Surgical classification of endometriosis revisited
Objective: To propose new approaches to the classification of the disease based on the analysis of 2352 operations of patients with endometriosis performed in the department over 10 years.Chuprynin V.D., Smolnova T.Yu., Melnikov M.V., Buralkina N.A.
Materials and methods: A total of 12125 operations were performed in the surgical department. Surgeries for endometriosis accounted for 19.4% of them (2352/12 125). In 81.9% of cases, endometriosis was the main indication for surgical treatment. The mean age of the patients was 34.1±6.03 years. There were the following forms of the disease: ovarian endometriosis in 13.9% of cases, superficial endometriosis in 49.4% of cases, deep endometriosis with the lesion of the underlying layers of the peritoneum (muscular, submucosal, subperitoneal) in 58.3% of cases, nodular adenomyosis (the size of adenomyotic nodule exceeding 2 cm) in 3.6% of cases.
Results: We proposed a new approach to the classification of endometriosis based on the depth of the lesion and type of surgical technology. The patients with stage 1 (superficial endometrioid heterotopias with a lesion depth not exceeding one layer) amounted to 25.7%; the rate of patients with stage 2 (endometriosis with the lesion of two layers (peritoneum, muscle/abdominal layers of any anatomical structure)) was 43.3%; stage 3 (endometriosis with the lesion of all layers of any anatomical structure, but without organ dysfunction) was noted in 17.2% of cases; stage 4 (endometriosis with the lesion of all layers of any anatomical structure and organ dysfunction) was detected in 7.1% of patients.
Different methods of surgical treatment of endometriosis were applied, depending on the depth of the lesion: coagulation was used in 95% of patients with stage 1 lesion, excision was used only in 5% of cases with peritoneal confluent lesion. The main method of surgical treatment of patients with stage 2 was excision (100%) followed by suturing or coagulation. The clinical picture of the disease was determined not by the number of foci but by the depth of the lesion since the neurovascular unit was involved. The main method of removal of foci in patients with stage 3 (endometriosis of all layers of the organ but without impairment of its function) was excision/resection, and the method of restoring the integrity of the organ/tissue was suturing/anastomosis. In case of damage to all layers and organ dysfunction (stricture, angulation, damage to neighboring organs), the extent of surgical treatment was expanded to resection in 95% and removal of the organ in 5% of cases.
Conclusion: This classification of endometriosis is relevant as the severity of endometriosis is assessed not due to the extension of the lesion but according to its depth. The use of this classification may help to identify the severity of the course of the disease most accurately and to predict further treatment tactics and rehabilitation which can improve reproductive outcomes and quality of life.
Keywords
Endometriosis is a chronic disease characterized by benign proliferation of tissue outside the uterine cavity, similar to the endometrium in the morphological and functional properties [1]. The disease affects 10–15% of reproductive-aged women. In terms of clinical diagnostic and therapeutic criteria, endometriosis is an extremely heterogeneous disease. This fact is confirmed by a large number of different classifications, none of which has been universally recognized.
Multifocal endometriosis lesion accounts for the need to have a reasoned coherent classification which could be unanimously agreed upon main issues, acceptable for new guidelines and extremely simple for a doctor to use in practice.
The analysis of the existing classifications was carried out in 2017 and a new protocol was proposed which included the following issues: forms of endometriosis (superficial, deep infiltrating, adenomyosis, ovarian endometriosis, various forms of extragenital endometriosis), the color of endometrioid heterotopias, the course of the disease, the results of hormonal examination, reproductive plans, previous hormone therapy, etc. [2].
However, after we performed 2352 operations for endometriosis in the Department of General Surgery in the National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia, we came to the conclusion that this protocol and the existing classifications are not complete for systemizing approaches both to surgical treatment and to combined treatment (in combination with medication). Moreover, in some cases it is impossible for a practical doctor to apply them due to their awkwardness.
Therefore, we had the following aim: to provide a practical doctor with a clinical classification of the disease for stratification of the risk for relapses of the disease and further management tactics of reproductive-aged patients, taking into account surgical tactics for the treatment of various forms of endometriosis.
Our approach to classifying (staging) forms of endometriosis is based not on an extensive approach to the analysis of the process (the number of foci, their development and the number of involved organs), but on an intraoperative assessment of the nature of the development of endometriosis foci in depth.
Materials and methods
A total of 12125 operations have been performed in the surgical department over the past 10 years. Surgeries for endometriosis accounted for 19.4% of them (2352/12125). In 81.9% of cases, endometriosis was the main indication for surgical treatment. The mean age of the patients was 34.1 (6.03) years. The distribution of patients by age is shown in Table 1.
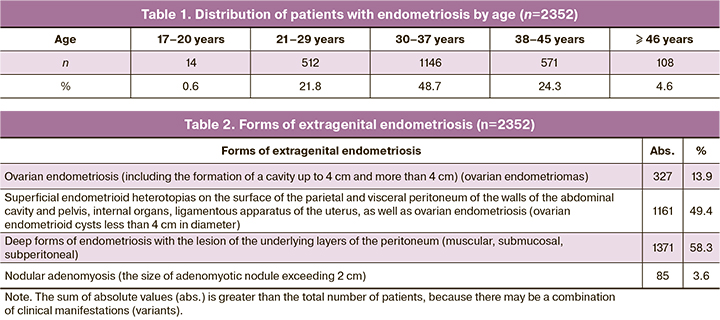
The age group of 30–37 years is predominant in the sample; this prevalence can be explained by the fact that patients with deep infiltrating endometriosis are often admitted to the clinic after multiple surgical interventions for endometriosis, incomplete surgical treatment, as well as due to prolonged infertility. In our study, the clinical manifestations of endometriosis were more severe in older patients (p<0.001).
In the analysis of the results, we considered the existing Russian and foreign classifications, as well as the protocols of the working group on recommendations for surgical treatment of endometriosis [3, 4]. There were the following clinical forms of endometriosis in 2352 patients (Table 2).
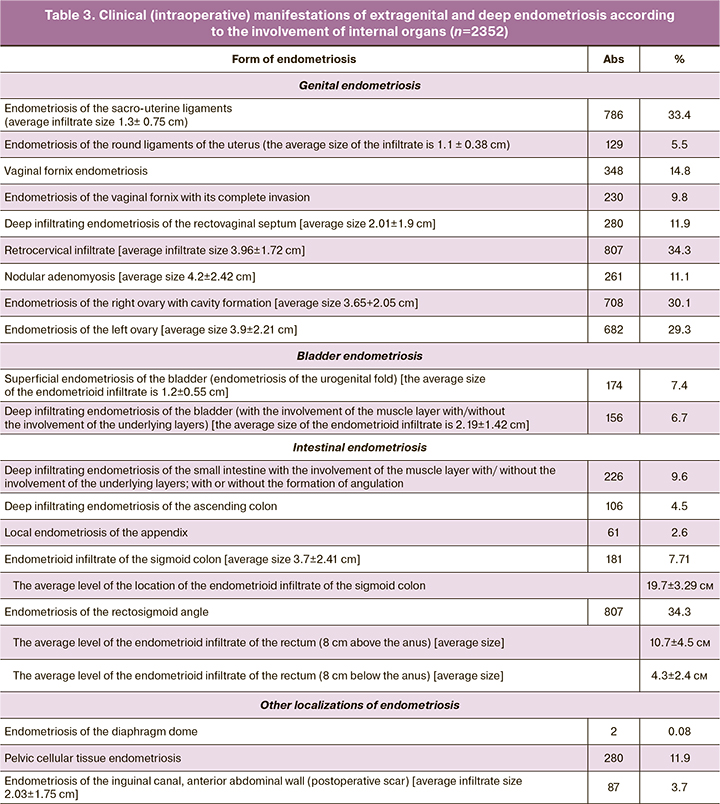
Intraoperative manifestations of extragenital and deep endometriosis are presented in Table 3.
Results
While dealing with patients with endometriosis, we came to the conclusion that the extent of surgical treatment is determined not by the number of foci, but by the size of the focus and its depth. Table 4 shows how the above-mentioned forms of endometriosis were distributed according to the depth of the lesion, regardless of the prevalence of the process, the number of foci and the number of lesions of internal organs and tissues, adhesive process, etc.
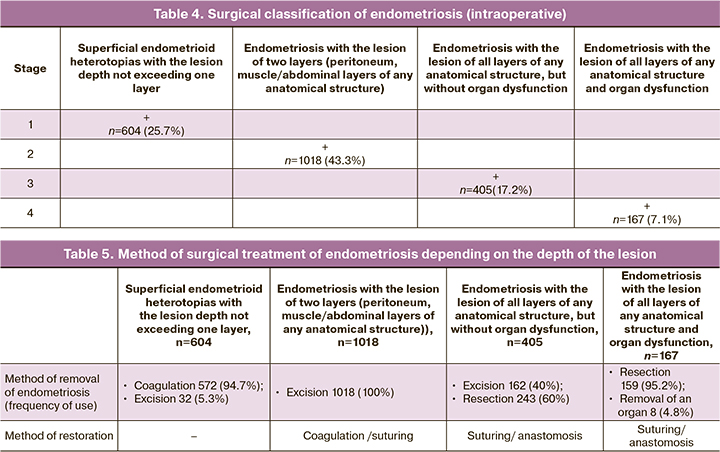
Thus, endometriosis severity was defined as stage 1 regardless of the number of foci in the visceral and parietal peritoneum; this stage was determined by the depth of the lesion. Coagulation which was the main surgical method was used in 95% of patients with stage 1 lesion, excision was used only in 5% of cases with peritoneal confluent lesion (Table 5).
The lesion of two layers (the peritoneum and the underlying layer (the peritoneal tissue or muscles of the hollow organ)) was defined as stage 2 of endometriosis. The main method of surgical treatment of patients with stage 2 was excision (100%) followed by suturing or coagulation.
The clinical picture of the disease was determined not by the number of foci but by the depth of the lesion since the neurovascular unit was involved.
The main method of removal of foci in patients with stage 3 (endometriosis of all layers of the organ but without impairment of its function) was excision/resection, and the method of restoring the integrity of the organ/tissue was suturing/anastomosis (Tables 4, 5).
In case of damage to all layers and organ dysfunction (stricture, angulation, damage to neighboring organs), the extent of surgical treatment was expanded to resection in 95% and removal of the organ in 5% of cases.
This classification is relevant because staging of endometriosis severity clearly reflects both the clinical picture of the disease and the use of a certain method of surgical treatment and extent of surgery (Table 5).
Discussion
All the proposed classifications mainly involve an assessment of endometriosis severity according to the extension (Latin extensivus – expanding, lengthening) of the lesion and taking into account the adhesive process. The severity of the disease was assessed on the basis of the number of foci. In fact, its assessment was based on a principle similar to the evaluation of tumor invasion with staging [5].
The universal classification of A. Acosta et al. (1973) also took into account general surgical forms of endometriosis (for example, “involvement of the urinary tract and/or intestines in the process”) [6]. In addition, the depth of the lesion was not specified, but it is crucial in choosing the method and extent of treatment (coagulation, excision, resection), determining the severity of the disease (as well as the classification of the American Fertility Society (AFS) which was revised later [7, 8]). For example, this classification stated the fact of involvement of the sacro-uterine ligaments in the process (“lesion of the sacro-uterine ligaments and peritoneum of the rectal-uterine space with its obliteration”). However, even complete obliteration of cul-de-sac may be superficial, and the extent of surgical treatment may be limited to incision of adhesions and coagulation of endometriosis foci of the sacro-uterine ligaments, which cannot correspond to the severe form of the disease described in this classification. And on the contrary, infiltration of one sacro-uterine ligament with an endometrioid infiltrate of more than 1–1.5 cm without obliteration of cul-de-sac at the site of the ureter projection can lead to serious consequences and to expansion of the extent including urethrolysis, neoanastomosis, etc. We found that the formation of endometrioid infiltrate of the sacro-uterine ligaments contributed more to the development of hydroureter, compared with endometrioid infiltrations of pelvic cellular tissue. There was a correlation in the frequent combination of infiltration of the sacro-uterine ligament and infiltration of the pelvic tissue. The number of endometrioid foci on the parietal peritoneum is not significant using this approach.
The new classification of the American Society of Fertility (now the American Society of Reproductive Medicine – ASRM) in 1996 did not take into account the depth of invasion either [9].
In 1991, P.R. Koninckx et al. proposed a classification based on the depth of endometriosis lesion, which we consider more appropriate for the selection of treatment tactics [10]. However, this classification included only the posterior pelvic region (components of the recto-uterine pouch) and did not take into account the deep forms of endometriosis of the anterior uterine space, lateral pelvic spaces and the area above the Linii innominate. It is quite possible that P.R. Koninckx considered only “natural” forms of endometriosis. We believe that the development of endometriosis of the round ligaments and vesico-uterine space is greatly influenced by iatrogenic factors. Therefore, deep forms of endometriosis of the vesico-uterine space and round ligaments are not typical for young patients (p=0.035). The role of iatrogenic factors in the development of endometriosis of the vesico-uterine space remains open.
The classification of retrocervical endometriosis (created by L.V. Adamyan, V.I. Kulakov) [11] has the disadvantage in trying to assess the topical sequence (pathological changes) of the development of the disease (from the superficial lesion of the sacro-uterine ligaments to the invasion of the infiltrate into adjacent organs). The classification does not take into account that the localization of the focus of endometriosis can be an independent clinical sign (for example, endometriosis of the rectovaginal septum with or without lesion of the rectal wall with or without the development of obturation syndrome may not manifest as endometriosis of the sacro-uterine ligaments).
We do not quite agree with the classification of ovarian endometriosis suggested by the same authors [11]. We believe that the concept of “staging” in ovarian endometriosis does not accurately reflect the process. For example, the stage transition of superficial endometrioid heterotopias on the surface of one ovary, the parietal peritoneum (stage 1 according to the classification) into endometriotic cysts more than 5–6 cm in diameter of both ovaries (stage 3) is doubtful. In our experience, it is worth evaluating the severity of organ involvement in the process. It is more appropriate to consider ovarian endometriosis with the formation of a cavity up to 3–4 cm in diameter as a variant of superficial endometriosis (stage 1), and one with diameter of more than 5 cm as ovarian endometriosis with the formation of a cavity as stage 2.
This approach is due to the need to use various surgical techniques for the removal of the focus: excision followed by coagulation should be used in the first case, and excision/coagulation and maybe suturing should be performed in the second case. Moreover, an endometrioid ovarian cyst with a diameter of 5–6 cm or more may be isolated, without endometrioid heterotopias of the other ovary and peritoneum in some cases; whereas, ovarian endometriosis up to 3–4 cm, as a rule, is accompanied by the presence of heterotopias of various depth and invasion in various anatomical areas.
The same issue arises with the extent of surgery in nodular adenomyosis. Adenomyotic nodule up to 2–3 cm in diameter (stage 1–2 in our classification) does not affect the method of suturing the myometrial defect after removal of the focus; but removal of adenomyotic nodule of 4 cm or more (stage 2–3) requires careful suturing of the nodular bed which is often accompanied by metroplasty [12].
In our country and in the world is known the classification of common forms of endometriosis by Prof. A.I. Ishchenko [13]. We support the author’s opinion about the presence of superficial forms during peritoneal implantation (stage 1), as well as the formation of infiltrates and adhesive process (stage 2), extraperitoneal organ involvement up to its deformation and obturation of the lumen, including the lesion of the surrounding fiber (stage 3 A–B), etc. This classification is the most acceptable in terms of surgery, as it gives the most accurate understanding of the severity (aggressiveness) of endometriosis. However, the concept of “staging” does not always correctly characterize the process. For example, we could see a deep form of endometriosis without initial superficial forms in 10% of cases. For example, there was an infiltration of the sacro-uterine ligament without the involvement of adjacent organs (their invasion) and without dissemination of endometriosis foci in the peritoneum of the pelvis, the serous cover of the pelvis and peritoneal cavity, etc., but with the infiltration development in the pelvic cellular tissue and the development of urodynamic disorders.
A number of authors [2] note that this classification is difficult to use due to the lack of a scoring system and lack of connection with clinical manifestations of the disease. We believe that a scoring system is not always acceptable. Firstly, endometriosis is not a stage disease, as it was mentioned above. Secondly, the large extensiveness at different depths of the lesion makes it difficult to calculate the score and in some cases it can be impractical (for example, infiltration of the lateral cellular space 3–4 cm in diameter with the involvement of the ureter and multiple superficial heterotopias on the peritoneum of the diaphragm). Besides, according to our experience, deep forms of endometriosis in some cases do not have a clinical picture and the only manifestation in the early stages is infertility; endometrioid infiltrate can be either an intraoperative finding due to another concomitant gynecological pathology or it does not manifest as a pain syndrome and can be revealed only by the appearance of blood in the feces or impaired passage of urine in the later stages of the disease. Moreover, the authors themselves point to the extreme degree of heterogeneity of the clinical course of the disease.
The latest ENZIAN classification of 2016 takes into account topography, the size of the lesion, the symmetry or asymmetry of the lesion [14]. However, the topical points are not entirely clear. For example, “1b–2bb” refers to a lesion of one or both sacro–uterine ligaments with infiltrate sizes up to 1 cm and more than 1 cm, respectively; while “3bb” and “4bb” refer to infiltration of cardinal ligaments without hydronephrosis and with hydronephrosis, respectively.
Anyway, all existing classifications offer an assessment of endometriosis severity on the basis of extension of the lesion including the number of foci, their size, the number of affected organs, the topical location of foci, etc. However, endometriosis severity is determined by the depth of the organ involvement and the extent of surgical intervention; the adhesive process does not always reflect the severity of the course and aggressiveness of the disease. In addition, it may have other causes. Not all classifications take into account the general surgical aspects of lesions of other organs, and, therefore, cannot assess the severity of the disease. Localization of endometriosis focus can be an independent clinical sign, and not a consequence of the stages of the process during the transition from one organ to another. Therefore, it is worth changing the stage of the process to the degree of severity. The scoring system is not always acceptable due to the fact that endometriosis is not a stage disease, and large extensiveness of the lesion at various depth does not give a clear understanding of the severity of the disease. In addition, large extensiveness in combination with various depth of the lesion makes it difficult to count scores and in some cases makes it impractical. It is also necessary to consider that deep forms of endometriosis do not have a clinical picture in some cases.
Conclusion
Thus, this classification based on the assessment of the lesion depth and surgical technology may help to identify the severity of the course of the disease most accurately and to predict further treatment tactics and rehabilitation which can improve reproductive outcomes and quality of life.
References
- Министерство здравоохранения Российской Федерации. Эндометриоз: диагностика, лечение и реабилитация. Клинические рекомендации. М.; 2013. 86c. [Ministry of Health of the Russian Federation. Endometriosis: diagnosis, treatment and rehabilitation. Clinical guidelines. M.; 2013. 86 p.in Russian)].
- Айламазян Э.К., Ярмолинская М.И., Молотков А.С., Цицкарава Д.З. Классификации эндометриоза. Журнал акушерства и женских болезней. 2017; 66(2): 77-92. [Aylamazyan E.K., Yarmolinskaya M.I., Molotkov A.S., Tsitskarava D.Z. Classifications of endometriosis. Journal of Obstetrics and Women’s Diseases. 2017; 66(2): 77-92. (in Russian)].https://dx.doi.org/10.17816/JOWD66277-92.
- Saridogan E., Becker C.M., Feki A., Grimbizis G.F., Hummelshoj L., Keckstein J. et al.; Working group of ESGE, ESHRE and WES. Recommendations for the surgical treatment of endometriosis. Part 1: Ovarian endometrioma. Hum. Reprod. Open. 2017; 2017(4): hox016. https://dx.doi.org/10.1093/hropen/hox016.
- Keckstein J., Becker C.M., Canis M., Feki A., Grimbizis G.F., Hummelshoj L. et al.; Working Group of ESGE, ESHRE, and WES. Recommendations for the surgical treatment of endometriosis. Part 2: deep endometriosis. Hum. Reprod. Open. 2020; 2020(1): hoaa002. https://dx.doi.org/10.1093/hropen/hoaa002.
- Beecham C.T. Classification of endometriosis. Obstet. Gynecol. 1966; 28(3): 437.
- Acosta A.A., Buttram V.C. Jr, Besch P.K., Malinak L.R., Franklin R.R., Vanderheyden J.D. A proposed classification of pelvic endometriosis. Obstet. Gynecol. 1973; 42(1): 19-25.
- The American Fertility Society. Classification of endometriosis.Fertil. Steril.1979; 32(6): 633-4.
- Revised American Fertility Society classification of endometriosis: 1985. Fertil. Steril. 1985; 43(3): 351-2. https://dx.doi.org/10.1016/s0015-0282(16)48430-x.
- Revised American Society for Reproductive Medicine. Classification of endometriosis: 1996. Fertil. Steril. 1997; 67(5): 817-21.https://dx.doi.org/10.1016/s0015-0282(97)81391-x.
- Koninckx P.R., Meuleman C., Demeyere S., Lesaffre E., Cornillie F.J. Sugges tive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is as sociated with pelvic pain. Fertil. Steril. 1991; 55(4): 759-65. https://dx.doi.org/10.1016/s0015-0282(16)54244-7.
- Адамян Л.В., Кулаков В.И. Эндометриозы. М.: Медицина; 1998. [Adamyan L.V., Kulakov V.I. Endometriosis. Moscow: Medicina; 1998(in Russian)].
- Горпенко А.А., Чупрынин В.Д., Асатурова А.В., Смольнова Т.Ю., Буралкина Н.А. Опыт органосохраняющего оперативного лечения женщин с диффузной формой аденомиоза III-IV стадии. Consilium Medicum. 2021; 23(7): 552-7. [Gorpenko A.A., Chuprynin V.D., Asaturova A.V., Smolnova T.Yu., Buralkina N.A. Experience of uterus-sparing surgical treatment in diffuse (stages III-IV) adenomyosis. Consilium Medicum. 2021; 23(7): 552-7.(in Russian)]. https://dx.doi.org/10.26442/20751753.2021.7.201076.
- Ищенко А.И., Кудрина Е.А. Эндометриоз: диагностика и лечение. М.: ГЭОТАР-МЕД; 2002. 104 с. [Ishchenko A.I., Kudrina E.A. Endometriosis: diagnosis and treatment. M.: GEOTAR-MED; 2002. 104 p. (in Russian)].
- Tuttlies F., Keckstein J., Ulrich U., Possover M., Schweppe K.W., Wustlich M. et al. ENZIAN-score, a classification of deep infiltrating endometriosis. Zentralbl. Gynakol. 2005; 127: 275-81. https://dx.doi.org/10.1055/s-2005-836904.
Received 20.06.2022
Accepted 29.06.2022
About the Authors
Vladimir D. Chuprynin, PhD, Head of the Surgery Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-35-75,v_chuprynin@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Tatyana Yu. Smolnova, Dr. Med. Sci., Senior Reseacher at the Surgery Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
+7(495)438-40-68, smoltat@list.ru, https://orcid.org/0000-0003-3543-651X, Scopus Author ID: 6504317244, 117997, Russia, Moscow, Ac. Oparina str. 4.
Mikhail V. Melnikov, PhD, Head in Clinical Work, Surgery Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-78-33,
m_melnikov@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Natalia A. Buralkina, Dr. Med. Sci., Senior Researcher at the Surgical Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
+7(495)438-78-33, n_buralkina@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Authors’ contributions: Chuprynin V.D. – developing a treatment strategy and management of patients with endometriosis, analysis and review of the new classification, editing; Smolnova T.Yu. – collection and analysis of clinical data, analysis of the Russian and foreign literature, development of a new classification, writing the article; Melnikov M.V. – developing a treatment strategy and management of patients with endometriosis; Buralkina N.A. – assistance in the design of the article, editing.
Conflicts of interest: The authors declare that they have no competing interests.
Funding: The study was performed without external funding.
Ethical Approval: The study was approved by the Ethical Review Board of Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Chuprynin V.D., Smolnova T.Yu., Melnikov M.V., Buralkina N.A.
Surgical classification of endometriosis revisited.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 7: 68-74 (in Russian)
https://dx.doi.org/10.18565/aig.2022.7.68-74