Role of obesity and overweight in preeclampsia
Objective: To investigate the effect of excess body weight and obesity on preeclampsia and to compare the results with the outcomes of extended first-trimester prenatal screening.Savelyeva I.V., Bukharova E.A., Nosova N.V., Prodanchuk E.G., Tsygankova O.Yu., Kuklina L.V.
Materials and methods: The study enrolled 155 patients who were divided into Group I (n=42) and Group II (n=63) with moderate and severe preeclampsia, respectively. Group III (control group) included 50 women with healthy pregnancy. Baseline evaluation included physical, ultrasonic, and biochemical examinations as part of the combined extended prenatal screening according to Russian Health Ministry Order 1130n. Correlation analysis was performed using Gamma (Gamma, G) and Spearman (R) coefficients.
Results: Overweight and obesity were found to be risk factors for gestational complications. These findings do not agree with the results of combined prenatal screening. The results of the first-trimester screening showed that 12 (11.4%) of patients in Groups I and II and five (10%) in the control group had a high risk of preeclampsia with a probability of 1:100 or higher. Correlation analysis showed a moderate association between pre-pregnancy body mass index and the development of preeclampsia during pregnancy (G=0.23, p=0.0015).
Conclusion: The results of the study confirm the relationship between preeclampsia and pre-pregnancy excess body weight. Excess body weight and obesity should be classified as adverse factors that exacerbate the course and outcome of pregnancy and require 100% preventive measures regardless of the results of the first-trimester screening.
Keywords
Obesity is one of the biggest public health problems worldwide [1]. Currently, there is an increase in the incidence of obesity among women of reproductive age [2]. The growing prevalence of the obesity epidemic of the disease has led to the XXI century [3, 4]. According to the WHO, 25% of women of childbearing age are overweight and up to 32% suffer from obesity, and the prevalence of this disease does not today have a decreasing trend [5–7]. Increased body weight in women before pregnancy is one of the most important causes of maternal and perinatal morbidity and mortality [8, 9]. Pregnant women who are obese are at risk for gestational complications, including preeclampsia and eclampsia. Therefore, this patient population has an increased risk of maternal and perinatal morbidity and mortality [10–12].
At the same time, hypertensive pregnancy complications are the fourth leading cause of maternal mortality [13]. To improve maternal and perinatal outcomes, women at high risk of preeclampsia undergo extended combined prenatal screening in the first trimester at 11–14 weeks of gestation as part of the routine screening of pregnant women. The Astraia software automatically predicts the development of early and late preeclampsia.
Considering obesity is the biggest public health problem associated with maternal and perinatal morbidity and mortality, and hypertensive disorders, this study aimed to investigate the effect of excess body weight and obesity on preeclampsia and to compare the results with the outcomes of extended first-trimester prenatal screening.
Materials and methods
The study enrolled 155 patients who were divided into Group I (n=42) with moderate and Group II (n=63) with severe preeclampsia. Group III (control group) included 50 women with healthy pregnancy.
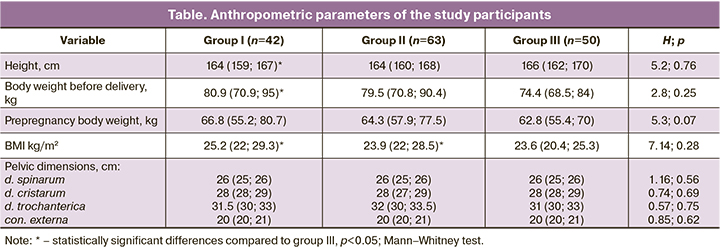
Each group was divided into subgroups according to preconception body mass index (BMI). Subgroup A included women with excess body weight (BMI 25–29.9 kg/m2), subgroup B with obesity (BMI≥30 kg/m2), and subgroup C with low or normal body weight (BMI≤24.9 kg/m2). BMI was calculated using the Ketle index (body mass index=weight (kg)/height (m)2). The study was reviewed and approved by the Ethics Committee of Omsk State Medical University (Ref. No: 97, dated 12.10.2017).
Patients with multiple and Rh-alloimmunized pregnancies, decompensation of extragenital diseases, and IVF pregnancies were excluded from the study.
Baseline clinical evaluation included medical history taking, determination of BMI, waist circumference (WC), hip circumference (HC), WC/HC ratio, blood pressure (BP), and laboratory tests (complete blood count and blood chemistry tests with the determination of lipid profile and plasma glucose levels). All patients underwent the full range of physical, ultrasound, and biochemical examinations as part of a combined extended prenatal screening according to Order 1130n of the Ministry of Health of the Russian Federation [14]. The ultrasound examination was performed using a Voluson 8 diagnostic ultrasound machine in accordance with the protocol of Fetal Medicine Foundation [15].
Statistical analysis
Statistical analysis was performed using the Statistica 10.0 Rus software package. The critical level of significance was considered at p<0.05. The normality of the distribution was tested by the Shapiro–Wilk test. Normally distributed continuous variables were expressed as means (M) and standard deviation (SD) and compared with a Student’s t test. Variables not meeting normality assumptions were reported as the median (Me) and interquartile range (Q1; Q3) and compared with a nonparametric Mann-Whitney test. Categorical variables were compared with the chi-square (χ2) test; for correlation analysis, we calculated Gamma correlation coefficient, taking into account a large number of repeated values.
Results and discussion
We analyzed 155 medical records of pregnant women aged 16 to 41 years. The results of the first-trimester screening showed that 12 (11.4%) of patients in Groups I and II and five (10%) in the control group had a high risk of preeclampsia with a probability of 1:100 or higher. The groups were comparable in age, but the BMI in group III was 6.3% lower (p=0.01, Mann–Whitney test) compared to group II and 1.3% lower compared with group I (p=0.04 Mann–Whitney test). The division into subgroups (Table, Fig. 1) showed that women with normal body weight predominated in the control (III) group, their proportion was 22.2% (p=0.02, χ2 test) lower in Group I and 33.3% (p=0.07, χ2 test) lower in Group II. The proportion of obese patients was equal in the preeclampsia groups and 2.4 times (p=0.12, χ2 test) higher than in the control group. There was a moderate correlation between elevated prepregnancy BMI and the development of preeclampsia (G=0.26, p=0.02).
All patients with obesity, 92.5% of overweight women and 72.5% of normal weight or underweight women had nonobstetric comorbidities (Fig. 2).
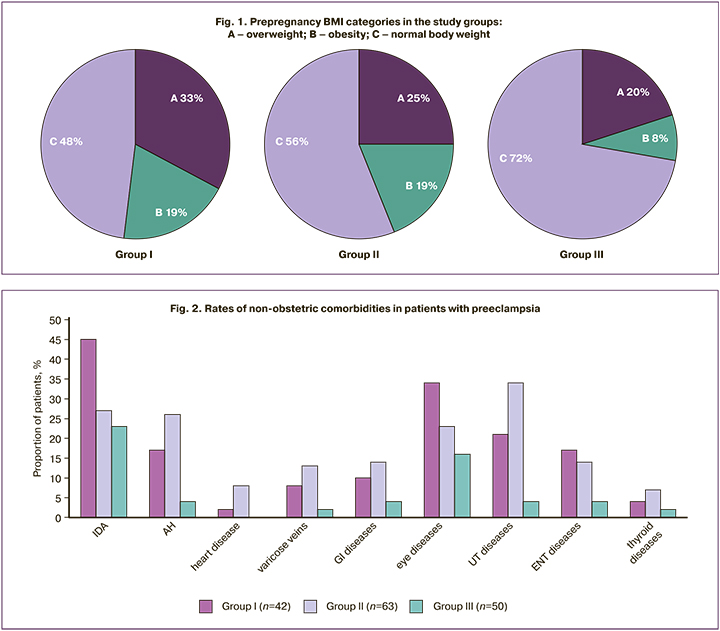
These results were confirmed by correlation analysis showing moderate correlation between body weight and the presence of extragenital pathology (G=0.70, p<0.001). There was also a moderate correlation between comorbidity rate and the occurrence of preeclampsia during pregnancy (G=0.57, p<0.001).
We identified a correlation between the features of obstetric history in the pregnant women of the study groups. There were 48.8% (p=0.02, χ2 test) and 25.6% (p=0.19, χ2 test) more primiparas in Groups I and II, respectively, than in the control group, which was confirmed by the correlation analysis data on the presence of moderate association between the development of preeclampsia and the number of births (G=0.30, p=0.001). Primiparas had a higher risk of developing preeclampsia, which is consistent with the literature [16, 17].
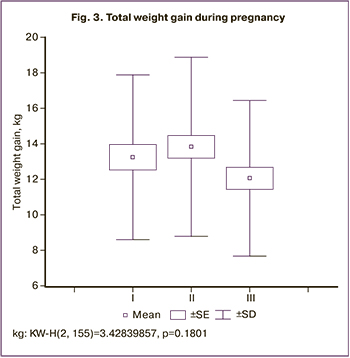
The main pregnancy complication in all groups was abnormal weight gain. Body weight gain during follow-up ranged from 3.4 to 24 kg (mean 13.2±4.6 kg) in Group I, from 2 to 30 kg (mean 13.8±5.0 kg) in Group II, and from 3 to 22 kg (mean 12.1±4.4 kg) in Group III. The correlation analysis revealed a moderate association between weight gain and preeclampsia during pregnancy (G=0.23, p=0.002). Thus, total weight gain was 9.1% (p=0.21, Student's t-test) higher in patients with moderate preeclampsia and 14% (p=0.07, Student's t-test) higher in those with severe preeclampsia compared to the control group (Fig. 3).
Women in the control group gave birth at 37–41 weeks. In Groups I and II, a third of the patients delivered preterm (33.3% in Group I and 38.1% in Group II) at 29–36 weeks gestation. Furthermore, there was a moderate correlation between the development of preeclampsia and gestational age at delivery (G=0.57, p<0.001). The overwhelming majority of pregnant women in Groups I and II were delivered surgically (83.3% and 96.8%). The reason for surgical delivery in all cases was poor general condition. In the control group, 38% of the patients underwent surgical delivery, which was 54.4% less frequent compared to Group I (p<0.001, χ2 test) and 60.7% compared to Group II (p<0.001, χ2 test).
Therefore, the course of pregnancy and birth outcomes differed significantly in pregnant women with excess body weight and obesity relative to those with normal body weight, primarily due to the onset of preeclampsia.
Conclusion
Our study confirmed the evidence that overweight and obesity can have an adverse effect on the course and outcome of pregnancy and delivery. Elevated prepregnancy BMI is associated with increased risk of preeclampsia. According to the results of the combined extended prenatal screening in the first trimester, obese and overweight patients constituted a high-risk group in only 11.4% of pregnant women. Our findings show a significantly higher risk of preeclampsia in this category of patients. This may serve as a development for additional approaches to the management of pregnant women and a customized childbirth strategy depending on the degree of fat metabolism abnormality. Further work in this direction will reduce the rate of pregnancy complications and improve obstetric and perinatal outcomes.
References
- ACOG Practice Bulletin No. 202: Gestational hypertension and preeclampsia. Obstet. Gynecol. 2019; 133(1): e1-25. https://dx.doi.org/10.1097/AOG.0000000000003018.
- Bianchi V.E. Weight loss is a critical factor to reduce inflammation. Clin. Nutr. ESPEN. 2018; 28: 21-35. https://dx.doi.org/10.1016/j.clnesp.2018.08.007.
- Yu L., Li Y., Du C., Zhao W., Zhang H., Yang Y. et al. Pattern recognition receptor-mediated chronic inflammation in the development and progression of obesity related metabolic diseases. Mediators Inflamm. 2019; 2019: 5271295. https://dx.doi.org/10.1155/2019/5271295.
- Диагностика, лечение, профилактика ожирения и ассоциированных с ним заболеваний. Национальные клинические рекомендации. СПб.; 2017: 7-10. [Diagnosis, treatment, prevention of obesity and associated diseases. National Clinical Guidelines. St. Petersburg.; 2017: 7-10 (in Russian)].
- Domokos G. Hyperglycemia-induced endothelial dysfunction. In: Endothelial dysfunction – old concepts and new challenge. Intechopen; 2018: 179-210. 10.5772/intechopen.68656.
- Echeverria C., Eltit F., Santibanez J.F., Gatica S., Cabello-Verrugio C., Simon F. Endothelial dysfunction in pregnancy metabolic disorders. Biochim. Biophys. Acta Mol. Basis Dis. 2020; 1866(2): 165414. https://dx.doi.org/10.1016/j.bbadis.2019.02.009.
- World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFRA, World Bank Group and the United Nations Population Division: executive summary. WHO; 2019. Available at: https://apps.who.int/iris/handle/10665/327596.
- Ottanelli S., Napoli A., Clemenza S., Mecacci F., Lapolla A., Metzger B.E. Hypertension and preeclampsia in pregnancy complicated by diabetes. Gestational diabetes. A Decade after the HAPO Study. Front. Diabetes. 2020; 28: 171-82. https://dx.doi.org/10.1159/000480173.
- Yonekura Collier A.R., Zsengeller Z., Pernicone E., Salahuddin S., Khankin E.V., Karumanchi S.A. Placental sFLT1 is associated with complement activation and syncytiotrophoblast damage in preeclampsia. Hypertens. Pregnancy. 2019; 38(3): 193-9. https://dx.doi.org/10.1080/10641955.2019.1640725.
- Дубровина С.О., Муцалханова Ю.С., Васильева В.В. Ранние предикторы преэклампсии. Акушерство и гинекология. 2018; 10: 47-51. [Dubrovina S.O., Mutsalkhanova Yu.S., Vasilyeva V.V. Early predictors of preeclampsia. Obstetrics and Gynecology. 2018; 10: 47-51. (in Russian)]. https://dx.doi.org/10.18565/aig.2018.10.47-51.
- Липатов И.С., Тезиков Ю.В., Азаматов А.Р., Шмаков Р.Г. Общность клинических проявлений преэклампсии и метаболического синдрома: поиск обоснования. Акушерство и гинекология. 2021; 3: 81-9. [Lipatov I.S., Tezikov Yu.V., Azamatov A.R., Shmakov R.G. The commonality of clinical manifestations of preeclampsia and metabolic syndrome: the search for justification. Obstetrics and Gynecology. 2021; 3: 81-9. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.3.81-89.
- Нагоев Т.М., Муминова К.Т., Ходжаева З.С., Холин А.М., Зиганшина М.М., Козлова А.А., Мартиросян Я.О. Материнская гемодинамика и преэклампсия. Акушерство и гинекология. 2020; 1: 5-11. [Nagoev T.M., Muminova K.T., Khodzhaeva Z.S., Kholin A.M., Ziganshina M.M., Kozlova A.A., Martirosyan Ya.O. Maternal hemodynamics and preeclampsia. Obstetrics and Gynecology. 2020; 1: 5-11. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.1.5-11.
- Преэклампсия. Эклампсия. Отеки, протеинурия и гипертензивные расстройства во время беременности, в родах и послеродовом периоде. Клинические рекомендации. М.; 2021. [Preeclampsia. Eclampsia. Edema, proteinuria and hypertensive disorders during pregnancy, childbirth and the postpartum period. Clinical recommendations. M.; 2021 (in Russian)].
- Приказ Минздрава России от 20.10.2020 №1130н Об утверждении Порядка оказания медицинской помощи по профилю акушерство и гинекология (зарегистрировано в Минюсте России 12.11.2020 № 60869) [Order of the Ministry of Health of the Russian Federation dated 20.10.2020 N 1130n On approval of the Procedure for providing medical care in the profile of obstetrics and Gynecology (Registered with the Ministry of Justice of the Russian Federation on 12.11.2020 N 60869) (in Russian)].
- The Fetal Medicine Foundation. Protocol for measurement of uterine artery pulsatility index. Available at: https://fetalmedicine.org/research/assess/preeclampsia/background
- Ходжаева З.С., Тимошина И.В., Дегтярева Е.И., Снеткова Н.В., Потапова А.А. Влияние ожирения и чрезмерной прибавки массы тела на исходы родов. Акушерство и гинекология. 2018; 9: 62-6. [Khodzhaeva Z.S., Timoshina I.V., Degtyareva E.I., Snetkova N.V., Potapova A.A. Impact of obesity and excessive gestational weight gain on birth outcomes. Obstetrics and Gynecology. 2018; 9: 62-6 (in Russian)]. https://dx.doi.org/10.18565/aig.2018.9.62-66.
- Шалина Р.И., Касум-заде Н.К., Коноплянников А.Г., Латышкевич О.А., Шеховцов Д.Б. Прогнозирование и профилактика преэклампсии в условиях городского центра планирования семьи и репродукции. Акушерство и гинекология. 2020; 7: 61-70. [Shalina R.I., Kasum-zade N.K., Konoplyannikov A.G., Latyshkevich O.A., Shekhovtsov D.B. Prediction and prevention of preeclampsia in the city Center for family planning and reproduction. Obstetrics and Gynecology. 2020; 7: 61-70. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.7.61-70.
Received 10.03.2022
Accepted 20.04.2022
About the Authors
Irina V. Savelyeva, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia, +7(913)654-35-77, saveljeva_iv_omsk@mail.ru, https://orcid.org/0000-0001-9342-7342, 644099, Russia, Omsk, Lenina str., 12.Elena A. Bukharova, Teaching Assistant at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia,
+7(913)661-98-88, buxarova88@mail.ru, https://orcid.org/0000-0002-6093-3721, 644099, Russia, Omsk, Lenina str., 12.
Natalya V. Nosova, Teaching Assistant at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia,
+7(951)417-44-52, natalya-nosova-85@mail.ru, https://orcid.org/0000-0002-2362-5367, 644099, Russia, Omsk, Lenina str., 12.
Eugene G. Prodanchuk, PhD, Associate Professor at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia, +7(913)973-50-33, ompeg@mail.ru, https://orcid.org/0000-0003-4498-5836, 644099, Russia, Omsk, Lenina str., 12.
Olga Yu. Tsygankova, PhD, Associate Professor at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia, +7(913)964-97-22, olts74@mail.ru, https://orcid.org/0000-0002-3553-055X, 644099, Russia, Omsk, Lenina str., 12.
Larisa V. Kuklina, PhD, Associate Professor at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia,
+7(908)103-22-22, kuklinalara@mail.ru, https://orcid.org/0000-0002-1496-6450, 644099, Russia, Omsk, Lenin str., 12.
Сorresponding author: Irina V. Savelyeva, saveljeva_iv_omsk@mail.ru
Authors' contributions: Savelyeva I.V. – concept and design of the study, manuscript editing; Bukharova E.A., Nosova N.V., Prodanchuk E.G., Tsygankova O.Yu., Kuklina L.V. – data collection and processing, statistical analysis, manuscript drafting.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Ethics Committee of Omsk State Medical University
(Ref. No: 97 dated 12.10.2017).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Savelyeva I.V., Bukharova E.A., Nosova N.V., Prodanchuk E.G.,
Tsygankova O.Yu., Kuklina L.V. Role of obesity and overweight in preeclampsia.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 5: 59-64 (in Russian)
https://dx.doi.org/10.18565/aig.2022.5.59-64