Surgical treatment results for high rectovaginal fistulas using invagination technique
Background. Rectovaginal fistula (RVF) is a rare type of malformation. Rectovaginal fistulas represent 5% of all anorectal fistulas. The results of surgical treatment are disappointing, and disease recurrence is in 20–80% of cases.Mudrov A.A., Krasnopolsky V.I., Popov A.A., Titov A.Yu., Fomenko O.Yu., Blagodarny L.A., Kostarev I.V., Sokolova Yu.A., Omarova M.M., Shelygin Yu.A.
Aim. Assessment of the efficacy of invagination technique.
Materials and methods. The study included 57 women with high RVFs aged 20–73 years. The mean age of the patients was 34 years. The causes of RVFs were: inflammatory diseases in 11 women (19,3%); obstetric injury – in 29 (51%); pelvic surgery – in 12 (21%); and RVFs due to other causes – in 5 (8,8%) women. 33 (57,8%) patients previously underwent surgical tratment. Diverting stomas were previously formed in 11 cases (19,2%).
Results. Surgical treatment using invagination technique was performed in all patients. The mean follow-up period was 23,2 months. Successful treatment of patients was in 63.2% of cases, and no postoperative complications were registered.
Conclusion. The invagination technique is an effective and safe method for treatment of high rectovaginal fistulas. In most cases application of this technique is possible without performing preventive colostomy.
Keywords
Rectovaginal fistula (RVF) is a socially significant medical condition that, does not pose an immediate danger to life, but sharply worsens its quality. At the same time, given that the most common cause of formation of a pathological anastomosis between the rectum and the vagina is birth trauma, the main contingent of patients is young women of fertile age. [1]. All over the world, RVFs are detected in 2–3 million women, and their proportion in the structure of rectal fistulas is at least 5% [2, 3].
Over a 100-year history of RVF treatment, more than a hundred different methods and techniques for the surgical treatment have been proposed. However, the recurrence rate of RVF is still 20–80% [4–6].
Among the numerous methods of treatment, we drew attention to the invagination technique to eliminate high RVF. For the first time a similar method was proposed by F. Koenig in 1903 for treatment of rectal fistulas [7]; in 1918, it was subsequently modified for rectovaginal anastomoses by R. Futh [8]. Further, there are only few published works (no more than 16), that mainly presented the clinical observations [9]. A large group of patients with RVF, who underwent surgery using the inverted technique was studied by B.A. Agaev [10].
This study presents the immediate and long-term results of application of the invagination technique for high RVF correction modified by the National Medical Research Center of Coloproctology (patent for the invention No. 2675351 of 18.12.2018) [11].
Materials and methods
From September, 2015 to March, 2019 the invagination technique for surgical correction of high RVFs in 57 patients was used in the National Medical Research Center of Coloproctology named after A. N. Ryzhikh of the Ministry of Health of Russia, Moscow, Russia. The inclusion criterion was the presence of high RVF. The exclusion criteria were: RVFs with opening located below the dentate line or 7–8 cm above it; RVFs after beam radiation therapy; the patients with a pronounced inflammatory process and purulent leaks in the rectovaginal septum; rectovaginal septal defects more than 2.5 cm in diameter; somatic diseases at the stage of decompensation; mental disorders; severe inflammatory bowel disease.
The decision to include the patients in the study (determination of inclusion/exclusion criteria) was made after a standard examination, which included collection of past medical history and case history; collection of obstetrical and gynecological anamnesis; clinical and instrumental examination (visual examination, vaginal examination and palpation, bimanual examination, transrectal ultraso und scan, sphincterometry, colonoscopy, proctography).
Statistical analysis
Descriptive statistics were presented in format M (SD), where M is a sample mean (arithmetic mean), SD (standard deviation); and in format Me (Q1; Q3) – the median (Me) and quartiles first (Q1) and third (Q3) for quantitative data with a distribution that differed from normal.
The Shapiro–Wilk test was used to check the normality of distribution including the residuals in the regression equations.
To determine the statistical significance of the differences between the studied groups of patients considering the dependence of the groups in the dynamic study, when the same objects were studied at different time, paired Wilcoxon test for a distribution different from normal and paired Student's t-test for normal distribution were used.
In this study, the significance level was 5% to determine the significance differences at p <0.05.
Results
57 patients included in the study underwent surgery using invagination technique, which was modified by the National Medical Research Center of Coloproctology [10]. There were no intraoperative complications.
Descriptive statistics is presented in Tables 1–6.
The age of patients was 20–73 years. The patients were predominantly young women (Table 1).
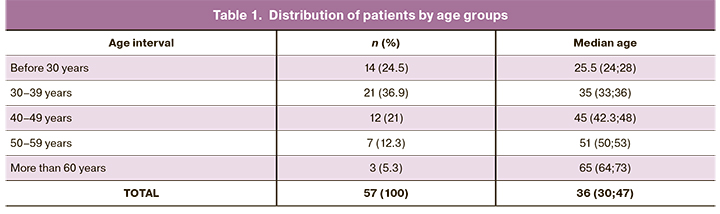
Within the age intervals, due to the small number of observations, the distributions were abnormal.
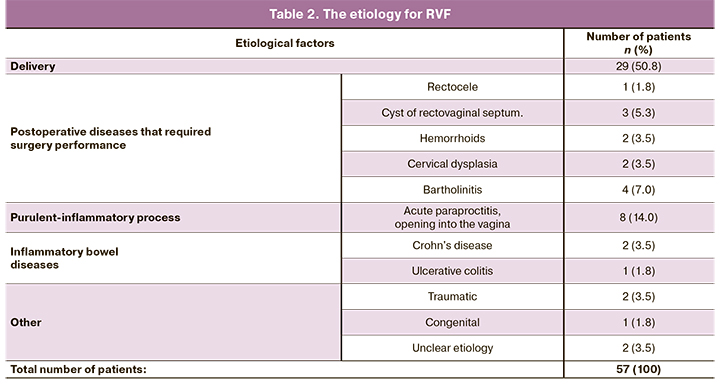
The most common cause of RVF was delivery-related injury in 29 (51%) patients (Table 2).
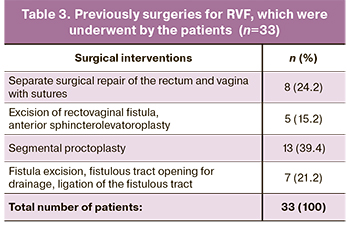
Previously, 33 (57.9%) patients underwent surgery for RVF in other medical institutions, i.e. the condition was recurrent; 13 (22.8%) of them underwent 2 or more surgeries, 11 (19.3%) patients underwent colostomy formation (Table 3).
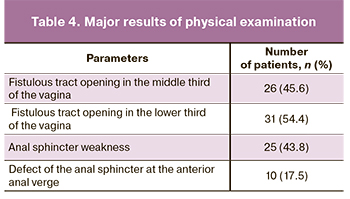
Physical examination was focused on the diameter and location of fistulous tract openings in the rectum and vagina, the presence of inflammatory-infiltrative changes in the rectovaginal septum, and the state of the anal sphincter tone and the levator ani muscles were assessed (Table 4).
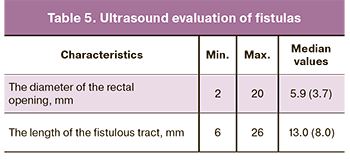
According to the ultrasound measurements, the diameter of the fistulous opening ranged from 2 to 20 mm, and was on average approximately 6 mm. The length of the fistulous tract ranged from 6 to 26 mm, and was on average 13 mm (Table 5). It should be noted that the values for the diameter and length of the fistulous tract were normally distributed (p <0.001).
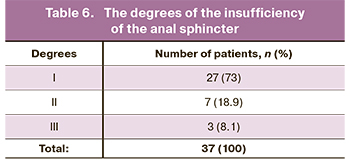
Given the partial or total leaking of intestinal contents through the vagina in patients with RVF, it was practically impossible to assess the changes in the function of the rectal obturator apparatus using subjective methods and scales, however, sphincterometry allowed us to identify the insufficiency of the anal sphincter in 37 (64.9%) patients: the first-degree insufficiency of the anal sphincter was in 27 women; the second-degree insufficiency was in 7 women; and the third-degree insufficiency was in 3 women (Table 6) [12].
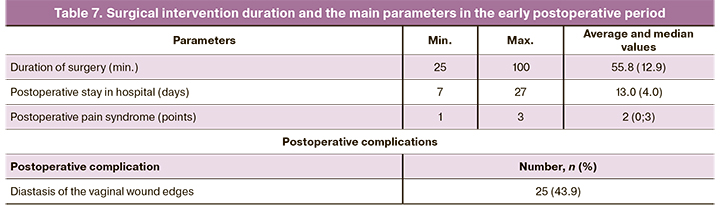
The time of surgery varied from 25 to 200 minutes, on average 55.8 (12.9) minutes, the distribution was normal (р=0.04).
The only complication in the early postoperative period was diastasis of the vaginal wound edges, which occurred in 25 (43.9%) patients; at the same time, gas and intestinal contents were discharged from the vagina in 9 (36.0%) women in the early postoperative period. In 3 (12.0%) cases of diastasis of the vaginal wound edges, disinvagination of the fistulous track into the vaginal lumen was performed.
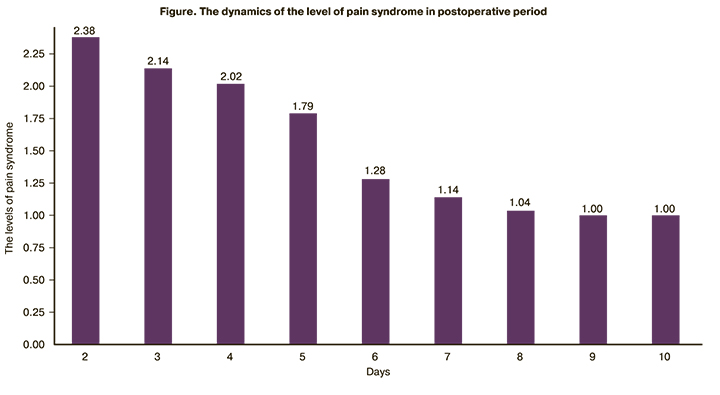
Despite diastasis of the vaginal wound edges, pain syndrome intensity on a scale of 0–10 points (the visual analogue scale) did not exceed 3 points in 43.9% of patients during all observations in the postoperative period (Figure).
The length of patients’ hospital stay was 7–27 days, on average 13.0 (4.0) days, the distribution was normal (р<0.001) (Table 7).
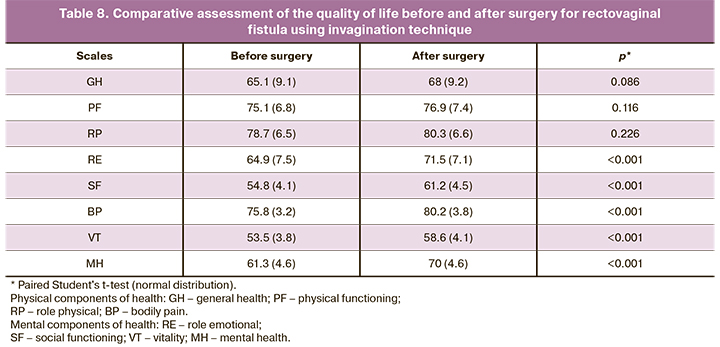
After surgery, the follow-up period ranged from 5 to 56 months, on average 23.2 (Me=18) months; the distribution was normal (p=0.002). Recurrence of the medical condition after using the invagination technique was detected in 21 (36.8%) patients. At the same time in 15 of them, the diameter of the fistulous opening significantly decreased (in 6 cases, a 1–2 mm decrease led to a complete reduction in clinical manifestations). Considering this, 3 months after surgery, a significant improvement in the quality of life was noted in 51 (89.5%) patients. Assessment of the quality of life (QOL) using the SF-36 Questionnary measuring 8 scales showed the improvement in physical components of health (Table 8).
Assessment of the function of the rectal obturator apparatus using sphincterometry, which was performed 3–6 months after application of the invagination technique showed that, there were practically no changes in comparison with the initial data (the differences were insignificant and were at the lower limits of normal values, i.e. the same as they were before surgery). The average anal pressure values were abnormally distributed both before and after surgery. The median anal pressure at rest was 37.5 (34.8; 41.8) mm Hg before surgery; the maximum pressure generated by contraction was 118.5 (91.5; 138) mm Hg. After surgical treatment, the median resting pressure was 37 (34; 40) mm Hg; the maximum pressure generated by contraction was 106.5 (89; 129) mm Hg (Table 9).
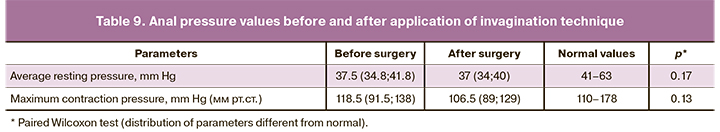
Preservation of the rectal obturator apparatus functioning after surgery was an objective evidence that invagination is a safety and minimally traumatic method.
Taking into account the overall regression of clinical manifestations, 6 of 21 patients with the recurrent disease refused further surgical treatment. In the period between 7–14 months, 15/21 women underwent repeated surgery. Of them, 9 patients underwent repeated surgery using invagination technique, among them 5 patients recovered; in 5/15 women the rectal and vaginal advancement flap repair was performed; 2 women recovered; in 1/15 case, the fistulous openings were successfully sutured separately in the rectum and vagina.
Thus, sequential multistage treatment of RVFs made it possible to cure 77.2% of patients.
Conclusion
The study showed that the invagination technique for surgical repair of RVFs is the operation of choice for the patients with high RVF. A low number of postoperative complications, low level of pain syndrome in the postoperative period, and the absence of a damaging effect on the rectal obturator apparatus prove that this method of treatment is safe. The invagination technique remains relevant in case of recurrent medical condition, and the use of this technique in 9/21 patients with recurrent condition has proven the possibility of repeated invagination. Thus, the invagination technique has been shown to be consistent and effective not only as a method for treatment of high rectovaginal fistulas, but also as a full-fledged link in the chain of multistage tactics for RVFs correction.
References
- Vogel J.D., Johnson E.K., Morris A.M., Paquette I.M., Saclarides T.J., Feingold D.L., Steele S.R. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis. Colon Rectum. 2016; 59(12): 1117-33. https://dx.doi.org/10.1097/DCR.0000000000000733.
- Abu-Gazala M., Wexner S.D. Management of rectovaginal fistulas and patient outcome. Expert Rev. Gastroenterol. Hepatol. 2017; 11(5): 461-71. https://dx.doi.org/10.1080/17474124.2017.1296355.
- Byamugisha J., El Ayadi A., Obore S., Mwanje H., Kakaire O., Barageine J. et al. Beyond repair – family and community reintegration after obstetric fistula surgery: study protocol. Reprod. Health. 2015; 18(12): 115. https://dx.doi.org/10.1186/s12978-015-0100-1.
- Göttgens K., Smeets R., Stassen L., Beets G., Breukink S.O. The disappointing quality of published studies on operative techniques for rectovaginal fistulas: a blueprint for a prospective multi-institutional study. Dis. Colon Rectum. 2014; 57(7): 888-98. https://dx.doi.org/10.1097/DCR.0000000000000147.
- Trompetto M., Luc R.A., Novelli E., Tutino R., Clerico G., Gallo G. Use of the Martius advancement flap for low rectovaginal fistulas. Colorectal Dis. 2019; 21(12): 1421-8. https://dx.doi.org/10.1111/codi.14748.
- Шелыгин Ю.А., ред. Клинические рекомендации. Колопроктология. М.: ГЭОТАР-Медиа; 2015: 108-25. [Shelygin Yu.A., eds. Clinical recommendations. Coloproctology. M.: GEOTAR-Media, 2015: 108-25. (in Russian)].
- Koenig F. Ueber Einstülpungsmethode bei der Operation der Fistula colli congenita und die gelegentliche Auwendung bei einer Mastdarmfistel. Arch. Klin. Chir. 1905; 70: 1008.
- Füth H. Zur Operation der Blasen-scheidenfistel. Arch. Gynäk. 1918; 109: 488-9.
- Аминев А.М. Руководство по проктологии. Куйбышев: «Волжская Коммуна»; 1973; 3: 368-87. [Aminev A.M. Guidance on proctology. Kuibyshev. Publishing house "Volga Commune." 1973; 3: 368-87. (in Russian)].
- Агаев Б.А., Джавадов Э.А., Аббасова Г.А. Хирургическое лечение средних и нижних ректовагинальных свищей методом инвертации. Хирургия. Журнал им. Н.И. Пирогова. 2010; 2: 44-6. [Agaev B.A., Dzhavadov E.A., Abbasova G.A. Surgical treatment of middle and lower rectovaginal fistulas by the method of inversion. Surgery. Journal named after N.I. Pirogov. 2010; 2: 44-6. (in Russian)].
- Мудров А.А., Шелыгин Ю.А., Титов А.Ю., Фоменко О.Ю., Благодарный Л.А., Соколова Ю.А., Костарев И.В., Омарова М.М. Малоинвазивный подход при лечении ректовагинальных свищей высокого уровня (первый опыт применения «инвагинационного» метода). Колопроктология. 2018; 4: 39-44. [Mudrov A.A., Shelygin Yu.A., Titov A.Yu., Fomenko O.Yu., Thankful L.A., Sokolova Yu.A., Kostarev I.V., Omarova M.M. Minimal invasive treatment of high level rectovaginal fistulas (the first experience of invagination method). Coloproctology. 2018; 4(66): 39-44. (in Russian)].
- Шелыгин Ю.А., Фоменко О.Ю., Титов А.Ю., Берсенева Е.А., Мудров А.А., Белоусова С.В. Сфинктерометрическая градация недостаточности анального сфинктера. Колопроктология. 2016; 4: 54-9. [Shelygin Yu.A., Fomenko O.Yu., Titov A.Yu. et al. Sphincterometry gradation of anal sphincter insufficiency. Coloproctology. 2016; 4(58): 54-9. (in Russian)].
Received 10.11.2020
Accepted 07.04.2021
About the Authors
Researcher of the Department of Coloproctology, Russian Medical Academy of Postgraduate Education. E-mail: aa-mudrov@mail.ru.ORCID: 0000-0002-1207-5988. 123423, Russia, Moscow, Salyama Adilya str., 2.
Vladislav I. Krasnopol'skii, M.D., Ph.D., Professor, Academician of RAS, President of Moscow Regional Research Institute of Obstetrics and Gynecology.
E-mail: gyn_endoscopy@mail.ru. ORCID: 0000-0001-7041-9024. 101000, Russia, Moscow, Pokrovka str., 22а.
Aleksandr A. Popov, M.D., Ph.D., Professor, Head of the Endoscopic Surgery of Moscow Regional Research Institute of Obstetrics and Gynecology.
E-mail: gyn_endoscopy@mail.ru. ORCID: 0000-0003-3692-2421. 101000, Russia, Moscow, Pokrovka str., 22а.
Aleksandr Yu. Titov, M.D., Ph.D., Head of the Department of General and Reconstructive Coloproctology, Ryzhikh National Medical Research Center of Coloproctology. E-mail: info@gnck.ru. ORCID: 0000-0002-1636-8075. 123423, Russia, Moscow, Salyama Adilya str., 2.
Oksana Yu. Fomenko, M.D., Ph.D., Head of the Laboratory of clinical pathophysiology, Ryzhikh National Medical Research Center of Coloproctology.
E-mail: oksana671@yandex.ru. ORCID: 0000-0001-9603-6988. 123423, Russia, Moscow, Salyama Adilya str., 2.
Leonid A. Blagodarny, M.D., Ph.D., Professor, Russian Medical Academy of Postgraduate Education. E-mail: rmapo@rmapo.ru. ORCID: 0000-0003-0010-1488.
123242, Russia, Moscow, Barrikadnaya str., 2/1.
Ivan V. Kostarev, M.D., Ph.D., Head of the Department of Minimally Invasive Coloproctology and Pelvic Surgery, Ryzhikh National Medical Research Center
of Coloproctology; Researcher of the Department of Coloproctology, Russian Medical Academy of Postgraduate Education. E-mail: info@gnck.ru.
ORCID: 0000-0002-1778-0571. 123423, Russia, Moscow, Salyama Adilya str., 2.
Yuliya A. Sokolova, doctor, Ryzhikh National Medical Research Center of Coloproctology. E-mail: info@gnck.ru. ORCID: 0000-0002-8715-6803.
123423, Russia, Moscow, Salyama Adilya str., 2.
Mariyam M. Omarova, postgraduate student of the Department of Coloproctology, Russian Medical Academy of Postgraduate Education.
E-mail: rmapo@rmapo.ru. ORCID: 0000-0001-7329-7878. 123242, Russia, Moscow, Barrikadnaya str., 2/1.
Yuri А. Shelygin, M.D., Ph.D., Professor, Academician of RAS, Ryzhikh National Medical Research Center of Coloproctology; Head of the Department of Coloproctology, Russian Medical Academy of Postgraduate Education. E-mail: info@gnck.ru. ORCID: 0000-0002-8480-9362. 123423, Russia, Moscow, Salyama Adilya str., 2.
For citation: Mudrov A.A., Krasnopolsky V.I., Popov A.A., Titov A.Yu., Fomenko O.Yu., Blagodarny L.A., Kostarev I.V., Sokolova Yu.A., Omarova M.M., Shelygin Yu.A. Surgical treatment results for high rectovaginal fistulas using invagination technique.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 5: 128-134 (in Russian)
https://dx.doi.org/10.18565/aig.2021.5.128-134



