Early diagnosis of endometrial hyperplasia based on clinical and anamnestic factors
Frolova Yu.S., Elgina S.I.
Objective: To determine clinical and anamnestic factors in the development of endometrial hyperplasia based on the analysis of the results of hysteroscopy and aspirate morphology.
Materials and method. A prospective cohort study was conducted for 3 years (2019–2021). The study included 900 women aged 20–70 years who underwent hysteroscopy and morphological assessment of the aspirate. Group I consisted of 440 women with hysteroscopically and morphologically confirmed endometrial hyperplasia, group II included 460 women without confirmed endometrial hyperplasia. In all cases, the indication for hysteroscopy were menstrual irregularities of unknown etiology, the pathological process that was detected or suspected during ultrasound examination.
Results: Statistically significant differences in clinical and anamnestic factors were found between the women with hysteroscopically and morphologically confirmed endometrial hyperplasia and the women without confirmed endometrial hyperplasia. Based on the obtained data, a computer program was developed using logistic regression for detection of endometrial hyperplasia. The sensitivity of this detection method was 88.7%, and the specificity was 92.6%. The computer program "Clinical and anamnestic factors for early diagnosis of endometrial hyperplasia" was submitted for registration to the Federal Service for Intellectual Property (Moscow).
Conclusion: The program "Clinical and anamnestic factors for early diagnosis of endometrial hyperplasia" can be recommended for routine use for detection of endometrial hyperplasia and carrying out therapeutic measures.
Authors’ contributons: Frolova Yu.S., Elgina S.I. – the concept and design of the study; writing the text of the article;
Frolova Yu.S. – material collection and processing; Elgina S.I. – article editing.
Conflicts of interest: The authors declare that they have no conflict of interests regarding publication of this article.
Funding: The study is financed by Kemerovo City Clinical Hospital No. 4, Kemerovo, Russia, the funds of compulsory health insurance; and private means.
Ethical Approval: The study is approved by Research Ethics Committee of Kemerovo State Medical University of the Ministry of Health of Russia (the Order of the Ministry of Health of Russian No. 266 of June 19, 2003).
Patient Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Frolova Yu.S., Elgina S.I. Early diagnosis of endometrial hyperplasia based on clinical and anamnestic factors. Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2023; (11): 132-139 (in Russian)
https://dx.doi.org/10.18565/aig.2023.96
Keywords
The prevalence rate of female reproductive system diseases is growing every year [1–4]. At the same time, the rates of cancer diagnoses in the gynecological structure of diseases continue to grow. So, from 2011 to 2016 in Russia, the number of cases of uterine cancer increased from 204,764 to 250,527 [3, 5, 6].
High growth rates of uterine and endometrial pathology make the researchers look for new approaches to early effective diagnosis of gynecological diseases, which will make it possible to verify the accuracy of the diagnosis at a minimal cost and in a short time and start appropriate treatment [2, 7, 8]. Endometrial hyperplasia is associated with the impact of various factors to which a woman is exposed throughout her life. However, the most significant predictors are highlighted. The age and the presence of various diseases, both gynecological (uterine fibroids) and extragenital (obesity, hypertension) diseases increase the risk of developing this pathology. Ovarian tumors are associated with endometrial hyperplasia in 19.6% of cases, with endometriosis in 15.3% [7]. Recurrences of previous endometrial hyperplastic processes happen in 10.0% of cases without adequate therapy.
According to some authors, menopausal transition and postmenopause are “vulnerable” age periods for endometrial hyperplastic processes, which are identified in 62.5% of cases in the structure of gynecological diseases. The women with endometrial hyperplasia have endocrine diseases in 31.5% of cases (polycystic ovary syndrome, thyroid and pituitary dysfunction [11].
In view of the above, early detection of endometrial hyperplasia is relevant today.
The purpose of the study was to determine clinical and anamnestic factors in the development of endometrial hyperplasia (EH) based on the analysis of the results of hysteroscopy and aspirate morphology.
Materials and methods
The study was performed in Kemerovo City Clinical Hospital No. 4, Kemerovo. The study was approved by the Research Ethics Committee of Kemerovo State Medical University of the Ministry of Health of Russia (the Order of the MH of Russia No. 266 of June 19, 2003). The women signed voluntary informed consent.
A prospective cohort study was carried out from 2019 to 2021. The study included 900 patients aged 20–70 years, who underwent hysteroscopy and morphological examination of aspirates. The number of women was limited by the term of carrying out the study and rule-out criteria.
The indications for hysteroscopy were menstrual irregularities of unclear etiology, detected or suspected pathological process during ultrasound examination. The diagnosis of endometrial hyperplasia was made on the basis of visualization of the uterine cavity during hysteroscopy, that was performed to obtain endometrial tissue sample from the uterine cavity by manual vacuum aspiration for pathological examination.
Endometrial hyperplasia was classified according to the WHO classification of endometrial hyperplasias (the latest publication in 2020 of new classification system of endometrial hyperplasia, WHO 2014) [1]. Out of 900 patients, 440 women were included in group I, in whom the diagnosis of endometrial hyperplasia was confirmed by hysteroscopy and morphological examination. Of them, 414/490 (94.1%) women had EH without atypia, and 26 (5.9%) women had EH with atypia. Group II included 460 women without confirmed diagnosis of endometrial hyperplasia. The results of pathological examination in women in group II showed that proliferation phase of endometrial defect was in 92.4% of cases and fibrotic stroma was in 7.6% of cases.
Inclusion criteria in group I (the main group) were women aged 20–70 years with hysteroscopically and morphologically confirmed endometrial hyperplasia.
Inclusion criteria in group II (the control group) were women aged 20–70 years inclusively, without hysteroscopically and morphologically confirmed endometrial hyperplasia.
Non-inclusion criteria in the study were women below 20 years and over 70 years of age, who were pregnant at the time of the study, had acute abnormal uterine bleeding, the diagnosis of endometrial hyperplasia that was made less than 5 years ago, polycystic ovary syndrome, thyroid and pituitary dysfunction, oncological diseases of different localization, who currently take different types of hormone therapy, refusal to participate in the study.
Lehr's formula for relative values was used to calculate the sample size per group:

where n – the sample size; Z – confidence probability = 1.96; p – the proportion of respondents with the presence of the studied characteristic; q=1-p is the proportion of respondents, who had no the studied characteristic; ∆ – a margin of sampling error.
At the same time, 95% confidence probability was selected, and 5% confidence interval. According to the published data, the prevalence of endometrial hyperplasia among female population at the age of 20–70 years is 5.0–10.1% [1, 12]. General sample size of the respondents, the female population aged 20 – 70 years, who were the patients of Kemerovo City Clinical Hospital No.4, was 39,850 women. Therefore, the required sample size was 140 patients. The number of actually selected patients for the study exceeded the sample size.
Statistical analysis
Statistical data processing was performed using software programs Microsoft Office Excel 2013 (Education licensing Open License 62007606) and IBM SPSS Statistiсs Base Campus Edition Campus Value Unit License v. 24 (Licensing agreement No. 20160805-1 of August 30, 2016 with LLC “Predictive Solutions”).
- Normality of distribution was checked using the Lilliefors-corrected Kolmogorov-
- Smirnov test.
Since the groups had non-normal distribution, the Mann–Whitney test was used to analyze the quantitative data in two independent samples at p<0.05.
The quantitative data are presented as median (Me) and interquartile range (the 25th and the 75th quartile) [Q1; Q3].
The quantitative values are presented as absolute values (abs, %). The qualitative parameters in 2 groups of patients were assessed using Pearson’s chi-squared test or Fisher’s exact test was used depending on the minimum expected number.
For statistically significant differences between the parameters, assessment of chances with 85% confidence interval (RR 95% CI) for each factor (significance level at p<0.05) was made, as well as a measure of association between nominal data was defined.
The interaction between the factors and collinearity were assessed, and the most significant factors were selected. Selection from a large number of characteristics was performed using step-by-step approach by sequential assessment of the significance of factors.
The detected clinical and anamnestic factors in women with endometrial hyperplasia that was confirmed by hysteroscopy and morphological examination provided the basis for early detection of this pathology. Binary logistic regression was used in creating the computer program.
Regression coefficients were calculated for all factors of endometrial hyperplasia. The significance of the identified factors was determined using Wald test. The probability of endometrial hyperplasia was calculated using the formula:
p=1/1+е-z (2),
where р – probability of endometrial hyperplasia; e – exponent = 2.852; z – dependent variable.
Calculation of the dependent variable z was performed using the formula:
z=а+ b1x1+ b2x2+ b3x3+…+ bixi (3),
where a – constant; bi – regression coefficients; xi – independent variables.
The probability of endometrial hyperplasia p varies in the range of 0–1. The probability is considered to be low at p<0.5 (0–0.4999), and high at р≥0.5 (0.5–1.0). In that case, the probability of the pathology is 99.0%.
Results and discussion
Eighteen clinical and anamnestic factors including the age of women, the character of menstrual function, parity, presence of gynecological diseases, extragenital pathology, method of contraception were analyzed. The age of women in the groups under study is presented in Table 1.
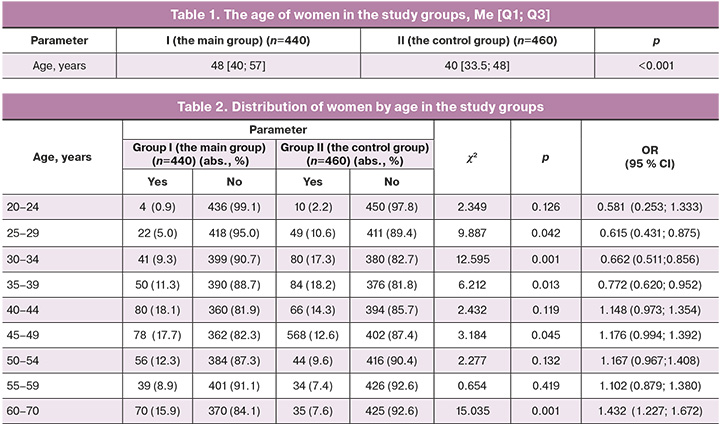
The age of women with hysteroscopically and morphologically confirmed endometrial hyperplasia was higher versus the age of women without confirmed endometrial hyperplasia.
Distribution of women by age is shown in Table 2. Persons’s chi-squared test was used for calculations.
Pathological examination most often confirmed endometrial hyperplasia in women aged 45–49 years (OR=1.176 (95% CI 0.994; 1.392)) and 60–70 years (OR=1.432 (95% CI 1.227; 1.672)). The age of women of 25–39 years was a factor reducing the probability of endometrial hyperplasia. At the same time, at the younger age, the risk of development of the pathology is less: 25–29 years (OR=0.615 (95% CI 0.431; 0.875)), 30–34 years (OR=0.662 (95% CI 0.511; 0.856)), 35–39 years (OR=0.772 (95% CI 0.620; 0.952)). The diagnosis of endometrial hyperplasia was made 2 times more often in postmenopausal women – 70% versus 35% (OR=1.432 (95% CI 1.227; 1.672)).
Menstrual cycle characteristics in patients at the time of inclusion in the study are shown in Table 3. Fisher’s exact test was used for calculations.
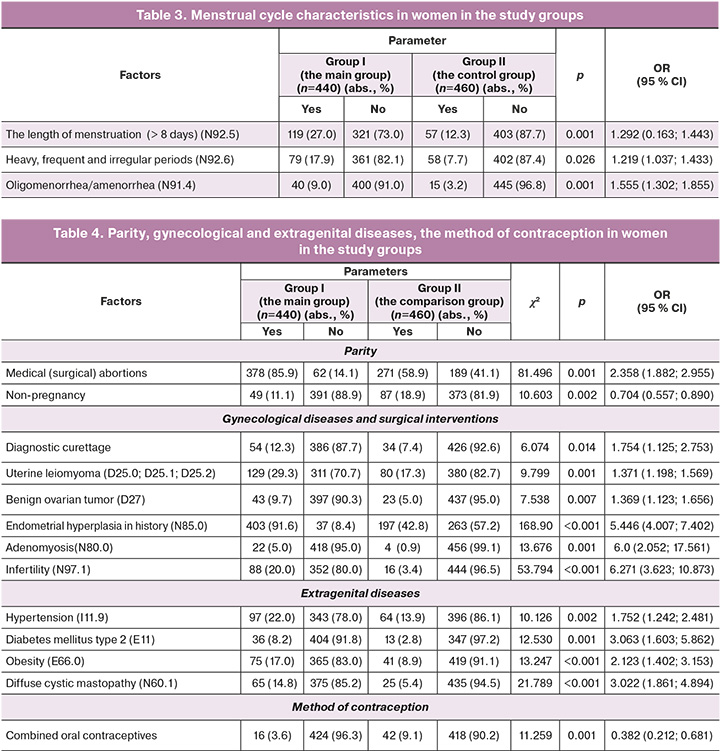
Long menstrual periods most often were in women in group 1 – 27.0% versus 12.3% of women in group II (OR=1.292 (95% CI 0.163; 1.443)).
In women in group I, abnormal periods (heavy, frequent and irregular) were observed most often (17,9%), oligomenorrhea/amenorrhea (9.0%); while in women in group II – in 7.7% and 3.3% of cases, respectively (OR=1.219 (95% CI 1.037; 1.433)), OR=1.555 (95% CI 1.302; 1.855)).
Parity, gynecological and extragenital diseases, method of contraception are shown in Table 4. Pearson’s chi-squared test was used for calculations.
Medical (surgical) abortions (OR=2.358 (95% CI 1.882; 2.955)), diagnostic curettage (OR=2.358 (95% CI 1.882; 2.955)) and non-pregnancy in anamnesis also were observed more often in women with endometrial hyperplasia (OR=0.482(95% CI 0.334; 0.705)).
Non-pregnancy reduced the risk of endometrial hyperplasia (OR=0.704 (95% CI 0.557; 0.890)). Probably, this fact was associated with lower number of women aged below 34 years, who had endometrial hyperplasia in the main group versus the control group (67 versus 139 women), and was due to the current tendency to realize reproductive function at a later age.
The women in group I were more often diagnosed with gynecological diseases, such as benign ovary masses (OR=1.369 (95% CI 1.123; 1.656)), uterine leyomyomas (OR=1.371(95% CI 1.198; 1.569)), adenomyosis (OR=6.0 (95% CI 2.052; 17.562)), infertility (OR=6.271 (95% CI 3.623; 10.873)). Previous endometrial hyperplasia was 2 time more often in women in group I versus the women in group II (OR=5.446 (95% CI 4.007; 7.402)), despite the fact that they had undergone hormone therapy for treatment of hyperplastic processes according to the clinical recommendations [1].
Extragenital diseases were more often in women in group I. Among extragenital diseases, hypertension (OR=1.752 (95% CI 1.242; 2.481)), obesity (OR=2.123 (95% CI 1.402; 3.153)), type 2 diabetes mellitus (OR=3.063 (95% CI 1.603; 5.862)) prevailed. Diffuse fibrocystic mastopathy was 2 times more often in women in group I versus the women in the control group (OR=3.022 (95% CI 1.861; 4.894)).
The women in the main group used combined oral contraceptives as a method of contraception less often – in 3.6% of cases versus 9.1% (95% CI 0.212; 0.681)), and preferred barrier methods (condoms and withdrawal).
The analysis of clinical and anamnestic factors detected statistically significant predictors. The modifiable risk factors for endometrial hyperplasia are the length (more than 8 days), the character of menstruation (heavy, regular), nulliparity, medical (surgical) abortions, diagnostic curettage; gynecological diseases, such as uterine leiomyoma, benign ovary masses, endometrial hyperplasia in history, adenomyosis, infertility; extragenital diseases – hypertension, type 2 diabetes mellitus, obesity, diffuse cystic mastopathy. The non-modifiable risk factors are the age of women at the time of making diagnosis. However, the women below the age of 39 years who take combined oral contraceptives have lower risk of developing endometrial hyperplasia.
Based on obtained information, the computer program was developed using logistic regression to define the risk group for the presence of endometrial hyperplasia. The ranking of the significance of the above described predictors was performed using the Wald test and showed the following results: the most significant predictor was age, then obesity, adenomyosis, endometrial hyperplasia in anamnesis, length of menstruation, somatic diseases – type 2 diabetes mellitus, hypertension, taking combined oral contraceptives, diffuse cystic mastopathy. All coefficients are significant according to the Wald test and influence the occurrence of endometrial hyperplasia (Table 5).
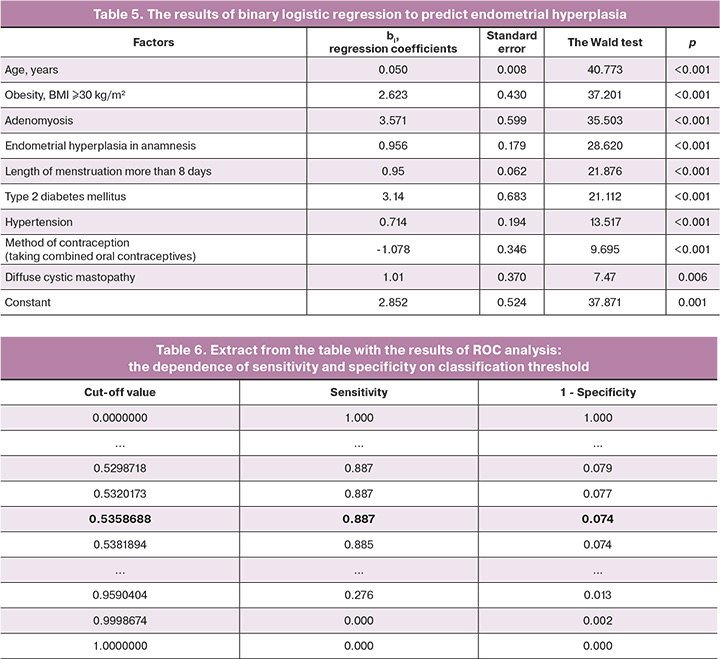
Based on the values of regression coefficients, all predictors had a direct relationship with the likelihood of endometrial hyperplasia.
The probability of the presence of endometrial hyperplasia was determined using formulas (2) and (3) with calculated regression coefficients. Using the obtained constants and regression coefficients bi presented in the Table and formulas (2) and (3), we obtained the equation:

By substituting the value xi (independent variables) into the equation, we obtain the probability of the presence of endometrial hyperplasia (dependent variable): Age – х1 (years); Obesity – х2 (0 means “no”, 1 mean “yes”); Adenomyosis – х3 (0 means “no”, 1 means “yes”); Endometrial hyperplasia in anamnesis – х4 (0 means “no”, 1 means “yes”); The length of menstruation more than 8 days – х5 (days); Type 2 diabetes mellitus – х6 (0 means “no”, 1 means “yes”); Hypertension – х7 (0 means “no”, 1 means “yes”); Method of contraception (intake of combined oral contraceptives) – х8 (0 means “no”, 1 means “yes”); Diffuse cystic mastopathy – х9 (0 means “no”, 1 means “yes”).
ROC analysis and construction of ROC curve were used to assess the quality of the created model. The percentage of correct classification of the model of the overall unfavorable outcome (the presence of endometrial hyperplasia) was 96.4%, AUC=0.964, p<0.001 (Figure).
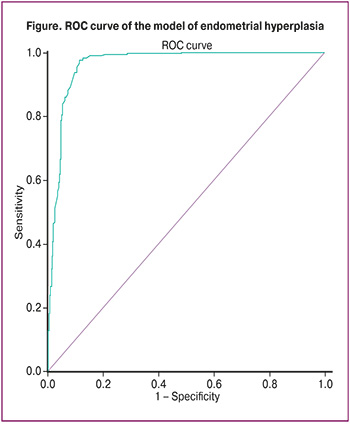
ROC analysis showed that the overall optimal cut-off threshold in the created model was at р>0.535 (Table 6).
The percentage of correct reclassification (model accuracy) was 91.1%, sensitivity – 88.7%, specificity – 92.6%. The given indicators demonstrate that the mode has high validity.
The use of this diagnostic model implies entering the women’s data into the computer for subsequent software program to calculate the presence of endometrial hyperplasia. The computer program “Clinical and anamnestic factors in early diagnosis of endometrial hyperplasia” was submitted for registration to the Federal Service for Intellectual Property (Moscow).
Testing of the developed model is planned using the independent sample.
This model cannot be used for women below 20 years and over 70 years of age, who have polycystic ovary syndrome, thyroid and pituitary disorders, oncological diseases and currently take hormonal drugs, and for pregnant women.
Discussion
Despite a wide range of diagnostic procedures, identification of endometrial hyperplasia in the early stages not always remains possible. Most often, the specialists do not perform pelvic ultrasound at the initial visit of patients to the outpatient facility, or in some cases, the women do not complain of menstrual irregularities considering them as normal. Due to this, the time frame from making the diagnosis to the occurrence of the disease increases. Medical societies develop simple and at the same time effective diagnostic methods for the identification of diseases, including endometrial hyperplasia. Our study included a comprehensive assessment of a significant number of clinical and anamnestic risk factors for the development of endometrial hyperplasia, which are both modifiable and non-modifiable. Some of the established predictors of endometrial hyperplasia are confirmed with the data obtained by other authors [1, 13, 14]. However, a comprehensive assessment of predictors was not given, and it was impossible for us to assess the impact of aggregate factors on the development of endometrial hyperplasia. The obtained data formed the basis for the development of the computer program “The clinical and anamnestic factors in early diagnosis of endometrial hyperplasia”, which will make it possible for primary care specialists to identify the risk group for developing endometrial hyperplasia among the female population without using instrumental diagnostic techniques.
Conclusion
Thus, the computer program based on determination of clinical and anamnestic factors, can be recommended to be used for early identification of the risk group among women at the age of 20–70 years with endometrial hyperplasia, differential approach to their follow-up and timely application of preventive and treatment measures.
References
- Министерство здравоохранения Российской Федерации. Гиперплазия эндометрия. Клинические рекомендации. 2021. [Ministry of Health of the Russian Federation. Hyperplasia of the endometrium. Clinical guidelines. 2021. (in Russian)].
- Адамян Л.В., Мельникова Н.С., Касян В.Н. Патология эндометрия в постменопаузе: нужен ли ультразвуковой скрининг? Проблемы репродукции. 2019; 25(2): 113-9. [Adamyan L.V., Melnikova N.S., Kasyan V.N. Endometrial pathology in postmenopausal women: do we need ultrasound screening? Russian Journal of Human Reproduction. 2019; 25(2): 113-9. (in Russian)]. https://dx.doi.org/10.17116/repro201925021113.
- Аксель Е.М., Виноградова Н.Н. Статистика злокачественных новообразований женских репродуктивных органов. Онкогинекология. 2019; 3(27): 64-78. [Aksel E.M., Vinogradova N.N. Statistics of malignant neoplasms of female reproductive organs. Oncogynecology. 2019; 3(27): 64-78. (in Russian)]. https://dx.doi.org/10.52313/22278710_2018_3_64.
- Сафронов О.В., Казачкова Э.А., Казачков Е.Л., Сафронов Е.О., Пустовал М.Л., Коршунов Д.В. Частота и структура внутриматочной патологии, подлежащей малоинвазивному хирургическому лечению, в свете учения о патоморфозе. Уральский медицинский журнал. 2020; 3 (186): 65-70. [Safronov O.V., Kazachkova E.A., Kazachkov E.L., Safronov E.O., Pustovaia M.L., Korshunov D.V. Prevalence rate and structure of minimally invasive surgical intrauterine pathology in the light of pathomorphosis theory. Urals Medical Journal. 2020; 3(186): 65-70. (in Russian)]. https://dx.doi.org/10.25694/URMJ.2020.03.3.
- Doherty M.T., Sanni O.B., Coleman H.G., Cardwell C.R., McCluggage W.G, Quinn D., Wylie J., McMenamin Ú.C. Concurrent and future risk of endometrial cancer in women with endometrial hyperplasia: A systematic review and meta-analysis. PLoS One. 2020;15(4):e0232231. https://dx.doi.org/10.1371/journal.pone.0232231.
- Zhao J., Hu Y., Zhao Y., Chen D, Fang T, Ding M. Risk factors of endometrial cancer in patients with endometrial hyperplasia: implication for clinical treatments. BMC Women's Health. 2021; 21: 312. https://dx.doi.org/10.1186/s12905-021-01452-9.
- Ашрафян Л.А., Антонова И.Б., Ивашина С.В., Бабаева Н.А., Алешикова О.А., Баранов И.И. Оптимизация диагностической тактики у пациенток с аномальными маточными кровотечениями в периоды пери и постменопаузы. Акушерство и гинекология: новости, мнения, обучение. 2019; 7(1): 24-30. [Ashrafyan L.A., Antonova I.B., Ivashina S.V., Babayeva N.A., Aleshikova O.A., Baranov I.I. Diagnostic tactics optimization in patients with abnormal uterine bleeding duringperi and postmenopause. Obstetrics and gynecology: News, opinions, training. 2019; 7(1): 24-30. (in Russian)].
- Фролова Ю.С., Елгина С.И. Сравнительная клинико-анамнестическая характеристика женщин с патологией эндометрия и полости матки, получивших помощь в амбулаторных и стационарных условиях. Мать и Дитя в Кузбассе. 2021; 2(85): 88-94. [Frolova Y.S., Elgina S.I. Comparative clinical and anamnestic characteristics of women with endometrial and uterine cavity pathology who received outpatient and inpatient care. Mother and Child in Kuzbass. 2021; 2(85): 88-94. (in Russian)]. https://dx.doi.org/10.24411/2686-7338-2021-10027.
- Амирасланов А.Т., Сафарова С.И. Факторы риска и прогностические показатели атипической гиперплазии эндометрия. Вестник современной клинической медицины. 2019; 12(2): 7-11. [Amiraslanov A.T., Safarova S.I. Risk factors and prognostic indicators of atypical endometrial hyperplasia. Bulletin of Modern Clinical Medicine. 2019; 12(2): 7-11. (in Russian)]. https://dx.doi.org/10.20969/VSKM.2019.12(2).7-11.
- Корниенко С.М. Факторы риска рецидивирования гиперпластических процессов эндометрия у женщин позднего репродуктивного и пременопаузального возраста. Репродуктивная эндокринология. 2017; 2(34): 28-31. [Kornienko S.M. Risk factors forrecurrence of endometrial hyperplastic processes in women of late reproductive and premenopausal age. Reproductive endocrinology. 2017; 2(34): 28-31 (in Russian)].
- Сулима А.Н., Колесникова И.О., Давыдова А.А., Кривенцов М.А. Гистероскопическая и морфологическая оценка внутриматочной патологии в разные возрастные периоды. Журнал акушерства и женских болезней. 2020; 69(2): 51-8. [Sulima A.N., Kolesnikova I.O., Davydova A.A., Kriventsov M.A. Hysteroscopic and morphological assessment of intrauterine pathology in different age periods. Journal of obstetrics and women’s diseases. 2020; 69(2): 51-8. (in Russian)]. https://dx.doi.org/10.17816/JOWD69251-58.
- Оразов М.Р., Хамошина М.Б., Мулина И.А., Артеменко Ю.С. Гиперплазия эндометрия – от патогенеза к эффективной терапии. Акушерство и гинекология: новости, мнения, обучение. 2021; 9(3): 21-8. [Orazov M.R., Khamoshina M.B., Mulina I.A., Artemenko Yu.S. Endometrial hyperplasia – from pathogenesis to effectivetherapy. Obstetrics and gynecology: News, opinions, training. 2021; 9(3): 21-8. (in Russian)]. https://dx.doi.org/10.33029/2303-9698-2021-9-3-21-28.
- Оразов М.Р., Радзинский В.Е., Аракелов С.Э., Хамошина М.Б., Носенко Е.Н., Духин А.О., Токтар Л.Р., Читанава Ю.С., Орехов Р.Е., Абитова М.З. Факторы риска гиперпластических процессов эндометрия у женщин в репродуктивном возрасте. Трудный пациент. 2019; 5(17): 19-21. [Orazov M.R., Radzinsky V.E., Arakelov S.E., Khamoshina M.B., Nosenko E.N., Duhin A.O., Toktar L.R., Chitanava Yu.S., Orekhov R.E., Abitova M.Z. Risk factors of endometrial hyperplasia in women of reproductive age. Difficult patient. 2019; 5(17): 19-21 (in Russian)]. https://dx.doi.org/10.24411/2074-1995-2019-10035.
- Подзолкова Н.М., Коренная В.В. Современные представления об этиологии, патогенезе и принципах лечения гиперплазии эндометрия. Акушерство и гинекология. 2021; 8: 192-9. [Podzolkova N.M., Korennaya V.V. Modern ideas about the etiology, thogenesis and principles of treatment of endometrial hyperplasia. Obstetrics and Gynecology. 2021; (8): 192-9 (in Russian)]. https://dx.doi.org/10.18565/aig.2021.8.192-199.
Received 10.04.2023
Accepted 27.10.2023
About the Authors
Yuliya S. Frolova, obstetrician-gynecologist, Kemerovo City Hospital No. 4, +7(923)5099116, beletskaya91@inbox.ru, https://orcid.org/0000-0002-6966-2081,650025, Russia, Kemerovo, Basovaya str., 12a.
Svetlana I. Elgina, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology named after G.A. Ushakova, Kemerovo State Medical University,
Ministry of Health of Russia, +7(905)0651613, Elginas.i@mail.ru, https://orcid.org/0000-0002-6966-2681, 650056, Russia, Kemerovo, Voroshilova str., 22a.
Corresponding author: Yuliya S. Frolova, beletskaya91@inbox.ru