remain very high [5-7].
The results of recent studies show that shortened sonographic cervical length is a fairly reliable diagnostic predictor of spontaneous preterm birth [8].
The presence of a shortened cervical length very often co-occurs with isthmic-cervical insufficiency (ICI), which is one of the leading causes of very and extremely preterm birth [9, 10].
A pronounced dilatation of the internal cervical os and prolapse of the membranes into the endocervical canal is a challenging clinical situation and sometimes unsolvable problem in terms of preserving pregnancy and perinatal outcomes [11, 12].
The impact of the vaginal microflora on the lower pole of the protruding membranes increases the risk of infectious complications or rupture of the membranes resulting in preterm birth, especially in the absence of timely and adequate intervention [13, 14]. That is why many experts consider it imperative that prophylactic cervical cerclage is made before 26 weeks’ gestation in women with ICI even with severely prolapsed membranes to prevent preterm birth, especially the extremely early one [14, 15].
ICI can be managed by both surgical and conservative means. The effectiveness of these methods, the pregnancy outcomes as a result of their use has been a subject of debate in both the international and domestic literature. So far, there is no consensus among researchers involved this discussion regarding the choice of a method for treating ICI [16].
In recent years, several studies have been published aimed at comparing of the effectiveness of active (cervical cerclage) versus expectant (bed rest) management of pregnant women with ICI and prolapsed fetal membranes [17, 18].
Many experts consider active management of pregnant women with ICI and prolapsed fetal membranes more effective than expectant management in terms of prolonging pregnancy and reducing perinatal morbidity and mortality [19, 20].
At the same time, further studies investigating this issue are needed due to adverse sequelae associated with ICI and prolapsed fetal membranes in relatively early pregnancy (second trimester), and high rates of perinatal morbidity and mortality.
This study aimed to compare obstetric and perinatal outcomes in women undergoing surgical or conservative management for ICI and prolapsed fetal membranes.
Materials and methods
The study was conducted at the Krasnoyarsk Regional Clinical Center for Maternity and Child Care. The study comprised 97 patients with ICI and prolapse of fetal membranes at 19-26 weeks’ gestation. Group I consisted of 65 patients who underwent surgical correction of ICI by the Mac-Donald technique with prior amnioreduction, tight filling of the urinary bladder, and the use of a Foley catheter to displace the lower uterine segment and protruding membranes upward. Group II (comparison group) included 32 women at 22–26 weeks’ gestation with ICI and prolapse of fetal membranes, who received conservative management (bed rest, prophylactic drugs). Patients in both groups received identical antibacterial therapy and corticosteroids for the prevention of neonatal respiratory distress syndrome.
Statistical analysis was performed using SPSS Statistics 22.0. The normality of the distribution was tested by the Shapiro-Wilk test. When quantitative variables were normally distributed, the results were expressed as the mean value (M) and standard deviation (SD). Otherwise, the median and the quartiles were reported (Me [Q1; Q3]). Statistical significance for comparisons of normally distributed data was determined by Student’s t-test for independent samples. Comparing numerical data not showing normal distribution was performed with the nonparametric Mann-Whitney test. Categorical variables were compared with the chi-square test (χ2). A value of p < 0.05 was considered statistically significant.
Results and discussion
Patients in both groups were comparable in age, gestational age, and the number of prior pregnancies and births. The mean age of patients group I and II was 31.03 (4.72) and 30.75 (4.9) years, respectively (p = 0.82). In the whole study cohort, 44%, 27%, and 16% of patients had a history of surgical termination of pregnancy, spontaneous miscarriage, and early fetal demise, respectively. The mean number of prior pregnancies and births in the total cohort was 3.59 [3.1; 4.07] and 0.92 (0.8), respectively.
There were no significant differences in gestational ages between group I [23.01 (1.8)] and II [22.8 (2.8)] at the time of diagnosis of prolapsed fetal membranes (p = 0.47). It should be particularly noted that 20.6% (n = 20) of patients in both groups had previously undergone ICI correction at 15 to 19 weeks’ gestation, which later proved ineffective. Moreover, 55% (n = 11), 20% (n = 4), and 25% (n = 5) of patients used obstetric pessary, underwent a cervical cerclage, and were treated with both pessary and cervical cerclage, respectively. The proportion of such patients was approximately equal in group I (20%, n = 13) and II (22%, n = 7).
Upon admission to the hospital, all patients underwent clinical and laboratory examination, including white blood cell count, C-reactive protein (CRP), and the quantitative bacteriology of the vaginal flora.
In both study groups, the white blood cell count at admission was within normal range: (11.28 (2.3) × 109/l in group I and 12.94 (4.1) × 109/l in group II) (p = 0.06). There were no statistically significant differences in CRP level either: 0.2 (0.69) mg/l in group I and 0.5 (0.3) mg/l in group II (p = 0.06). These findings implied the absence of any inflammatory process at the time of hospitalization in both groups.
Before the surgical correction, cultures of vaginal specimens were obtained from patients of group I. In 44.6% of them, no growth of microflora was found, 16.6% of patients had Lactobacillus species; occasionally, typical representatives of the vaginal flora - conditionally pathogenic microorganisms were found (Fig. 1).
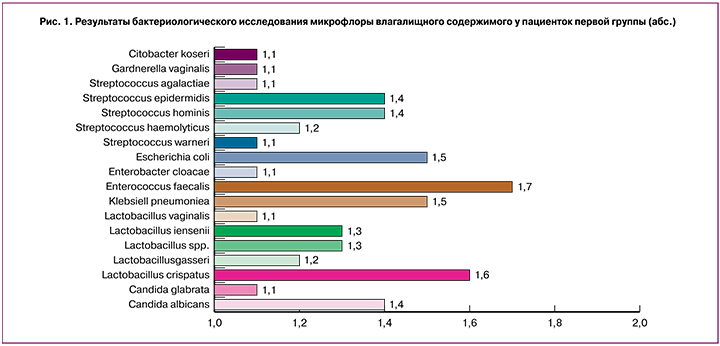
At the same time, microscopic examination of Gram-stained vaginal smears showed that 55% of patients had an inflammatory type of smear, 27% had a dysbiosis-type smear, and only 18% of patients had normal smears.
Surgical correction of ICI for prolapsed fetal membranes involved a whole set of measures aimed primarily at preserving the integrity of the membranes during cervical cerclage. This complex of measures included the following: 1) ultrasound-guided transabdominal amnioreduction aspirating 50-80 ml of amniotic fluid depending on the amniotic fluid index and gestational age to relieve tension from the lower pole of the membranes; 2) tight filling of the urinary bladder through a Foley catheter with 300 ml of warm sodium chloride solution to displace the prolapsed membranes upward above the internal os, Scherer technique; 3) intracervical placement of a Foley catheter to replace the membranes into the lower uterine segment above the internal os; 4) using monofilament as suture material (supolen, mersilene tape); 5) adequate anesthesia (predominantly regional anesthesia); 6) subsequent postoperative drug support including tocolysis with gynipral for 48 hours, micronized vaginal progesterone (400 mg/day) from the first postoperative day, antibiotic therapy for 7-10 days, and a 24 hour course of dexamethasone for the prevention of neonatal respiratory distress syndrome. Similar drug therapy was administered to the patients in group II, who chose conservative management (bed rest).
It should be noted that 13.3% of patients (6 out of 65) who chose surgery, experienced a cervical cerclage failure. The duration of pregnancy prolongation among patients in group I and II was 71.6 days (10.1 weeks) and 17.4 days (2.4 weeks), respectively (p <0.001). The median gestational age at delivery was 31.3 [29.7; 38.4] and only 25 [24.4; 32.5] weeks among patients in group I and II, respectively (p <0.001). In group I, the pregnancy prolongation was 8 weeks longer than in group II. However, the in-hospital length of stay at the Department of Pathological Pregnancy was significantly longer in group I than in group II [17.6 (12.8) vs. 11.2 (12.3) days] (p = 0.01).
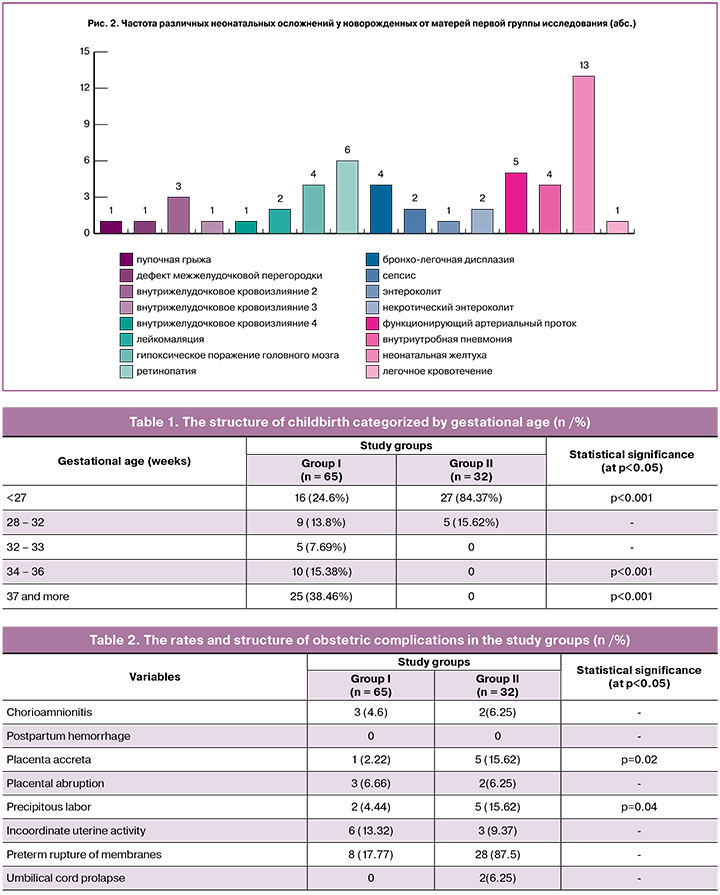
In group II, early and extremely preterm births with low and extremely low birth weight preterm deliveries were statistically significantly more common and there were no full-term newborns in this group (Table 1). In group I, only 24.6% of patients gave birth to newborns with extremely low birth weight, and 38.4% of patients achieved a full term delivery (almost every third patient).
The mode of delivery in the comparison groups did not significantly affect the perinatal results. The rate of cesarean delivery was 22% (13 out of 65) and19.4% (6 out of 32) in group I and II, respectively(p = 0.76). The mean gestational age at the time of cesarean delivery was 32.2 (4.3) and 26.8 (1.8) weeks (p <0.001) in group I and II, respectively. In group I, 38.4% (n = 5) of cesarean sections were performed beyond 37 weeks’ gestation.
Indications for cesarean section were a footling breech presentation, placental abruption, the presence of two or more uterine scars, and non-obstetric comorbidities. Proportions of these indications were similar in both groups.
Analysis of obstetric complications at all stages of the management of these patients in both groups (during pregnancy prolongation, during labor and the postpartum period) showed no statistically significant differences in the incidence of chorioamnionitis, postpartum hemorrhage, and placental abruption. At the same time, patients who chose expectant management were more likely to experience precipitous labor and placenta accreta (table 2).
We carried out a comparative analysis of some of the main perinatal indicators, including newborns’ birth weight, Apgar scores, and immediate and long-term neonatal complications.
Owing to greater pregnancy prolongation and higher gestational age at the time of delivery, the mean birth weight of newborns group I was significantly higher than in group II, respectively (2110.83 [1808.76; 2412.90] vs. 810.15 [700.0; 920.23] gram) (p <0.001). The first-minute Apgar scores among newborns in Group I and II were 7 [5; 8] and 2 [1.5; 3.5], respectively (p <0.001).
The rate of perinatal losses in group I (6.6%) was significantly lower than in group II (57.2%) (p <0.001). Early neonatal death occurred in 3.4% (n = 2) and 16.6% (n = 6) newborns in group I and II (p = 0.02); there were 2 (3.5%) and 10 (31.25%) intrapartum deaths in group I and II, respectively (p <0.001). Also, 12.3% (n = 4) of infants in group II died more than 7 days after their birth and were included in the structure of infant mortality. Considering the high incidence of intrapartum deaths in group II, we analyzed the gestational age at the time of delivery in this cohort, which was 24.4 (1.7) weeks; however, only one patient (10%) gave birth at 29 weeks. This patient had epilepsy and underwent a cesarean section after going into labor. The high incidence of perinatal losses in group II was associated with deep prematurity, extremely low birth weight, and infectious complications.
Many of preterm newborns need some form of initial respiratory support in the first minutes and days of life due to the immaturity of their lungs. There was a direct relationship between the rate of neonatal respiratory distress syndrome and the degree of prematurity. In our study, 28% of newborns from mothers in group I and 95.2% in group II needed respiratory support by mechanical ventilation (p <0.001).
Most of the patients in group II had deeply preterm infants and the length of their treatment in the second stage of nursing was significantly longer than in group I [81.6 (8.4) vs. 29.5 (6.7) days, respectively] (p <0.001). Accordingly, the financial costs of providing newborn care for infants in group I was several times higher than in group I.
After discharge from the hospital, all newborns were observed at a specialized follow-up office of the Krasnoyarsk Regional Clinical Center for Maternity and Child Care. The most common neonatal complications in newborns were neonatal jaundice (20%), retinopathy (9.2%), grade 2 intraventricular hemorrhage (4.6%), and hypoxic brain injury (6.1 %) (Fig. 2). It should be noted that given a timely diagnosis and adequate treatment, all these complications are currently curable with a relatively favorable prognosis.
Conclusion
The findings of our study demonstrated the superiority of active management with surgical correction over conservative strategy in women with ICI and prolapsed fetal membranes. Simultaneous implementation of a set of techniques described in this article (tight filling of the urinary bladder, transabdominal amnioreduction, using a Foley catheter for cervical cerclage), adequate postoperative drug therapy, and careful follow up enables achieving greater pregnancy prolongation (on the average, 8 weeks longer than in group II), thereby significantly reducing perinatal mortality and morbidity. Besides, active management reduces the financial costs of rehabilitation and treatment of preterm infants due to a significantly lower incidence of neonatal complications and a shorter length of hospital stay.
References
- Rand K.M., Austin N.C., Inder T.E., Bora S., Woodward L.J. Neonatal infection and later neurodevelopmental risk in the very preterm infant. J Pediatr. 2016;170:97-104.
- Delorme P., Goffinet F., Ancel P.Y., Foix-LHélias L., Langer B., Lebeaux C. et al. Cause of preterm birth as a prognostic factor for mortality. Obstet Gynecol. 2016; 127(1): 40-8.
- Артюхов И.П., Цхай В.Б., Капитонов В.Ф., Коновалов В.Н., Роговенко Е.Ю. Семейные и медицинские проблемы, связанные с рождением и выхаживанием детей, родившихся с экстремально низкой массой тела. Сибирскоемедицинскоеобозрение. 2011; 3(69): С.98-103. [Artyukhov I. P., Tskhai V. B., Kapitonov V. F., Konovalov V. N., Of logovenko E. J. Family and medical problems associated with birth and nursing of children born with extremely low birth body weight. Siberian medical review. 2011; 3: 98-103 (in Russian)]
- Costeloe K.L., Hennessy E.M., Haider S., Stacey F., Marlow N., Draper E.S. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ. 2012;345:e7976.
- Jarjour I.T. Neurodevelopmental outcome after extreme prematurity: a review of the literature. Pediatr Neurol. 2015 Feb;52(2):143-52.
- Lagatta J., Andrews B., Caldarelli L., Schreiber M., Plesha-Troyke S., Meadow W. Early neonatal intensive care unit therapy improves predictive power for the outcomes of ventilated extremely low birth weight infants.J Pediatr. 2011;159(3): 384-91. e1.
- Rogers E.E., Hintz S.R. Early neurodevelopmental outcomes of extremely preterm infants. SeminPerinatol. 2016 Dec;40(8):497-509.
- Conde-Agudelo A., Romero R. Predictive accuracy of changes in transvaginal sonographic cervical length over time for preterm birth: a systematic review and metaanalysis. Am J Obstet Gynecol. 2015;213(6):789-801.
- Crane J.M., Hutchens D. Follow-up cervical length in asymptomatic high-risk women and the risk of spontaneous preterm birth.J Perinatol. 2011;31(5):318-23.
- Vandermolen B.I., Hezelgrave N.L., Smout E.M., Abbott D.S., Seed P.T., Shennan A.H. Quantitative fetal fibronectin and cervical length to predict preterm birth in asymptomatic women with previous cervical surgery. Am J Obstet Gynecol. 2016; 215(4): 480.e1-480.
- Хамадьянов У.Р., Саубанова Т.В., Потемкина Е.В. Профилактика невынашивания беременности при истмико-цервикальной недостаточности путем хирургической коррекции методом серкляжа. Российский вестник акушера-гинеколога 2014; 3: 43-6. [Khamaganov W.R., Saubenova T.V.,Potemkina E.V. Prevention of pregnancy in the isthmic-cervical insufficiency, surgical correction by the method of cerclage. Russian Bulletin of obstetrician-gynecologist 2014; 14(3): 43-6 (in Russian)]
- Alfirevic Z., Stampalija T., Roberts D., Jorgensen A.L. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4: CD008991.
- Paules C., Moreno E., Gonzales A., Fabre E., González de Agüero R., Oros D. Amniotic fluid sludge as a marker of intra-amniotic infection and histological chorioamnionitis in cervical insufficiency: a report of four cases and literature review. J Matern Fetal Neonatal Med. 2016;29(16):2681-4.
- Kim C.J., Romero R., Chaemsaithong P., Chaiyasit N., Yoon B.H., Kim Y.M. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015; 213(4 Suppl):S29-52.
- Aoki S., Ohnuma E., Kurasawa K., Okuda M., Takahashi T., Hirahara F. Emergency cerclage versus expectant management for prolapsed fetal membranes: a retrospective, comparative study. J Obstet Gynaecol Res. 2014;40(2):381-6.
- Kuon R.J., Hudalla H., Seitz C., Hertler S., Gawlik S., Fluhr H., Gausepohl H.J., Sohn C., Pöschl J., Maul H. Impaired neonatal outcome after emergency cerclage adds controversy to prolongation of pregnancy. PLoS One. 2015; 10(6): e0129104.
- Беспалова О.Н., Саргсян Г.С. Выбор метода коррекции истмико-цервикальной недостаточности //Журнал акушерства и женских болезней. – 2017. – Т. 66. – № 3. – С. 157–168. [Bespalova O. N., Sargsyan G. S. Choice of method of correction of isthmic-cervical insufficiency. Journal of obstetrics and women's diseases. 2017; 66(3): 157-68]
- Namouz S., Porat.S, Okun N., Windrim R., Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013; 68(5): 379-88.
- Abo-Yaqoub S., Mohammed A.B., Saleh H. The effect of second trimester emergency cervical cerclage on perinatal outcome. J Matern Fetal Neonatal Med. 2012; 25(9): 1746-9.
- Zhu L.Q., Chen H., Chen L.B., Liu Y.L., Tian J.P., Wang Y.H. et al. Effects of emergency cervical cerclage on pregnancy outcome: a retrospective study of 158 cases. Med SciMonit. 2015; 21:1395-401.
- Kanai M., Ashida T., Ohira S., Osada R., Konishi I. A new technique using a rubber balloon in emergency second trimester cerclage for fetal membrane prolapse. J Obstet Gynaecol Res. 2008;34(6):935-40.
Received 17.05.2018
Accepted 22.06.2018
About the Authors
Tskhay, Vitaly B., MD., prof., head of Department of Perinatology, Obstetrics and Gynecology, Medical Faculty, Krasnoyarsk State Medical University namedafter V.F. Voyno-Yasenetsky. 660022, Russia, Krasnoyarsk, P. Zheleznyaka str. 1. Tel.: +79232872134. E-mail: tchai@yandex.ru
Dudina, Anna Yu., assistant of Department of Perinatology, Obstetrics and Gynecology, Medical Faculty, Krasnoyarsk State Medical University named
after V.F. Voyno-Yasenetsky. Obstetrician-gynecologist of Department of Pregnancy Pathology Unit №1. Krasnoyarsk Regional Clinical Center of Maternity and Childhood.
660022, Russia, Krasnoyarsk, P. Zheleznyaka str. 1. Tel.: +79131974868. E-mail: anybar@mail.ru
Kochetova, Elena E., head of Department of Pregnancy Pathology Unit №1.. Krasnoyarsk Regional Clinical Center of Maternity and Childhood.
Adress: 600074, Russia, Krasnoyarsk, Academician Kirensky str. 2A. Tel.: 89059713287. Е-mail: elena.kochetova.64@mail.ru
Lobanova, Tatjana T., head of Department of Ultrasound and Functional diagnostics, Krasnoyarsk Regional Clinical Center of Maternity and Childhood.
600074, Russia, Krasnoyarsk, Academician Kirensky str. 2A. Теl.: +79131974868. E-mail: oufd_pc@pericentr.ru
Reodko, Svetlana V., Obstetrician-gynecologist of Department of Pregnancy Pathology Unit №1. Krasnoyarsk Regional Clinical Center of Maternity and Childhood.
Adress: 600074, Russia, Krasnoyarsk, Academician Kirensky str. 2A. Tel.: 89082007802. E-mail: sv_reodko@mail.ru
Mikhailova, Aleksandra V., Doctor-resident of Department of Perinatology, Obstetrics and Gynecology, Medical Faculty, Krasnoyarsk State Medical University named
after V.F. Voyno-Yasenetsky. Adress: 660022, Russia, Krasnoyarsk, P. Zheleznyaka str. 1. Tel.: +79832958571. E-mail: alexandra11928@gmail.com.
Domracheva, Marina Y., associate professor of Department of Perinatology, Obstetrics and Gynecology, Medical Faculty, Krasnoyarsk State Medical University named
after V.F. Voyno-Yasenetsky. Adress: 660022, Russia, Krasnoyarsk, P. Zheleznyaka str. 1. Tel.: +79082210584. E-mail: m-domracheva@mail.ru
Konovalov, Vyacheslav N., assistant of Department of Perinatology, Obstetrics and Gynecology, Medical Faculty, Krasnoyarsk State Medical University named
after V.F. Voyno-Yasenetsky. 660022, Russia, Krasnoyarsk, P. Zheleznyaka str. 1. Tel.: +79082213361. E- konovalovvn@gmail.com
Bezruk Ekaterina Valerievna, obstetrician-gynecologist of Department of Pregnancy Pathology Unit №1. Krasnoyarsk Regional Clinical Center of Maternity and Childhood. 600074, Russia, Krasnoyarsk, Academician Kirensky str. 2A. Tel.: +79832009848. E-mail: ekbezruk@yandex.ru
Для цитирования: Tskhay V.B., Dudina A.Y., Kochetova E. E., Lobanova T. T., Reodko S.V., Mikhailova A.V., Domracheva M.Y., Konovalov V. N., Bezruk E.V. Comparative analysis of surgical and conservative treatment of pregnant women with cervical incompetence in case of amniotic sac prolapse. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (6):63-9 (in Russian)
https://dx.doi.org/10.18565/aig.2019.6.63-69