Бесплодие является одной из самых сложных проблем в жизни семейной пары, имеющей негативные последствия для психического и социального благополучия вовлеченных лиц [1]. Бесплодные пары, в сравнении с фертильными, более склонны к депрессии, тревоге, потере чувства собственного достоинства и неудовлетворенности своей сексуальной жизнью [2–6]. У 50% пар, страдающих бесплодием, наблюдаются более высокий уровень стресса, тревоги, депрессии, более низкие показатели по шкалам психологического благополучия, удовлетворенности качеством жизни: у женщин с бесплодием выявлены расстройство адаптации в 50% случаев, легкая степень депрессии в 12–54% и тревожные расстройства в 12–23% случаев [7]. При бесплодии у женщин, в сравнении с мужчинами, наблюдаются более высокая личностная тревожность, также при женском факторе бесплодия обнаруживаются более тяжелые проявления депрессии [8, 9].
A.N. Yli-Kuha с соавт. (2010) сообщили о результатах сравнительного исследования психиатрической заболеваемости 9175 женщин, проходивших лечение по поводу бесплодия методами вспомогательных репродуктивных технологий (ВРТ) в Финляндии в 1996–1998 гг. Выявлено, что у них было меньше случаев госпитализации в связи с проявлениями тревоги, депрессии, психотическими синдромами, расстройствами личности, биполярным расстройством, нарушениями пищевого поведения, чем в контрольной группе [10]. Однако разница была статистически значимой только для расстройств психотического уровня. Различия в частоте госпитализаций сохранялись в течение последующих 10 лет наблюдения, за исключением повышенного риска госпитализации из-за расстройств адаптации. Также выявлено, что у родивших после лечения бесплодия женщин было меньше госпитализаций по поводу всех психиатрических заболеваний, чем у неродивших. Различия были статистически значимыми для тревожных расстройств, депрессии и употребления психоактивных веществ. Число госпитализаций у неродивших женщин с бесплодием было сопоставимо с данными контрольной группы, за исключением психотических расстройств, которых в контрольной группе было значимо больше [10]. T.K. Kjaer с соавт. (2011) провели сравнительное ретроспективное исследование суицидального риска у женщин с бесплодием [11]. Изучены данные когорты из 51 221 женщины с первичным и вторичным бесплодием, поставленных на учет за период 1973–1998 гг. Наблюдение проводилось до 2006 г. включительно. Выявлено, что у женщин, не родивших ни одного ребенка, в 2 раза выше суицидальный риск по сравнению с женщинами, родившими детей.
У женщин, страдающих бесплодием, отмечены менее стабильные супружеские отношения, чем у фертильных женщин [12]. Бездетность, обусловленная бесплодием, часто совпадает с провалом репродуктивных планов и способствует нарушению самоидентификации, негативному восприятию собственного тела, сомнениями в своей женственности и привлекательности для партнера [13]. Бесплодие является важным фактором, влияющим на сексуальное и диадическое функционирование [14]. У женщин с бесплодием выше распространенность сексуальных дисфункций, проявляющихся низкой сексуальной активностью, низким уровнем сексуального удовлетворения и снижением частоты сексуальных контактов. Сравнительное исследование сексуального здоровья женщин с первичным и вторичным типами бесплодия показало существенное превалирование сексуальных нарушений у женщин с вторичным бесплодием [15]. Значимые различия получены в отношении функции оргазма, уровня сатисфакции и общей оценки сексуальной функции. В целом уровень сексуального удовлетворения у женщин взаимосвязан с удовлетворенностью семейными отношениями [16].
Исследования доказали, что качество супружеских отношений – это значимый предиктор счастья и субъективного благополучия для обоих партнеров, а гармоничные супружеские отношения являются наиболее важным источником поддержки пары во время лечения бесплодия [17, 18].
Цель исследования: изучить особенности сексуального функционирования и психопатологической структуры сексуальных дисфункций у женщин с бесплодием в программах ВРТ для разработки лечебно-реабилитационных мероприятий и повышения качества жизни в паре.
Материал и методы исследования
Проведено открытое сплошное сравнительное описательное поперечное исследование сексуального функционирования, психопатологических особенностей и личностных характеристик 323 женщин, обратившихся в ФГБУ НЦАГиП им. В.И. Кулакова Минздрава России по поводу бесплодия для прохождения программ ВРТ в 2013–2016 гг. Критериями включения в исследование являлись отсутствие детей, женское бесплодие (МКБ-10 – N97), возраст женщин от 21 до 46 лет включительно, наличие постоянного партнера, согласие на участие в исследовании. Процедуры исследования были одобрены локальным этическим комитетом.
В исследовании применялись клинико-психопатологический, клинико-сексологический методы; использовались психометрические шкалы: опросник «Индекс женской сексуальной функции» (ИЖСФ) («Female Sexual Function Index» – FSFI); опросник выраженности психопатологической симптоматики «Symptom Check List-90-revised» (SCL-90-R); Мюнхенский личностный тест «Munich Personality Test» (МЛТ) [19–22].
Статистическая обработка данных проводилась в программе IBM SPSS версия 22. Различия между группами устанавливались при помощи Т-критерия Стьюдента при нормальном распределении и при помощи метода Манна–Уитни при не нормальном распределении. Результаты считались статистически значимыми при уровне значимости (p) меньше или равном 0,05.
Результаты исследования
Всего в исследовании приняли участие 653 пациентки с бесплодием (МКБ-10 – N97), 64 из них были исключены из исследования в связи с несоответствием критериям отбора. Проведен анализ результатов исследования 589 респондентов.
Средний возраст участниц исследования составил 33,81±6,20 года, высшее и незаконченное высшее образование имели 88,96% женщин, в официальном браке состояло 77,93% пациенток. Уточненный диагноз был представлен «женским бесплодием трубного происхождения» (N97.1) – 41,93%, «женским бесплодием, связанным с мужским фактором» (N97.4) – 22,24%, «женским бесплодием, связанным с отсутствием овуляции» (N97.0) – 19,52% и «другими формами женского бесплодия» (N97.8) – 16,31%. У 28,01% пациенток наблюдались сочетанные формы бесплодия, у 38,37% женщин бесплодие сочеталось с эндометриозом.
В ходе психопатологического исследования и структурированного клинического интервью у пациенток проводились оценка психического статуса и сексуального функционирования. Выявленные психические и сексуальные расстройства анализировались и квалифицировались в соответствии с диагностическими критериями МКБ-10, класса «Психические расстройства и расстройства поведения» (F00-F99) [23].
Согласно данным клинико-психопатологического обследования у 347 (58,9%), пациенток, включенных в исследование, выявлены психические расстройства непсихотического уровня. Они формировались на фоне длительного хронического стресса в связи с бесплодием, неудачными попытками его преодоления; служебных, семейных, финансовых трудностей; вследствие затрат большого количества времени на посещение лечебных учреждений и значительных материальных расходов при прохождении обследования и лечения. Психотравмирующими факторами, наряду с бесплодием, являлись дезадаптация межличностных отношений в связи с разочарованностью партнера текущими жизненными обстоятельствами. Кроме того, важным дезадаптирующим фактором было существенное изменение социального положения – уход с работы из-за невозможности совмещения с лечением, полная финансовая зависимость от партнера.
После проведенного клинико-сексологического обследования с использованием опросника ИЖСФ 589 пациенток, проходивших лечение по поводу бесплодия в отделении ВРТ, были разделены на три группы: 1-я группа – 108 человек с клинически выраженной сексуальной дисфункцией и общим баллом ИЖСФ ≤26,55; 2-я группа – 76 пациенток с латентными формами сексуальной дисфункции и общим баллом ИЖСФ ≤26,55, 3-я группа (сравнения) – 405 пациенток без сексуальных дисфункций с общим баллом ИЖСФ >26,55. На основании анализа полученных результатов были выявлены психические расстройства непсихотического уровня у пациенток с сексуальными дисфункциями (1-я группа) в 100% случаев, у пациенток с латентными формами сексуальных дисфункций (2-я группа) – в 75,0% случаев, а у пациенток без сексуальных расстройств (3-я группа, сравнения) – в 44,9% случаев; всего у 58,9% обследованных пациенток (табл. 1).
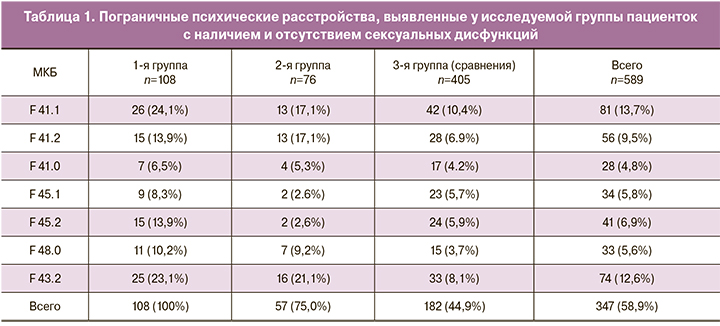
У всех пациенток с сексуальной дисфункцией (1-я группа) обнаруживались пограничные психические расстройства, синдромальная характеристика которых определялась в основном тревожно-астеническим, тревожно-депрессивным и тревожно-ипохондрическим вариантами в рамках невротических, связанных со стрессом и соматоформных расстройств (F4).
Таким образом, была выявлена высокая коморбидность сексуальных дисфункций и пограничных психических расстройств у женщин с бесплодием в программах ВРТ. Наличие у них сексуальных дисфункций свидетельствовало о выраженности психической дезадаптации и требовало особого внимания в организации мультидисциплинарной помощи с привлечением психотерапевта, сексолога.
Тревожные расстройства (F41) были выявлены у 28,0% исследованных пациенток (всего – 589 человек), из них генерализованное тревожное расстройство (F41.1) у 13,7%, смешанное тревожное и депрессивное расстройство (F41.2) у 9,5%, паническое расстройство (F41.0) у 4,8%. Сексуальные дисфункции у пациенток с тревожными расстройствами преимущественно имели вторичный характер, ведущим сексологическим расстройством являлось снижение либидо и нарушение оргазма. Пациентки высказывали жалобы на снижение интереса к половой жизни, вынужденный характер интимных отношений, утрату яркости сексуальных переживаний, утрату или невыразительность оргастических ощущений.
При недифференцированном соматоформном расстройстве (F45.1) (5,8%) у пациенток наблюдались разнообразные соматические феномены в различных частях тела, преимущественно алгические; среди них ведущей являлась тазовая боль, разной степени выраженности, не объяснявшаяся наличием заболеваний (например, эндометриозом) постоянная или связанная с менструацией, с дефекацией, с мочеиспусканием. Соматические феномены усиливались во время эмоционального напряжения при контактах с врачами, проведении процедур ВРТ, ожидании результатов, конфликтах с близкими. Сексологическая симптоматика также была разнообразной с вовлечением всех составляющих сексуальной функции – нарушения влечения и возбуждения, расстройства оргазма, нарушения генитальной реакции, гениталгии и сексуальная дисгармония в паре.
При ипохондрическом расстройстве (F45.2) у 6,9% пациенток обнаруживались выраженная фиксация на патологических телесных ощущениях, формирование идей о своем здоровье, сочетавшихся с тревожно-депрессивными нарушениями, сексуальной ангедонией. Гормональная подготовка в программах ВРТ, процедуры забора яйцеклеток, переноса эмбрионов в полость матки вызывали тягостные переживания, пациентки высказывали многочисленные жалобы на телесные сенсации, среди которых доминировали болевые ощущения внизу живота, гастроинтестинальные симптомы (вздутие живота, тошнота, нарушения стула). Для пациенток данной группы среди сексологических дисфункций было характерно формирование недостаточности генитальной реакции, глубокой и поверхностной форм диспареунии.
При неврастенических расстройствах (F48.0) у 5,6% пациенток наблюдались астенические проявления в виде общей слабости, эмоциональной неустойчивости, раздражительности, конфликтности, несдержанности, плаксивости, истощаемости, чувства беспомощности, а также нерезко выраженные симптомы тревоги, легкая степень депрессии. В отношениях с партнером у пациенток отмечалась постепенно нарастающая дистанцированность, дезадаптация межличностных отношений. Преобладающими сексуальными дисфункциями у пациенток данной группы были расстройства возбуждения и любрикации; следует отметить, что при этом не формировались выраженные болевые сексуальные дисфункции.
Расстройства адаптации (F43.2) обнаруживались у 12,6% пациенток, преимущественно в виде смешанной тревожной и депрессивной реакции, у 8,3% наблюдались психологические реакции тревожно-депрессивного спектра. Формирование расстройства происходило на фоне выраженного дистресса, связанного с обстоятельствами жизни, трудностями лечения бесплодия, недостаточностью материальных ресурсов, ухудшения межличностных отношений с партнером. Сексуальные дисфункции у пациенток данной группы возникали вторично, были кратковременными, преимущественно были представлены расстройствами либидо, возбуждения и оргазма.
Сексуальные дисфункции нозологического уровня были выявлены из 589 обследованных пациенток у 108 (18,34%), из них у 79,63% выявлено 1 сексуальное расстройство, у 22,37% – 2 и более (рис. 1).

Структура сексуальных дисфункций преимущественно была представлена изолированным расстройством либидо (F52.0) (25,0%), оргазма (13,9%) и сочетанным расстройством либидо с оргазмической дисфункцией (F52.3) (13,0%), диспареунией (F52.6) (5,6%). Сексуальная дисгармония в паре (34,3%) обнаруживалась реже, чем сексуальные дисфункции в совокупности. Это объяснялось сохранностью сексуальных отношений в паре на уровне потребностей партнера, что поддерживалось значимостью брака для пациенток и наличием у них удовлетворенности семейными отношениями.
Гениталгии были представлены поверхностной и глубокой диспареунией (26%), а также вагинизмом (11%). Глубокая диспареуния преобладала у пациенток с бесплодием на фоне эндометриоза. Особенности ее формирования состояли в том, что первоначально симптоматика была соматически обусловлена, болезненные проявления имели четко выраженный периодический характер, преимущественно перед менструацией. При отсутствии адекватного лечения эндометриоза в процессе половой жизни симптомы тазовой боли постепенно нарастали, особенно в периоды эмоционального напряжения, трудных жизненных ситуаций, межличностных конфликтов; усиливались, приобретали постоянный характер. Формирование хронической тазовой боли сопровождалось фиксацией пациенток на здоровье, постоянными обследованиями, поиском врачей, которые «смогут поставить правильный диагноз, вылечить», разочарованием, неудовлетворенностью и отрицанием пациентками психологических аспектов расстройства. Болевые ощущения при половой близости приводили к вторичному нарушению оргазмической функции, понижению либидо и снижению половой активности. Формировались невроз ожидания и уклоняющийся стиль поведения в интимной сфере. Нарастание симптоматики приводило к нарушению сексуальной адаптации в паре, что подтверждалось анализом сексуального функционирования партнера.
В ходе исследования было установлено, что наряду с клинически значимыми сексуальными расстройствами, можно выделить латентные формы сексуальных дисфункций, выявленные симптомы которых на момент обследования не вызывали стресс у пациенток – 76 (12,9%). Наличие симптомов сексуальной дисфункции было подтверждено анализом результатов опросника ИЖСФ (FSFI) – низких показателей по отдельным доменам и суммарному баллу (менее 26,55). Несмотря на низкие показатели при самооценке сексуального здоровья, дисгармоничных сексуальных отношений в паре пациентки отрицали наличие сексуального расстройства, либо затруднялись с ответом, демонстрировали низкую готовность обращения за сексологической помощью, за исключением случаев, когда возникали риски разрыва отношений, потери партнера. У остальных пациенток нарушения сексуального функционирования либо не было выявлены, либо проявлялись в виде адаптивной реакции на текущие жизненные обстоятельства, были кратковременными (не более трех месяцев), не вызывали стресс. Общий балл опросника ИЖСФ (FSFI), отражающий сексуальное функционирование за последние 4 недели, был выше 26,55, хотя по отдельным доменам могли быть низкие показатели, что свидетельствовало о наличии нарушений сексуальных реакций.
В группах пациенток с клинически выраженными (1-я группа) и латентными сексуальными расстройствами (2-я группа) по сравнению с группой без сексуальных дисфункций (3-я группа) выявлены достоверные различия по всем показателям ИЖСФ (FSFI): низкие уровни влечения, возбуждения, оргастичности и психологической сатисфакции, ухудшение сексуальной генитальной реакции, выраженность диспареунии (p<0,0001). Напротив, не выявлены значимые различия между 1-й и 2-й группой по всем доменам, за исключением различий на уровне тенденции по домену «любрикация» (рис. 2).
 Таким образом, клиническая (1-я) и латентная (2-я) группы отличались не степенью выраженности сексологической симптоматики, а наличием фрустрации в связи с сексуальной дисфункцией, значимостью сексуального функционирования, а также оценкой партнерской ситуации.
Таким образом, клиническая (1-я) и латентная (2-я) группы отличались не степенью выраженности сексологической симптоматики, а наличием фрустрации в связи с сексуальной дисфункцией, значимостью сексуального функционирования, а также оценкой партнерской ситуации.
При анализе преморбидных личностных характеристик пациенток с бесплодием в программах ВРТ по результатам МЛТ с использованием критерия U Манна–Уитни для независимых выборок в 1-й группе в сравнении с 3-й группой, показатели по доменам «экстроверсия» (p<0,000), «толерантность к фрустрации» (p<0,000) были достоверно ниже, по доменам «эзотерические тенденции» (p<0,044), «невротизм» (p<0,008) – достоверно выше, по домену «склонность к изоляции» (p<0,0057) – выше на уровне тенденции. Во 2-й группе в сравнении с 3-й группой показатель по домену «невротизм» был достоверно выше (p<0,028); по доменам «экстроверсия» – ниже, «склонность к изоляции» – выше на уровне тенденции (рис. 3).
На основании проведенного анализа результатов SCL-90 выявлены статистически значимые отличия между 1-й и 3-й группами по доменам «навязчивость», «сенситивность», «депрессия», «тревожность», «враждебность», «психотизм» и тенденции по доменам «фобия» и «паранояльность». Все показатели по доменам в 1-й группе были выше по сравнению с 3-й группой. Между 1-й и 2-й группами статистически значимые различия не выявлены. Обнаружены тенденции отличий между 2-й и 3-й группами по доменам «навязчивость», «сенситивность», «депрессия», «тревожность» и «фобия». При сравнении средних показателей нормы и данных в группах выявлены значимые отличия либо тенденции различий по всем доменам (табл. 2).

Обсуждение
Бесплодие накладывает психологическое бремя на супружеские пары. Тревога, депрессия, чувство беспомощности, неспособность к принятию, отсутствие социальной поддержки значительно повышают риск психической дезадаптации женщин с бесплодием, является одним из наиболее важных факторов, приводящих к разрыву семейных отношений, отказу от дальнейшего лечения [24, 25]. Проведенное исследование позволило изучить особенности сексуального функционирования, психопатологические и личностные характеристики 589 женщин, обратившихся в ФГБУ НЦАГиП им. В.И. Кулакова Минздрава России по поводу бесплодия для прохождения программ ВРТ в 2013–2017 гг.
Анализ полученных результатов показал, что 58,9% исследованных женщин страдали психическими расстройствами непсихотического уровня, среди них преобладали тревожные расстройства (28,0%). В ходе исследования было установлено, что наряду с сексуальными дисфункциями нозологического уровня (18,34%) выделяются латентные формы сексуальных дисфункций (12,9%), характеризовавшиеся отсутствием дистресса, несмотря на длительное наличие симптомов сексуальной дисфункции, подтвержденных анализом результатов опросника ИЖСФ. Пограничные психические расстройства выявлены у пациенток с клинически выраженными сексуальными дисфункциями в 100%, с латентными сексуальными дисфункциями в 75,0%, а у пациенток без сексуальных расстройств в 44,9% случаев, что убедительно демонстрирует высокую коморбидность сексуальных дисфункций и психических расстройств непсихотического уровня. Структура сексуальных дисфункций представлена изолированными и сочетанными формами женских сексуальных расстройств, среди них преобладало расстройство либидо (25,0%).
Проведенный анализ результатов у пациенток с клинически выраженными и латентными сексуальными дисфункциями в сравнении с пациентками без сексуальных расстройств показал достоверные различия по всем доменам опросника ИЖСФ: низкие уровни влечения, возбуждения, оргастичности и психологической сатисфакции, ухудшение сексуальной генитальной реакции, выраженность диспареунии (p<0,0001). Анализ преморбидных личностных характеристик и выраженности психопатологической симптоматики по результатам МЛТ и SCL-90 показал, что у пациенток с сексуальными расстройствами статистически значимо ниже показатели доменов «экстроверсия», «толерантность к фрустрации» и выше модальностей «эзотерические тенденции», «невротизм», «навязчивость», «сенситивность», «депрессия», «тревожность», «враждебность», «психотизм» (p<0,05).
Заключение
Таким образом, проведенное исследование позволило выявить у 58,9% из 589 исследованных пациенток с бесплодием в программах ВРТ психосоматические расстройства непсихотического уровня, среди них преобладали тревожные расстройства (28,0%); у 18,34% – сексуальные дисфункции нозологического уровня и у 12,9% латентные формы сексуальных дисфункций, среди которых преобладало расстройство либидо (25,0%). Установлена высокая коморбидность сексуальных дисфункций и психических расстройств непсихотического уровня (у пациенток с клинически выраженными сексуальными дисфункциями в 100% и с латентными сексуальными дисфункциями в 75,0% случаев против 44,9% у пациенток без сексуальных расстройств). Изученные особенности психопатологической структуры сексуальных дисфункций у женщин при бесплодии необходимы для разработки дифференцированной тактики проведения лечебно-реабилитационных мероприятий и повышения качества жизни в супружеской паре.