Prediction of reproductive outcomes in patients with deep endometriosis after surgical treatment
Objective. To assess the prognostic significance of the endometriosis fertility index (EFI) for predicting the chances of pregnancy after surgical treatment for infiltrative endometriosis.Safronova A.S., Buralkina N.A., Chuprynin V.D., Cheremin M.M.
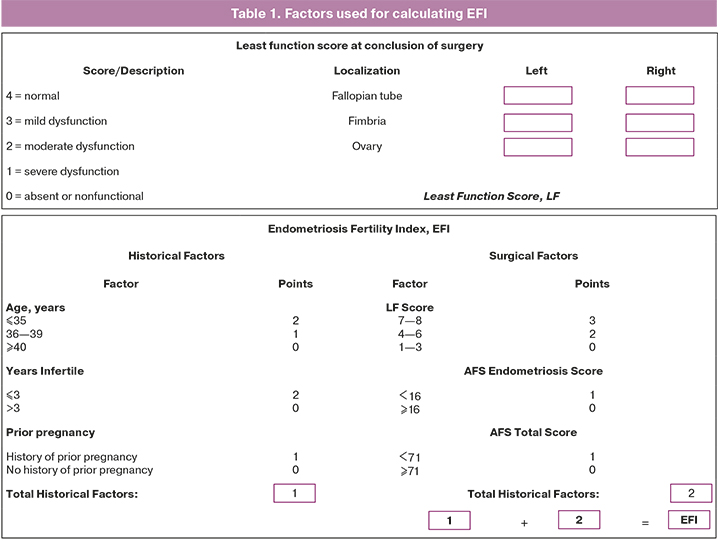
Materials and methods. This was a prospective cohort study carried out at the Department of Operative Gynecology and General Surgery at the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia (2018–2020). The study included 99 patients aged from 18 to 40 years with stage III–IV deep infiltrative endometriosis. All patients were divided into two groups: group I included patients who had deep endometriosis with colon lesions (n=63), group II – deep endometriosis without colon lesions (n=36). According to the objectives of the study, all patients were evaluated for the chances of pregnancy using EFI. The EFI parameters are presented in Table 1. Statistical analysis of the obtained data was carried out using the GraphPad Prism 9.0.0.121 software (USA).
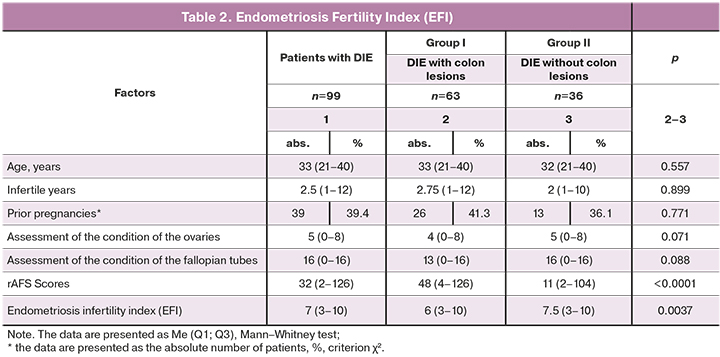
Results. The median EFI was 6 (3–10) in group I, and it was significantly lower than one in group II, namely, 7.5 (3–10), p=0.0037. There was a significant correlation between the EFI ratio and pregnancy (AUC=0.8049, p=0.0004). EFI was significantly higher in the group of patients who became pregnant compared to patients who did not get pregnant (7 versus 4, p=0.0002).
Conclusion. The patients planning pregnancy after surgery for deep infiltrative endometriosis are recommended to determine the EFI index as the most effective prognostic marker of pregnancy after surgery. If the EFI index is less than 5, patients should be recommended to undergo assisted reproduction due to the low probability of spontaneous pregnancy. If the EFI index is equal to or more than 5, patients can be recommended to conceive spontaneously within a period of 18 months after the operation. After 18 months, there is a significant decrease in the chances of spontaneous pregnancy, and therefore patients should be advised to undergo assisted reproduction.
Keywords
The problem of infertility in patients with endometriosis continues to be relevant nowadays. There are four types of endometriosis: peritoneal endometriosis, ovarian endometrioid cysts (endometrioma), deep endometriosis (DE) (previously known as deep infiltrative endometriosis or DIE), and adenomyosis [1–3]. Deep endometriosis is the most severe form of endometriosis, and according to some researchers, it occurs in about 1% of reproductive-aged women [4]. DIE is associated with pain syndrome in more than 95% of patients; the clinical manifestations of this syndrome are usually dysmenorrhea, non-cyclical pelvic pain, as well as deep dyspareunia [5]. Infertility complaints are reported by 30 to 50% of women with endometriosis [6–8]. The probability of spontaneous pregnancy in patients with deep endometriosis is about 10%.
In 2009, G. Adamson et al. proposed to use the Endometriosis Fertility Index (EFI) to predict the chance of conception following surgical treatment of endometriosis [4]. EFI makes it possible to predict the probability of conception based on the data obtained during the surgical intervention (the condition of the ovaries and fallopian tubes, the stage of endometriosis according to the rAFS classification) and the anamnestic data. The sum of the scores for each factor allows us to calculate the EFI coefficient, which varies from 0 to 10 scores, and can be used to assess the probability of pregnancy in patients with endometriosis-associated infertility after surgical treatment of endometriosis.
Materials and methods
This was a prospective cohort study which included 99 patients of reproductive age (from 18 to 40 years) with DIE: group I included patients who had DIE with colon lesions (n=63), group II consisted of patients with DIE without colon lesions (n=36).
The Endometriosis Fertility Index (EFI) was calculated for all patients on the basis of patient’s case history and data obtained intraoperatively. The assessment of reproductive outcomes in the postoperative period was carried out using a questionnaire that included the following questions: (1) about planning pregnancy after surgery; (2) if pregnancy occurred/did not occur after surgery; (3) how pregnancy occurred (spontaneously/after ART); (4) how long the postoperative period was prior to pregnancy; (5) about the outcome of pregnancy. The survey was followed by the interpretation of the obtained data and the evaluation of the prognostic value of the EFI score.
Statistical analysis
Statistical analysis of the obtained data was carried out using the GraphPad Prism 9.0.0.121 software (USA). The significance of the differences in quantitative indicators was assessed using the Mann–Whitney U-test. Quantitative data with a normal distribution are presented as the arithmetic mean (M) and standard deviation (SD). Non-normal distributions are given as the median (Me) and the interquartile interval (Q1; Q3), where Q1 and Q3 are the first and third quartiles. To compare the prevalence of variables in the groups of the study, the chi-square test (χ2), as well as chi-square test with Yates’ correction for low frequencies, are used. The results are presented as mean (standard deviation). The Kaplan–Meier method is used to make a curve of the cumulative pregnancy rate. The diagnostic value of the EFI score is determined on the basis of ROC analysis and AUC calculation. Differences are considered statistically significant at p <0.05 (95% confidence level).
Results
The average age of patients in groups I and II was 33 (30–36) years and 32 (29–36) years, respectively, without significant differences between the groups.
Taking into account the role of obesity [9, 10] and smoking [11] as possible independent factors of infertility, we conducted a comparative analysis of anthropometric parameters and anamnestic data of the patients. The average body mass index (BMI) in group I was 21 (20–23) kg/m2 and it was 20 (19–22) kg/m2 in group II; it did not differ significantly between the groups, p=0.06. Weight deficit (BMI<18.5 kg/m2) was observed in 11.1% (11/99) of patients with DIE. Nicotine dependence was revealed in 11.1% (7/63) and 5.6% (2/36) of women in groups I and II, respectively; the differences between the groups were not significant.
Among the previous gynecological surgical interventions, the percentage of previously performed ovarian resection in groups I and II was 61.9% (39/63) and 30.6% (11/36), respectively; it was significantly higher in patients with colorectal endometriosis. Also, previously performed operations for endometriosis were noted in the previous history of 46.5% of patients with DIE. They included 34.3% of patients who underwent a single surgical intervention and 12.1% of patients who had two or more interventions. The percentage of previously performed operations for endometriosis in patients with colorectal endometriosis was higher compared to patients of group II, and amounted to 60.3% and 22.2%, respectively (p=0.001).
 The next stage of the study was the analysis of the menstrual function in patients with DIE. Early menarche was found to occur in 1% of patients, later menarche was observed in 3%. The duration of the cycle in patients with DIE was 28 (28-29) days, the duration of menstruation was 5 (5–6) days. Profuse menstruation was noted in 54.5% of patients, moderate – 39.4%, scanty – 5.1%. On average, 70.0% of women in the study group reported complaints of pain in the lower abdomen.
The next stage of the study was the analysis of the menstrual function in patients with DIE. Early menarche was found to occur in 1% of patients, later menarche was observed in 3%. The duration of the cycle in patients with DIE was 28 (28-29) days, the duration of menstruation was 5 (5–6) days. Profuse menstruation was noted in 54.5% of patients, moderate – 39.4%, scanty – 5.1%. On average, 70.0% of women in the study group reported complaints of pain in the lower abdomen.
The analysis of the patients’ reproductive history revealed that 54% and 47% of women in groups I and II had pregnancies (p=0.662). The duration of infertility in both groups was 2.5 years (1–12) and it did not differ significantly between the groups. Primary infertility was noted in 35.4% of women with DIE, secondary infertility was found in 16.2% of patients. Pregnancy ended in full-term delivery in 31.7% of patients of group I and 25% of group II; induced abortions in early weeks gestation were noted in 7.9% and 8.3% of patients; missed abortions were reported in 6.3% and 8.3% of women, respectively. Unsuccessful IVF attempts were noted in the previous history of 7.1% of patients with DIE, concomitant male factor was observed in 2.0% of cases.
The main complaint of patients with DIE was pain in the lower abdomen, not related to the menstrual cycle (76.8%). Patients’ complaints of dysmenorrhea were less common – 41.4%, dyspareunia – 33.3% and loose stools during menstruation – 42.4%; the differences between the groups were not significant. Patients with colorectal endometriosis also complained of dyschesia (17.5%), flatulence (4.8%), blood admixture (9.5%) and the presence of mucus (6.3%) in the feces.
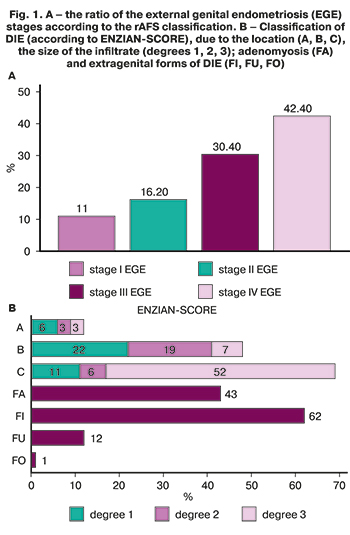
The assessment of endometriosis severity, its localization and the size of endometrioid foci was carried out on the basis of the rAFS classification and ENZIAN-SCORE. The percentage of patients with adenomyosis (FA) was 43%, intestinal endometriosis (FI) – 62%, ureteral endometriosis (FU) – 12%, another localization of endometriosis (anterior abdominal wall, FO) – 1% (Fig. 1).
The chances of pregnancy after surgery were estimated using EFI [12]. The factors which are used for calculating EFI are shown in Table 1.
The assessment of the EFI factors revealed no significant differences in age, the number of prior pregnancies, and the duration of infertility between the groups. However, rAFS Score (total score) was 4.4 times higher in patients with colorectal endometriosis (group I) compared to patients with DIE without bowel lesion (48 versus 11, p<0.0001), which was indicative of a more severe stage of endometriosis and adhesions. The median EFI was 6 (3–10) in group I, and it was significantly lower than one in group II, namely, 7.5 (3–10), p=0.0037 (Table 2).
The reproductive outcomes of patients with DIE were evaluated at the next stage of the study. The average duration of the postoperative period before pregnancy was 10.5 months (from 1 to 25 months) in the group of patients with DIE who planned pregnancy after surgery. The total percentage of the pregnancy rate in patients with DIE was 40.4%. In the group of patients with colorectal endometriosis, this indicator was equal to (11/31) 35.5%, which was lower compared to the group of patients with DIE without colon lesion, where this indicator was 47.1%; the differences between the groups were not significant. Spontaneous pregnancy occurred in 73.7% (14/19) of cases, and pregnancy after ART treatment occurred in 26.3% (5/19) of cases. The results of the study showed no significant differences between the subgroups in the duration of the postoperative period before pregnancy and how pregnancy occurred.
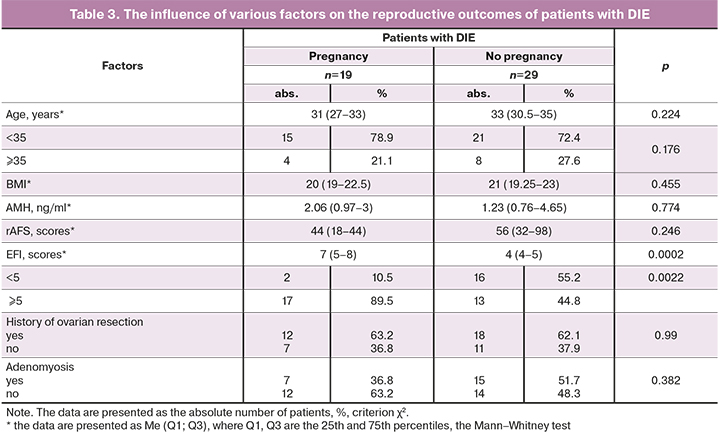
There was an analysis of factors affecting the pregnancy rate in patients with DIE. Age, BMI, AMH level, stage of external genital endometriosis (EGE), and adenomyosis did not influence the chance of conception in patients with DIE after the surgical treatment (Table 3).
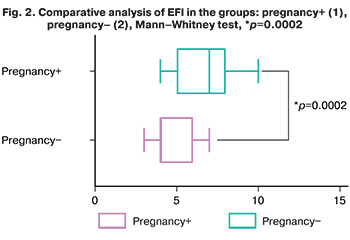 A significantly higher EFI score was observed in the group of patients who became pregnant compared to the patients who did not become pregnant (7 versus 4), p=0.0002 (Fig. 2).
A significantly higher EFI score was observed in the group of patients who became pregnant compared to the patients who did not become pregnant (7 versus 4), p=0.0002 (Fig. 2).
The evaluation of the prognostic value of the EFI score for assessing the pregnancy rate in patients with DIE was carried out on the basis of ROC analysis. EFI has been shown to be highly sensitive to the onset of pregnancy (AUC=0.8049, p=0.0004) (Fig. 3).
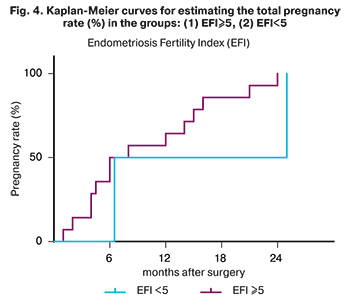
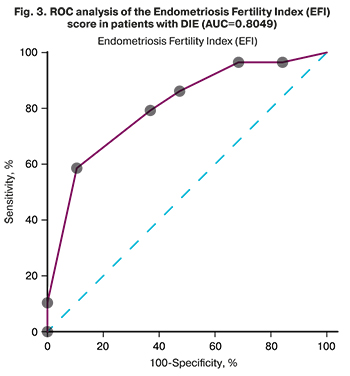 According to the results of the ROC analysis for the EFI score, the best cut–off value was 5.5 scores (sensitivity – 79.3%, specificity – 63.2%; 95% CI: 0.6796–0.9302). We classified all cases into two groups on the basis of the data obtained: EFI ≥ 5 scores and EFI <5 scores. The total pregnancy rate in the groups with EFI<5 and EFI≥5 was estimated using the Kaplan–Meier method (Fig. 4). This indicator in the group of patients with EFI<5 did not exceed 50% within 24 months after surgery, while the indicator for EFI≥5 was 84.2% in 18 months after surgery. The total pregnancy rate in patients with EFI≥5 without the ART treatment during the first 6, 12 and 18 months after surgery was 31.6%, 52.6% and 68.4%; pregnancy rate in patients who underwent ART was 31.6%, 57.9% and 84.2%, respectively.
According to the results of the ROC analysis for the EFI score, the best cut–off value was 5.5 scores (sensitivity – 79.3%, specificity – 63.2%; 95% CI: 0.6796–0.9302). We classified all cases into two groups on the basis of the data obtained: EFI ≥ 5 scores and EFI <5 scores. The total pregnancy rate in the groups with EFI<5 and EFI≥5 was estimated using the Kaplan–Meier method (Fig. 4). This indicator in the group of patients with EFI<5 did not exceed 50% within 24 months after surgery, while the indicator for EFI≥5 was 84.2% in 18 months after surgery. The total pregnancy rate in patients with EFI≥5 without the ART treatment during the first 6, 12 and 18 months after surgery was 31.6%, 52.6% and 68.4%; pregnancy rate in patients who underwent ART was 31.6%, 57.9% and 84.2%, respectively.
Discussion
 Endometriosis Fertility Index (EFI) has been used to evaluate the pregnancy rate by a number of authors. This indicator varies from 0 to 10 and can be used to predict pregnancy after surgical treatment of endometriosis [13–16]. According to the study conducted by S. Maheux-Lacroix et al. (2017), women with stage III–IV endometriosis and the EFI score > 7 have a chance for live birth of a child conceived without ART after surgery in about 60% of cases after 3 years and in 75% of cases after 5 years [17]. However, if the EFI score is ≤ 2, the probability of pregnancy with a wait-and-see approach is very low (from 0 to 10%); therefore, it is recommended to perform ART in the early postoperative period in this group of women. But even despite the ART treatment, the rate of live births in women in this group remains less than 40%, what women should be informed about when undergoing the treatment.
Endometriosis Fertility Index (EFI) has been used to evaluate the pregnancy rate by a number of authors. This indicator varies from 0 to 10 and can be used to predict pregnancy after surgical treatment of endometriosis [13–16]. According to the study conducted by S. Maheux-Lacroix et al. (2017), women with stage III–IV endometriosis and the EFI score > 7 have a chance for live birth of a child conceived without ART after surgery in about 60% of cases after 3 years and in 75% of cases after 5 years [17]. However, if the EFI score is ≤ 2, the probability of pregnancy with a wait-and-see approach is very low (from 0 to 10%); therefore, it is recommended to perform ART in the early postoperative period in this group of women. But even despite the ART treatment, the rate of live births in women in this group remains less than 40%, what women should be informed about when undergoing the treatment.
Conclusion
The patients planning pregnancy after surgery for deep infiltrative endometriosis are recommended to determine the EFI score as the most effective prognostic marker of pregnancy after surgery. If the EFI score is less than 5, patients should be recommended to undergo assisted reproduction due to the low probability of spontaneous pregnancy. If the EFI score is equal to or more than 5, patients can be recommended to conceive spontaneously within a period of 18 months after the operation. After the above-mentioned period there is a significant decrease in the chances of spontaneous pregnancy, and therefore patients should be advised to undergo assisted reproduction.
References
- Keckstein J., Becker C.M., Canis M., Feki A., Grimbizis G.F., Hummelshoj L.; Working group of ESGE, ESHRE, and WES. Recommendations for the surgical treatment of endometriosis. Part 2: deep endometriosis. Hum. Reprod. Open. 2020; 2020(1): hoaa002. https://dx.doi.org/10.1093/hropen/hoaa002.
- Keckstein J., Hudelist G. Classification of deep endometriosis (DE) including bowel endometriosis: From r-ASRM to #Enzian-classification. Best Pract. Res. Clin. Obstet. Gynaecol. 2021; 71: 27-37. https://dx.doi.org/10.1016/j.bpobgyn.2020.11.004.
- Keckstein J., Ulrich U., Possover M., Schweppe K.W. ENZIAN-Klassifikation der tief infiltrierenden Endometriose. Zentralbl. Gynäkol. 2003; 125: 291.
- Berlanda N., Somigliana E., Frattaruolo M.P., Buggio L., Dridi D., Vercellini P. Surgery versus hormonal therapy for deep endometriosis: is it a choice of the physician? Eur. J. Obstet. Gynecol. Reprod. Biol. 2017; 209: 67-71. https://dx.doi.org/10.1016/j.ejogrb.2016.07.513.
- Ballard K.D., Seaman H.E., de Vries C.S., Wright J.T. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study – Part 1. BJOG. 2008; 115(11): 1382-91. https://dx.doi.org/10.1111/j.1471-0528.2008.01878.x.
- Evans B.M., Decherney A.H. Fertility and endometriosis. Clin. Obstet. Gynecol. 2017; 60(3): 497-502. https://dx.doi.org/10.1097/GRF.0000000000000295.
- Ярмолинская М.И., Айламзян Э.К. Генитальный эндометриоз. Различные грани проблемы. СПб.: Эко-Вектор; 2017. [Yarmolinskaya M.I., Aylamzyan E.K. Genital endometriosis. Different facets of the problem. St. Petersburg: Eco-Vector; 2017. (in Russian)].
- Краснопольская К.В. Лечение бесплодия при эндометриозе: взгляд репродуктолога. М.: МЕДпресс-информ; 2019. [Krasnopolskaya K.V. Treatment of infertility in endometriosis: the look of a reproductologist. M.: MEDPress-inform, 2019. (in Russian)].
- Broughton D.E., Moley K.H. Obesity and female infertility: potentional mediators of obesity's impact. Fertil. Steril. 2017; 107(4): 840-7. https://dx.doi.org/10.1016/j.fertnstert.2017.01.017.
- Shah D.K., Correia K.F., Vitonis A.F., Missmer S.A. Body size and endometriosis: results from 20 years of follow-up within the Nurses’ Health Study II prospective cohort. Hum. Reprod. 2013l; 28(7): 1783-92. https://dx.doi.org/10.1093/humrep/det120.
- Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil. Steril. 2018; 110(4): 611-8. https:/dx.doi.org/10.1016/j. fertnstert.2018.06.016.
- Adamson G.D., Pasta D.J. Endometriosis fertility index: the new, validated endometriosis staging system. Fertil. Steril. 2010; 94(5): 1609-15. https:/dx.doi.org/10.1016/j.fertnstert.2009.09.035.
- Tomassetti C., Geysenbergh B., Meuleman C., Timmerman D., Fieuws S., D'Hooghe T. External validation of the endometriosis fertility index (EFI) staging system for predicting non-ART pregnancy after endometriosis surgery. Hum. Reprod. 2013; 28(5): 1280-8. https://dx.doi.org/10.1093/humrep/det017.
- Cohen J., d’Argent E.M., Selleret L., Antoine J.M. Endometriose profonde et fertilite. Presse Med. 2017; 46: 1184-91. https://dx.doi.org/10.1016/j.lpm.2017.10.002.
- Boujenah J., Bonneau C., Hugues J.N., Sifer C., Poncelet C. External validation of the Endometriosis Fertility Index in a French population. Fertil. Steril. 2015; 104(1): 119-23. e1. https:/dx.doi.org/10.1016/j.fertnstert.2015.03.028.
- Wei D.M., Yu Q., Sun A.J., Tian Q.J., Chen R., Deng C.Y. et al. Relationship between endometriosis fertility index and pregnancies after laparoscopic surgery in endometriosis-associated infertility. Zhonghua Fu Chan Ke Za Zhi. 2011; 46(11): 806-8.
- Maheux-Lacroix S., Nesbitt-Hawes E., Deans R., Won H., Budden A., Adamson D., Abbott J.A. Endometriosis fertility index predicts live births following surgical resection of moderate and severe endometriosis. Hum. Reprod. 2017; 32(11): 2243-9. https://dx.doi.org/10.1093/humrep/dex291.
Received 19.04.2021
Accepted 13.07.2021
About the Authors
Anastasia S. Safronova, doctor, Surgical Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,Ministry of Health of the Russian Federation. E-mail: doc_safronova@mail.ru. ORCID: 0000-0002-5962-1165. 117997, Russia, Moscow, Academician Oparin str., 4.
Natalya A. Buralkina, MD, DSc, Senior Researcher, Surgical Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: natalyaburalkina@yandex.ru. ORCID: 0000-0001-5109-6725.
117997, Russia, Moscow, Academician Oparin str., 4.
Vladimir D. Chuprynin, Candidate of Medical Sciences, Head of the Surgical Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: v_chuprynin@oparina4.ru. ORCID: 0000-0002-2997-9019.
117997, Russia, Moscow, Academician Oparin str., 4.
Mikhail M. Cheremin, resident obstetrician-gynecologist, N.V. Sklifosovsky Research Institute of Emergency Medicine, Department of Health of the City of Moscow. E-mail: mkhrznt@gmail.com. 129090, Russia, Moscow, Bolshaya Sukharevskaya sqr., 3.
For citation: Safronova A.S., Buralkina N.A., Chuprynin V.D., Cheremin M.M. Prediction of reproductive outcomes in patients with deep endometriosis after surgical treatment.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2021; 7: 158-164 (in Russian)
https://dx.doi.org/10.18565/aig.2021.7.158-164



