В настоящее время известна значимость грудного вскармливания (ГВ) для профилактики инфекционных и неинфекционных заболеваний как ребенка (формирование правильного прикуса, более высокого индекса IQ интеллекта, профилактика ожирения, онкологических, аллергических заболеваний), так и матери (профилактика рака груди и яичников, остеопороза, сердечно-сосудистых заболеваний), причем не только в период ГВ, но и всю последующую жизнь [1]. Чем продолжительнее ГВ, тем более выражено его положительное влияние. Клинические данные свидетельствуют о том, что значимость эффектов ГВ увеличивается с каждым годом кормления [2]. Прежде всего это связано с уникальным биологическим составом грудного молока. Несмотря на известные преимущества ГВ для здоровья матери и ребенка и изначальный настрой матерей на ГВ, его распространенность значительно снижается в популяции уже в первые месяцы после родов [3]. Чаще всего это обусловлено трудностями, с которыми женщины сталкиваются в период становления ГВ, доступностью докорма смесью по желанию при отсутствии медицинских показаний в родильных домах, а также часто недоступностью профессиональной поддержки кормящих мам как на этапе родильного дома, так и после выписки [4, 5].
Известно, что поддержка ГВ уже на этапе беременности и в послеродовом периоде, основанная на соблюдении принципов 10 шагов «Инициативы по созданию в больницах благоприятных условий для грудного вскармливания» ВОЗ и ЮНИСЕФ (ранее – «Больница, доброжелательная к ребенку»), повышает исключительность и продолжительность ГВ. Причем, чем больше принципов из 10 внедрено в конкретном родильном доме, тем более вероятно успешное ГВ среди выписанных пациентов [6, 7].
Исследования выявили, что ненормированные (без медицинских показаний) предлактационные кормления ребенка смесью до наступления II стадии лактогенеза (использование докорма смесью на стадии формирования лактации) значительно снижают распространенность ГВ после выписки [8]. Докорм смесью в первые дни после рождения был связан с двукратным ростом смешанного вскармливания в возрасте от 30 до 60 дней и трехкратным риском прекращения ГВ к 60-му дню [9]. ВОЗ и Американская академия ГВ не запрещают использовать бутылки, но информируют о рисках, связанных с кормлением из них. Данный способ кормления является конкурирующим с сосанием груди, что может негативно сказываться на захвате груди и движениях языка во время сосания; у некоторых детей может проявиться отказ от груди в пользу бутылки [8, 10].
Целью данного исследования было проанализировать распространенность ГВ после выписки из роддома у диад мать-ребенок в зависимости от способа вскармливания в первые дни после рождения.
Материалы и методы
В ФГБУ «Научный центр акушерства гинекологии и перинатологии им. академика В.И. Кулакова» Минздрава России за период с апреля 2020 г. по июнь 2022 г. проводилось исследование на диадах мать-ребенок (n=37), которые получали докорм сцеженным молозивом и/или смесью. Все дети были доношенные и здоровые, с оценкой по шкале Апгар более 7 баллов; все приложены к груди в родильном зале или операционной сразу после рождения, большинство находились в палатах совместного пребывания. Состояние всех детей расценивалось как удовлетворительное все время пребывания в стационаре и при выписке. Критериями исключения были: осложнения послеродового периода у матери или ребенка (недоношенность, асфиксия при рождении и др.), перевод ребенка в отделение патологии новорожденных. В контрольную группу вошли диады мать-ребенок (n=24) исключительно на ГВ. В акушерско-гинекологическом анамнезе, в течении беременности различий между основной и контрольной группами не было. В контрольной группе у всех женщин были естественные роды, так как после операции кесарева сечения временное разлучение матери и ребенка в большинстве случаев приводит к применению докорма смесью. Проводились анкетирование и очный осмотр женщин и детей во время кормления. При анкетировании были учтены следующие параметры: гестационный возраст, вес при рождении, время первого прикладывания к груди, получал ли ребенок смесь, в каком количестве и каким способом, по каким причинам, были ли для докорма медицинские показания или только желание женщины, с какими сложностями при кормлении грудью столкнулись женщины, получили ли помощь специалиста по грудному вскармливанию, были ли удовлетворены ею, сцеживали ли женщины грудь, как часто, докармливали ли сцеженным молоком/молозивом ребенка, эффективность сосания груди ребенком.
Все женщины были проконсультированы специалистами из отдела поддержки грудного вскармливания института неонатологии и педиатрии ФГБУ «Научный центр акушерства гинекологии и перинатологии им. академика В.И. Кулакова» как минимум 1 раз, в основной группе – чаще 2 раз. Повторные консультации были необходимы тогда, когда корректировкой захвата груди ребенком и позиционированием его у груди не удавалось достичь эффективного и безболезненного кормления с первого раза. В этом случае проводился пальцевой тест и по его результатам подбирался логопедический массаж, которому также обучалась мама ребенка. Кроме того, на повторных консультациях продолжались обучение матери прикладыванию к груди и работа над улучшением эффективности сосания груди ребенком. Также у некоторых матерей применялись силиконовые накладки на соски, и у всех матерей вводилось сцеживание груди до момента начала эффективного сосания груди ребенком. Распространенность ГВ на первом году выявлялась при опросе по телефону в 1, 3, 6, 12 и 18 месяцев жизни ребенка, а в 1 и 3 месяца – еще наличие исключительно ГВ (после введения прикорма в диапазоне 4–6 месяцев исключительно ГВ становится невозможным). Вся информация получена с добровольного информированного согласия женщин.
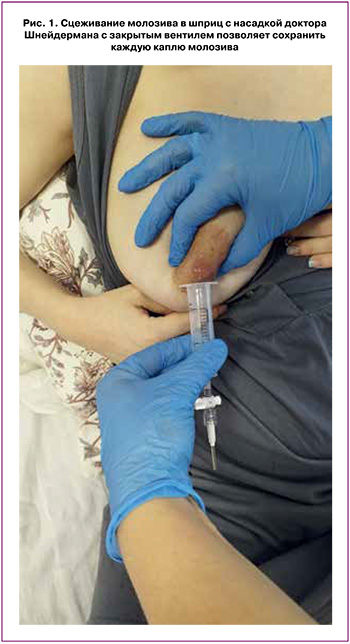
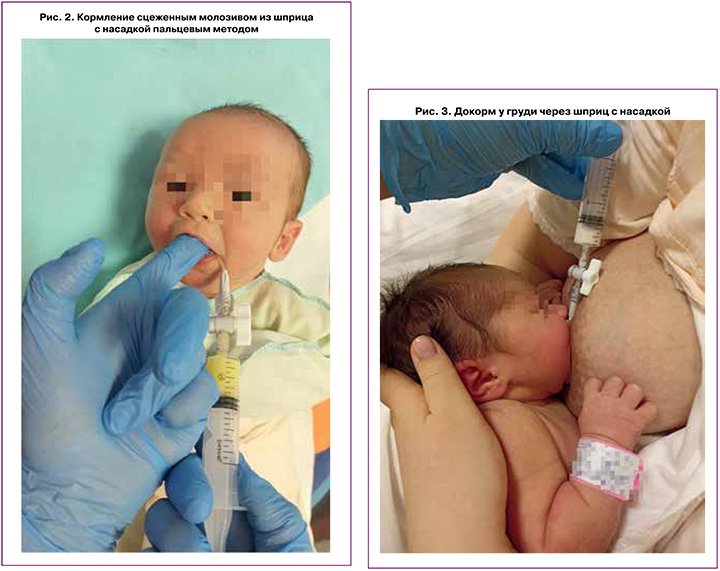
В зависимости от способа докорма в основной группе были сформированы две подгруппы. В 1-ю подгруппу вошли дети (n=18), получавшие докорм молозивом/молоком и частично смесью альтернативным способом – пальцевым кормлением из шприца. Все женщины этой подгруппы регулярно сцеживали грудь и докармливали сцеженным молозивом или молоком сразу после сцеживания. В этой подгруппе применялся новый удобный аксессуар – насадка на шприц (рис. 1–3), изобретенная доктором М.Г. Шнейдерманом [11, 12]. Главные преимущества данной насадки на шприц для докорма – поворотный вентиль, который в закрытом состоянии позволяет осуществить сбор молозива или молока в шприц при снятом поршне без потерь. При открытии вентиля молоко свободно поступает новорожденному через изогнутую трубочку защечно при давлении на поршень. В отличие от сбора молозива в шприц с насадкой доктора Шнейдермана, при сборе в шприц с удаленным поршнем без насадки с закрытой наконечником игле происходит вытекание молозива из иглы, несмотря на закрытый колпачок. Кроме того, насадка доктора Шнейдермана благодаря слегка изогнутому наконечнику позволяет удобно осуществлять докорм за щеку ребенка как при пальцевом кормлении (рис. 2), так и при кормлении без пальца и при докорме непосредственно у груди (рис. 3).
Во 2-ю подгруппу вошли дети (n=18), получавшие докорм смесью из бутылки. Всем матерям были объяснены риски кормления из бутылки и проведено обучение кормлению из шприца с сосанием и без сосания пальца. Во второй подгруппе матери осознанно сделали выбор в пользу кормления из бутылки как более удобного для них и традиционного, что и послужило критерием разделения на подгруппы.
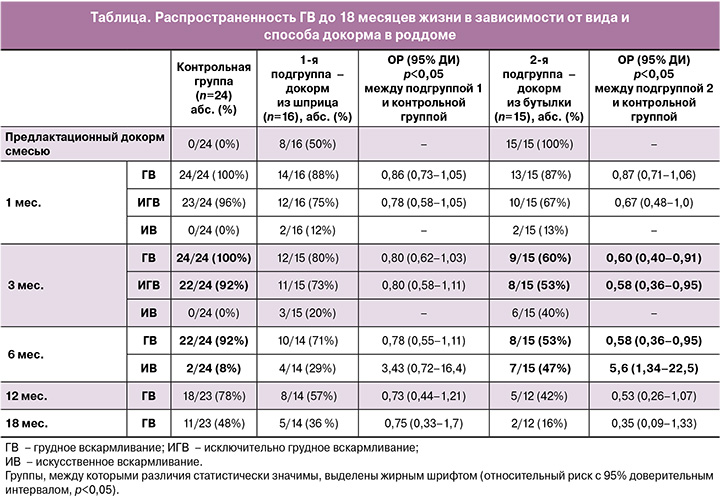
В 1-й подгруппе через месяц после родов удалось при телефонном опросе получить информацию о продолжении ГВ после выписки только у 16/18 (89%) матерей, в 3 месяца – у 15/18 (83%), в 6 месяцев и далее – у 14/18 (78%); во 2-й подгруппе – у 15/15 (100%) матерей в интервале от 1 до 6 месяцев, у 12/15 (80%) – в 12 и 15 месяцев (таблица). В контрольной группе в интервале от 1 до 6 месяцев удалось дозвониться до 24/24 (100%), а в 12 и 18 месяцев – до 23/24 (96%) матерей.
Статистический анализ
Статистический анализ проводили по общепринятым методам в пакете прикладных лицензионных программ Microsoft Office 2007. Качественные переменные представлены в абсолютных значениях и в процентном соотношении, также определялись средние значения со стандартным отклонением М (SD) и рассчитывался относительный риск с оценкой значения границ 95% доверительного интервала (ДИ), на основании чего делался вывод о статистической значимости выявленной связи между фактором риска и исходом при уровне значимости p<0,05 [13].
Результаты
У матерей 1-й подгруппы срок гестации составил 37–41 неделю (М (SD)=39,4 (1,15) недели). У 3/16 (19%) матерей было оперативное родоразрешение, у 13/16 (81%) – естественные роды. Масса детей при рождении составила 2750–4120 г (М (SD)=3396 (417,5) г), средняя длительность нахождения в роддоме – 3,8 (1,4) дня. В этой подгруппе сложности с прикладыванием ребенка к груди испытывали 5/16 (31%) матерей, патологическая потеря веса наблюдалась у 3/16 (19%) детей, 4/16 (25%) женщин испытывали боль при кормлении грудью в сочетании с трещинами или ссадинами сосков, 2/16 (12%) отмечали вялое сосание ребенком груди, 2/16 (12%) – чрезмерное беспокойство ребенка как основную причину докорма. У большинства детей – 11/16 (69%) этой подгруппы были выявлены особенности сосания при проведении пальцевого теста.
Все матери (100%) нуждались в помощи специалиста по ГВ, и все были удовлетворены оказанной помощью. Все матери были вынуждены начать докорм в первые двое суток после родов. Причем половина (8 матерей) докармливали только своим сцеженным молоком, а 8 (50%) – сочетали кормление сцеженным молоком с докормом смесью. Причиной докорма смесью по медицинским показаниям были трудности с прикладыванием ребенка к груди, большая потеря массы тела – 12/16 (75%) и желание женщины – 4/16 (25%). II стадия лактогенеза наступила у матерей 1-й подгруппы через 3,25 (0,45) дня после родов.
Большинство женщин – 17/18 (94%) – из тех, кто использовали докорм из шприца с насадкой доктора Шнейдермана М.Г., высоко оценили удобство использования насадки на шприц и постоянно применяли ее (рис. 1, 2). Одна женщина применяла только изредка, мотивируя, что удобнее собирать молозиво через носик, не снимая поршень, и докармливать по пальцу непосредственно из шприца. Вероятно, это было обусловлено небольшими объемами сцеженного молозива. Кроме того, насадка применялась непосредственно у груди матери, через шприц с насадкой подавался докорм сцеженным молозивом (молоком) или смесью при выраженном беспокойстве у груди и отказном поведении (рис. 3).
Гестационный возраст при рождении во 2-й подгруппе составил 37–41 неделю (М (SD) = 39,3 (1,17)). У 9/15 (60%) женщин было оперативное родоразрешение, у 6/15 (40%) – естественные роды. Масса тела детей при рождении составляла 2750–4120 г (М (SD)=3367 (388,4) г). Все дети были приложены к груди в родильном зале или операционной в течение первых 30 минут жизни. Средняя продолжительность пребывания в роддоме во 2-й подгруппе составила 4,05 (1,08) дня. Все дети, рожденные путем операции кесарева сечения, в первые сутки получали докорм из бутылки. Некоторых новорожденных докармливали смесью более суток в связи с состоянием матерей. 3/15 (20%) матерей находились в палатах раздельного пребывания, в дневные часы у них была возможность совместного пребывания. Детей им приносили на кормление не менее 6 раз в сутки. II стадия лактогенеза наступила у матерей этой подгруппы на 3,5 (0,65) день после родов. Со сложностями с прикладыванием к груди столкнулись 3/15 (20%) матерей, 9/15 (60%) испытывали боль при кормлении грудью, у 7/15 (47%) были трещины или ссадины сосков, 2/15 (13%) ребенка сосали грудь редко и непродолжительно. 8/15 (54%) женщин нерегулярно сцеживали грудь. 100% детей получали докорм смесью, из них 6/15 (40%) получали докорм смесью 6 раз в сутки, 9/15 (60%) – 4 и менее раз в сутки. Причиной докорма смесью 6/15 (40%) матерей назвали голод ребенка и недостаточное количество молозива и докармливали смесью без медицинских показаний по собственному желанию. Болезненность при кормлении грудью усилилась у 3 женщин после введения докорма смесью из бутылки. Все матери нуждались в помощи специалиста по ГВ, все были удовлетворены оказанной помощью.
Продолжительность ГВ, исключительно ГВ и распространенность смешанного вскармливания в 1, 3, 6, 12 и 18 месяцев в обеих подгруппах и контрольной группе представлены в таблице. Распространенность ГВ во всех временных промежутках была больше в подгруппе с докормом из шприца, но статистически значимых различий между подгруппами не получено. Вероятно, это связано с неоднородностью группы с докормом из шприца – докорм смесью (также из шприца) присутствовал у половины детей из этой группы, преимущественно по медицинским показаниям. Кроме того, в этой группе чаще – у 11/16 (69%) детей – встречались особенности сосания при проведении пальцевого теста (поршневидные движения языка, кусающие движения нижней челюсти без выкладывания языка и другие), требующие проведения логопедического массажа.
Все дети из основной группы – 3/16 (19%) из 1-й подгруппы и 4/15 (27%) из 2-й, получавшие докорм смесью в возрасте 1 и 3 месяцев, к 6 месяцам полностью перешли на искусственное вскармливание. Вероятно, это связано с тем, что докорм смесью часто с течением времени подавляет по принципу обратной связи ГВ.
Гестационный возраст при рождении в контрольной группе составил 37–41 недель (М (SD)=39,1 (2,59) недель), масса тела детей при рождении составляла 2750–4120 г (М (SD)=3421,5 (318,6) г), средняя длительность нахождения в роддоме составила 3,4 (0,58) дня. Все дети родились естественным путем и были приложены к груди в родильном зале, все матери находились совместно со своими детьми, которые вскармливались исключительно грудью. 17/24 (70,8%) матерей нуждались в помощи специалиста по ГВ. Сложности с прикладыванием к груди испытывали 11/24 (45,8%) матерей, 14/24 (58,3%) испытывали боль при кормлении грудью, у 9/24 (37,5%) были трещины или ссадины сосков, 6/24 (25%) женщин временно сцеживались из-за сложностей с прикладыванием к груди и болезненности кормления. II стадия лактогенеза наступила у матерей этой группы раньше – на 2,9 (0,36) сутки после родов, что, вероятно, связано с частым прикладыванием к груди и отсутствием оперативного родоразрешения у матерей этой группы, отодвигающего наступление второй стадии лактогенеза, однако различия не были статистически значимыми.
Количество диад мать-ребенок на ГВ во всех возрастных периодах предсказуемо превалировало в контрольной группе по сравнению с подгруппами, которые получали докорм (таблица). Однако статистически значимыми различия были только по сравнению со 2-й подгруппой (с предлактационным докормом смесью из бутылки) – в 3 и 6 месяцев соответственно (таблица). Причем риск полного перехода на искусственное вскармливание в возрасте 6 месяцев в 5,6 раза выше во 2-й подгруппе по сравнению с контрольной группой (ОР 5,6; 95% ДИ 1,34–22,5; p<0,05).
Обсуждение
Исключительно ГВ в роддоме является важным правильным стартом ГВ и связано с более длительным кормлением грудью в дальнейшем, что подтверждается многочисленными данными литературы [1–3, 14, 15]. Также крайне важна профессиональная поддержка в первые дни после родов, когда женщины сталкиваются с такими проблемами, как боль в сосках при кормлении и невозможность приложить к груди ребенка. Чаще всего оптимальное позиционирование ребенка у груди и правильное прикладывание помогают устранить данные проблемы. Однако в ряде случаев этого бывает недостаточно, и тогда женщины нуждаются в более длительной поддержке ГВ. Грамотно организованный докорм сцеженным молоком или молозивом помогает сформировать лактацию и сохранить исключительно ГВ даже при отсутствии эффективного сосания ребенком груди [15].
При появлении трудностей с ГВ, особенно сопровождающихся беспокойством ребенка, часто используется докорм смесью по желанию женщины без медицинских показаний. Профессиональная поддержка ГВ помогает избежать или хотя бы значительно уменьшить количество применяемой смеси, так как основным видом докорма при этом становится сцеженное молоко или молозиво через шприц, что способствует формированию лактации по принципу обратной связи [9, 15, 16]. В нашем исследовании 6/15 (40%) матерей во 2-й подгруппе предлагали смесь из бутылки своему ребенку из-за беспокойного поведения ребенка у груди, несмотря на оказанную поддержку специалистов по ГВ. Пациентки 2-й подгруппы проигнорировали рекомендацию сцеживания и докорма сцеженным молоком или молозивом, причем у 6/15 (40%) это привело к прекращению лактации в первые 3 месяца, а риск полного перехода на искусственное вскармливание в 6 месяцев жизни в 5 раз выше в этой подгруппе по сравнению с детьми, находящимися исключительно на ГВ (ОР 5,6; 95% ДИ 1,34–22,5; p<0,05).
В 1-й подгруппе матерей, которые сцеживались и кормили сцеженным молоком, распространенность ГВ была выше во все временные периоды, по сравнению с женщинами, которые не сцеживались, однако эти различия статистически не значимы. Причем именно в 1-й подгруппе докорма через шприц докорм смесью в основном был по медицинским показаниям и только у четверти (4/16 (25%)) – по желанию женщины, что, вероятно, связано с более серьезными нарушениями лактации в этой подгруппе.
Полностью перешли на искусственное вскармливание в первые 3 месяца дети из 2-й подгруппы, получавшие в роддоме большие суточные объемы смеси – от 120 до 300 мл. Это согласуется с данными литературы – только строго дозированное (малыми объемами) краткосрочное вскармливание новорожденных из шприца на фоне поддержки ГВ не повлияло на ГВ в течение 6 месяцев, а сохранение докорма смесью в возрасте 1 недели связано с прекращением ГВ до 6 месяцев [16].
Во 2-й подгруппе женщин, которые не стали регулярно сцеживаться и докармливать детей своим молоком, несмотря на соответствующие рекомендации, распространенность ГВ статистически значимо меньше по сравнению с группой, чьи дети были исключительно на ГВ в 3 и 6 месяцев, и риск потери ГВ в 6 месяцев в 5 раз выше, что согласуется с данными литературы. В исследовании с участием 1500 женщин только раннее исключительное ГВ оказалось статистически значимым для достижения предполагаемой продолжительности ГВ (ОШ 2,3; 95% ДИ 1,8–3,1) [17]. Данные, собранные Центром по контролю и профилактике заболеваний, включающие данные о вскармливании младенцев и практике родовспоможения в более чем 1300 больницах США, показали, что более высокие баллы по внедрению поддерживающей ГВ практики ухода за беременными и кормящими (аналог инициативы ВОЗ «Больница, доброжелательная к ребенку») были связаны с более высокими показателями исключительно ГВ во время выписки из стационара и при любом и исключительно ГВ в 8 недель после родов [18].
Болезненное прикладывание к груди, наблюдавшееся у половины всех женщин (27/55 (49%)), участвовавших в нашем исследовании, заслуживает особого внимания. По данным литературы, это приводит к снижению количества молока, нарушению оттока молока и раннему прекращению ГВ [19]. Исследование, проведенное в США, показало, что боль и травма сосков были одними из наиболее часто упоминаемых причин раннего отлучения от груди. В исследовании с участием более 1600 женщин с одноплодными родами примерно у 10% боль в сосках сохранялась на 7-й день после родов; 72% из них были связаны с неправильным позиционированием и захватом груди, 23% – с короткой уздечкой языка и 4% – с очень частым кормлением. Женщины, получавшие помощь, выздоравливали в течение 1–2 недель, а показатели исключительно ГВ в течение 6 недель не отличались от таковых у матерей без болей в сосках [20]. Следовательно, женщинам с болью в сосках при кормлении грудью особенно важна профессиональная помощь для сохранения лактации в дальнейшем [21].
В настоящее время отмечается некоторая отрицательная динамика по продолжительности ГВ в Российской Федерации по данным Росстата (2021 г.) – в 2020 г. уменьшилось количество детей на ГВ в 6 и более месяцев (39,2%) по сравнению с 2010 г. (40,4%); женщины чаще стали прекращать кормить грудью в возрасте от 3 до 6 месяцев [22]. В нашем исследовании видно, что в подгруппе с докормом из шприца, в которой были наиболее распространены трудности с прикладыванием к груди и были медицинские показания к докорму смесью, распространенность ГВ на первом году выше, чем в целом по России. Ключевым моментом в этом, вероятнее всего, является личная мотивация женщин на сохранение ГВ, несмотря на трудности, а также профессиональная поддержка специалистами из отделения поддержки ГВ и строго дозируемое количество смеси, подаваемое несосательным методом – из шприца, что согласуется с данными литературы [17, 18, 21].
Современные исследования свидетельствуют о влиянии даже небольшого количества смеси в первые дни жизни на состав микробиома на первом году жизни. Среди младенцев, находящихся на исключительно ГВ в возрасте 3 месяцев (n=579), выявлены изменения микробиома у тех младенцев, которые получали смесь в период новорожденности (n=179) [23]. Следовательно, применение докорма смесью требует строгого дозирования смеси, применяемой по медицинским показаниям для сохранения продолжительного ГВ в дальнейшем [24]. В недавнем исследовании, где было проанализировано 3 230 500 рождений в США в 2017 г., выявлено, что ГВ в значительной степени связано со снижением вероятности постперинатальной младенческой смертности (на 26%) в различных расовых и этнических группах населения США [25]. Поэтому центр контроля заболеваемости ставит национальной задачей в программе «Здоровые люди-2030» повышение распространенности исключительно ГВ, начиная с родильного дома, и снижение распространенности предлактационного кормления смесью.
В Указе Президента Российской Федерации от 06.06.2019 № 254 «О Стратегии развития здравоохранения в Российской Федерации на период до 2025 года» особое внимание уделено профилактике заболеваний и снижению младенческой смертности на период до 2025 г. [26]. Все вышесказанное позволяет рассматривать повышение распространенности ГВ как национальную здоровьесберегающую стратегию [27].
Заключение
Предлактационное (до наступления II стадии лактогенеза) применение смеси из бутылки без регулярного опорожнения молочных желез приводит к статистически значимому снижению распространенности ГВ в 3 и 6 месяцев по сравнению с группой на исключительно ГВ. Причем риск прекращения ГВ в возрасте 6 месяцев в 5 раз выше, если в роддоме применялся предлактационный докорм смесью из бутылки, по сравнению с группой на исключительно ГВ в роддоме.
Для сохранения исключительно ГВ в роддоме, когда есть сложности с прикладыванием к груди, необходимо обучение регулярному сцеживанию груди и докорму сцеженным молозивом или молоком несосательным способом – пальцевым методом через шприц. Таким образом, исключительно ГВ в родильном доме способствует увеличению продолжительности ГВ в дальнейшем. Исключительно ГВ в роддоме зависит от мотивации женщин на ГВ (сформированной до родов лактационной доминанты) и профессиональной поддержки ГВ, позволяющей преодолеть возникающие трудности в начале ГВ, избегая применения предлактационного докорма смесью без медицинских показаний.
По нашему мнению, для увеличения распространенности ГВ в России считаем целесообразным формирование службы профессиональной поддержки ГВ как на этапе стационара, так и на амбулаторном этапе. Также назрела необходимость повышения социальной значимости ГВ для формирования мотивации женщины на кормление грудью в дородовом периоде.