В современной гинекологии широко применяются лазерные технологии в лечении стрессового недержания мочи, смешанного типа недержания мочи, синдрома релаксированного влагалища, пролапса тазовых органов I и II степени и вульвовагинальной атрофии. Стрессовое недержание мочи является самой распространенной формой недержания мочи у женщин и проявляется непроизвольной потерей мочи при превышении внутрипузырного давления над внутриуретральным, что бывает при чихании, кашле, смехе, физических упражнениях или при изменении положения тела [1–3]. Проявлением ургентного недержания мочи является непроизвольное выделение мочи, возникающее сразу после внезапного непреодолимого позыва к мочеиспусканию. Когда проявляются симптомы обеих форм недержания, такой тип недержания называется смешанным [4, 5]. Генитальный пролапс является распространенной патологией среди пациенток репродуктивного и перименопаузального возраста. Пролапс тазовых органов существенно снижает качество жизни вследствие возникновения мочевой, аноректальной и сексуальной дисфункций. Наиболее распространенным симптомом при генитальном пролапсе является ощущение выпячивания стенки влагалища, а также чувство инородного тела в промежности [6–8].
В настоящее время для коррекции генитоуринарных расстройств применяются два типа лазеров: углекислый (СО2) лазер и эрбиевый (Er:YAG) лазер. Эрбиевый лазер имеет длину волны 2940 нм, глубина проникновения в биоткань составляет не более 0,05 мм (50 мкм) [9–11]. СО2-лазер излучает волну в 10 600 нм и имеет очень высокий уровень поглощения водой, а значит и биотканями [12]. В результате действия лазерного излучения на ткани укорачиваются межмолекулярные поперечные связи тройной спирали коллагена, что приводит к мгновенному сокращению волокон на две трети их длины, запускаются механизмы неоколлагенеза [13–15]. Длительность положительного эффекта от процедур определяется индивидуально, в среднем составляет до одного года [1, 2, 16].
Материал и методы исследования
В проведенном нами клиническом исследовании принимали участие 72 пациентки. На момент окончания исследования и проведения статистической обработки данных в исследуемую группу входили 65 пациенток. 7 пациенток были исключены из исследования ввиду неявки на все запланированные лечебные сеансы по причине личных обстоятельств. Критерием включения пациенток в исследование являлось наличие следующих диагнозов: пролапс тазовых органов I–II степени, смешанный тип недержания мочи, стрессовое недержание мочи, вульвовагинальная атрофия. Среди пациенток данной группы 52 имели в анамнезе роды, впоследствии способствовавшие развитию синдрома релаксированного влагалища. Средний возраст пациенток исследуемой группы составлял 44±4,1 года. Основными жалобами являлись: недержание мочи при кашле, смехе, чихании, физической активности, учащенное мочеиспускание, чувство неполного опорожнения мочевого пузыря, чувство давления в нижних отделах живота, недержание мочи вследствие сильного позыва к мочеиспусканию, потеря мочи по каплям, чувство засасывания воздуха во влагалище и дискомфорт при половом контакте, ощущение сухости слизистой оболочки вульвы и влагалища.
Перед началом лечения всем пациенткам проводился гинекологический осмотр, цитологическое исследование мазков на степень чистоты влагалища и наличие атипичных клеток, ультразвуковое исследование органов малого таза. Учитывая, что вопросы недержания мочи, неприятных ощущений во влагалище и неудовлетворенность качеством сексуальной жизни являются достаточно интимным для большинства пациенток, нами была проведена беседа с каждой из них перед началом лечения, где в доступной форме было разъяснено, для чего нужна процедура лазерного воздействия, как будет проходить курс лечения, и какие результаты мы планируем достигнуть.
 В ходе исследования было проведено анкетирование пациенток до начала лечения и при каждом лечебном сеансе, для чего использовали специализированный международный опросник PFDI-20 – Pelvic Floor Disorders Distress Inventory [17]. PFDI-20 состоит из трех подразделов: CRAD-8 (ColoRectal-Anal Distress Inventory) для оценки отдельных симптомов расстройств нижних отделов желудочно-кишечного тракта, POPDI-6 (Pelvic Organ Prolapse Distress Inventory) для выявления симптомов пролапса органов малого таза и UDI-6 (Urinary Distress Inventory) для оценки расстройств мочевыделительной системы. На каждый вопрос пациентка может дать один их четырех вариантов ответа, оцениваемый в баллах, характеризующих степень выраженность данного симптома: 0 баллов – «нет», 1 балл – «иногда», 2 балла – «редко», 3 балла – «часто», 4 балла – «всегда». Максимальное количество баллов по каждому подразделу составляет от 0 до 100, по опроснику PFDI-20 – 300 баллов. Для подсчета индекса сексуальной функции у женщин мы использовали международный опросник FSFI – Female Sexual Function Index [18], состоящий из 19 вопросов, где максимальное количество баллов составляет 36. Ввиду того, что не все пациентки вели половую жизнь, то опросник FSFI был использован у 59 из 65 пациенток.
В ходе исследования было проведено анкетирование пациенток до начала лечения и при каждом лечебном сеансе, для чего использовали специализированный международный опросник PFDI-20 – Pelvic Floor Disorders Distress Inventory [17]. PFDI-20 состоит из трех подразделов: CRAD-8 (ColoRectal-Anal Distress Inventory) для оценки отдельных симптомов расстройств нижних отделов желудочно-кишечного тракта, POPDI-6 (Pelvic Organ Prolapse Distress Inventory) для выявления симптомов пролапса органов малого таза и UDI-6 (Urinary Distress Inventory) для оценки расстройств мочевыделительной системы. На каждый вопрос пациентка может дать один их четырех вариантов ответа, оцениваемый в баллах, характеризующих степень выраженность данного симптома: 0 баллов – «нет», 1 балл – «иногда», 2 балла – «редко», 3 балла – «часто», 4 балла – «всегда». Максимальное количество баллов по каждому подразделу составляет от 0 до 100, по опроснику PFDI-20 – 300 баллов. Для подсчета индекса сексуальной функции у женщин мы использовали международный опросник FSFI – Female Sexual Function Index [18], состоящий из 19 вопросов, где максимальное количество баллов составляет 36. Ввиду того, что не все пациентки вели половую жизнь, то опросник FSFI был использован у 59 из 65 пациенток.
При каждом приеме мы проводили измерение силы мышц тазового дна с помощью системы PMTx с биологической обратной связью, состоящей из манометра со шкалой из 12 делений, воздухопроводящей трубки и резинового цилиндрического конуса. Измерение силы тазовых мышц выполняется в течение 5 секунд. Для оценки подвижности уретры и шейки мочевого пузыря использовали Q-tip тест (тест прямого катетера). Пациенткам с пролапсом гениталий во время натуживания на гинекологическом кресле определяли степень выраженности пролабирования передней и задней стенок влагалища. Больным со стрессовым недержанием мочи при осмотре на гинекологическом кресле проводили пробу кашлевого толчка. До и после лечения пациенткам было проведено ультразвуковое исследование с цветовым допплеровским картированием для оценки состояния кровоснабжения стенок влагалища и соноэластография в режиме реального времени на аппарате Toshiba Aplio 500 для определения жесткости тканей. Согласие на участие в исследовании было получено от всех пациенток. Статистическая обработка данных проводилась с помощью программы Statistica 10.
Мы провели оценку данных литературы о применении эрбиевого лазера в лечении генитоуринарных расстройств. Ряд зарубежных авторов, таких как U.B. Ogrinc и соавт. (2015) [1], M. Gambacciani и соавт. (2015) [19], P. Gaviria и соавт. (2016) [20], N. Fistonić и соавт. (2016) [21] и некоторые другие проводили лечение стрессового и смешанного типов недержания мочи, синдрома релаксированного влагалища, вульвовагинальной атрофии у пациенток, как в репродуктивном, так и в постменопаузальном периоде, применяя от 1 до 4 процедур лазерного воздействия с интервалом 15–30 дней, ориентируясь на клиническую ситуацию. Отечественные авторы А.А. Коваль, А.А. Безменко (2015), Г.А. Лапий, А.И. Неймарк и соавт. (2016) [13, 22] проводили лечение стрессового недержания мочи и генитального пролапса минимум двумя процедурами с интервалом от 21 до 45 дней. Многие исследователи отмечают, что при недостаточном эффекте возможно проведение большего количества процедур спустя тот же временной промежуток до момента достижения желаемого результата. В нашем исследовании при решении вопроса о количестве процедур мы опирались на данные литературы, объективного обследования (опросники, соноэластография, перинеометрия, гинекологический осмотр), а также субъективные ощущения пациенток.
Исследование проводилось в период с 10.09.2015 г. по 30.03.2016 г. Всем пациенткам было проведено лечение эрбиевым лазером (Er:YAG-лазер с длиной волны 2940 нм) процедурами IncontiLase и IntimaLase с технологией Fotona Smooth на аппарате SP Spectro (Fotona, Словения) согласно последовательности, запатентованной производителем. 65 пациенткам были проведены 4 сеанса воздействия лазерным излучением с интервалом в 28 дней. Каждая процедура состоит из нескольких этапов. На первом этапе лазерная энергия подается по всей окружности стенок влагалища через широкопольный излучатель с 360-градусной насадкой с распределением около 650 Дж лазерной энергии. На втором этапе процедуры используется угловая 90-градусная насадка для формирования во фракционированном SMOOTH-режиме пучки излучения для воздействия на стенки влагалища. Передняя стенка облучается фракционированным пучком в несколько продольных проходов. На этом этапе распределяется около 250 Дж энергии. На третьем этапе используется излучатель с прямым наконечником для работы в области преддверия влагалища и наружного отверстия уретры фракционированным пучком в SMOOTH-режиме, где распределяется около 100 Дж энергии. Таким образом, около 1000 Дж энергии расходуется для выполнения одного сеанса. В соответствии с данными зарубежной [19–21] и отечественной [13] литературы используемая в исследованиях плотность потока энергии составляла от 3 до 10 Дж/см2. Оптимальной и рекомендованной производителем плотностью потока для выполнения процедуры лечения является 10 Дж/см2, но при высокой степени индивидуальной чувствительности энергия импульсов может быть снижена, что не противоречит принципу доставки лазерной энергии SMOOTH и не снижает степень эффективности метода. Лазерное воздействие является минимально инвазивным в виде плавных последовательностей импульсов с акцентом на переднюю стенку влагалища, которая интимно связана с мочевым пузырем и мочеиспускательным каналом и обладает меньшей чувствительностью по сравнению с областью преддверия влагалища и периуретральной областью. В нашем исследовании в ходе лечения энергия импульсов при воздействии на переднюю стенку влагалища составляла в среднем 8–10 Дж/см2, на боковую и заднюю стенки влагалища – 6–8 Дж/см2, на область наружного отверстия уретры – 3–4 Дж/см2. Длительность одной процедуры составляла 10–15 минут. Во время проведения процедуры контролировался уровень дискомфорта пациенток, болевые ощущения, а также потенциальные побочные эффекты. Анестезия не использовалась. В процессе лечения мы увеличивали энергию лазерных импульсов с каждой последующей процедурой на 1–2 Дж/см2 с целью приближения к рекомендуемой плотности потока энергии – 10 Дж/см2. При проведении исследования нами было отмечено, что у пациенток перименопаузального периода имеется повышенная чувствительность в области влагалища и вульвы, а также дискомфорт и жалобы во время проведения лечения чаще, чем у молодых пациенток, что обусловлено гипоэстрогенией, дистрофическими и атрофическими процессами слизистой оболочки данной области. Поэтому у пациенток перименопаузального периода применялись импульсы меньшей энергии, чем у пациенток репродуктивного возраста. Более половины пациенток оценили процедуры IncontiLase и IntimaLase как совершенно безболезненные, тогда как другие отмечали ощущение жжения во время обработки области преддверия влагалища. Этот дискомфорт исчезал во время паузы между последовательными лазерными импульсами. Все пациентки возвращались к повседневной активности сразу после процедуры.
Результаты исследования
Частота встречаемости симптомов в исследуемой группе
Определение значимости различий показателей частоты встречаемости симптомов у пациенток исследуемой группы (n=65) до и после лечения по данным подразделов опросника PFDI-20 проводилось с помощью критерия χ2 по методу Мак-Немара. По данным подраздела POPDI до начала лечения такие симптомы, как чувство давления в нижних отделах живота и чувство неполного опорожнени мочевого пузыря являлись наиболее часто встречаемыми и выявлялись в равной мере (n=37, 57%). Вторым по частоте встречаемости симптомом была тяжесть в области таза (n=25, 38%). Также пациенток беспокоили чувство выпадения инородного тела из влагалища (n=21, 33%), необходимость вправить влагалище или часть прямой кишки для полного опорожнения кишечника (n=12, 19%) или для начала мочеиспускания или полного опорожнения мочевого пузыря (n=3, 5%). После проведения терапии эрбиевым лазером выявлено статистически значимое снижение частоты встречаемости таких симптомов, как чувство давления в нижних отделах живота (n=28, 44%, р=0,0077), тяжесть в области таза (n=17, 26%, р=0,0133) и чувство неполного опорожнени мочевого пузыря (n=27, 42%, р=0,0044). Степень выраженности других проявлений пролапса тазовых органов до и после лечения не показали статистически значимых различий.
 Проявления дисфункции нижних отделов желудочно-кишечного тракта мы оценили по данным подраздела СRAD. До начала терапии наиболее часто встречалось чувство неполного опорожнения кишечника после дефекации (n=44, 67%), эпизоды недержания газов и необходимость сильного натуживания для опорожнения кишечника встречались в равной степени (n=37, 57%). Также встечались такие симптомы, как боль при дефекации (n=16, 24%) и эпизоды недержания кала при жидком стуле (n=12, 19%). После проведенного лечения отмечено снижение частоты встречаемости симптомов дисфункции нижних отделов желудочно-кишечного тракта, а именно таких, как чувство неполного опорожнения кишечника после дефекации (n=41, 63%, р=0,2482), эпизоды недержания газов (n=35, 55%, р=1,0), необходимость сильного натуживания для опорожнения кишечника (n=34, 52%, р=0,2482), боль при дефекации (n=7, 10%, р=0,1336) и эпизоды недержания кала при жидком стуле (n=6, 9%, р=0,4795), но не выявлено статистически значимых различий. Незначительное уменьшение симптомов дисфункции нижних отделов желудочно-кишечного тракта, вероятнее всего, связано с явлениями неоколлагенеза и улучшением тургора тканей в данной области после проведния курса лечения.
Проявления дисфункции нижних отделов желудочно-кишечного тракта мы оценили по данным подраздела СRAD. До начала терапии наиболее часто встречалось чувство неполного опорожнения кишечника после дефекации (n=44, 67%), эпизоды недержания газов и необходимость сильного натуживания для опорожнения кишечника встречались в равной степени (n=37, 57%). Также встечались такие симптомы, как боль при дефекации (n=16, 24%) и эпизоды недержания кала при жидком стуле (n=12, 19%). После проведенного лечения отмечено снижение частоты встречаемости симптомов дисфункции нижних отделов желудочно-кишечного тракта, а именно таких, как чувство неполного опорожнения кишечника после дефекации (n=41, 63%, р=0,2482), эпизоды недержания газов (n=35, 55%, р=1,0), необходимость сильного натуживания для опорожнения кишечника (n=34, 52%, р=0,2482), боль при дефекации (n=7, 10%, р=0,1336) и эпизоды недержания кала при жидком стуле (n=6, 9%, р=0,4795), но не выявлено статистически значимых различий. Незначительное уменьшение симптомов дисфункции нижних отделов желудочно-кишечного тракта, вероятнее всего, связано с явлениями неоколлагенеза и улучшением тургора тканей в данной области после проведния курса лечения.
При анализе данных подраздела UDI наиболее часто у пациенток до лечения встречался такой симптом, как недержание мочи вследствие сильного позыва к мочеиспусканию (n=49, 76%), которое в самостоятельной форме не выявлялось, а всегда сопровождалось явлениями стрессового недержания мочи, вульвовагинальной атрофии и генитального пролапса. На втором месте – учащенное мочеиспускание (n=40, 62%), потеря мочи в незначительных количествах (n=37, 57%). Недержание мочи при кашле, смехе, чихании, а также боль или дискомфорт в нижних отделах живота встречались в равной степени (n=31, 48%), реже выявлялось затруднение опорожнения мочевого пузыря (n=25, 38%). Среди пациенток исследуемой группы смешанная форма недержания мочи встречалась чаще (n=24, 36%), чем стрессовое недержание (n=7, 11%). При оценке результатов выявлено статистически значимое снижение частоты встречаемости всех вышеуказанных симптомов после лечения по сравнению с данными до начала терапии (p<0,05).
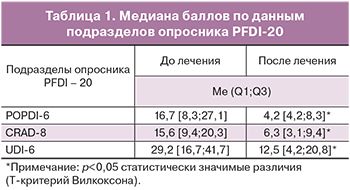
Оценка баллов по опроснику PFDI-20
Улучшение отмечено у 60 (92%) из 65 пациенток после проведения четырех процедур лечения лазером. При анализе результатов опросника PFDI-20 мы видим постепенное уменьшение общей медианы баллов с каждым лечебным сеансом. Нами выявлено статистически значимое улучшение качества жизни по сравнению с данными до лечения (Т-критерий Вилкоксона, p<0,05) (рис. 1).
 При детальном анализе опросника установлено статистически значимое снижение медианы баллов по всем трем подразделам, что говорит о значительном улучшении состояния пациенток, а также о снижении проявлений стрессового и смешанного типов недержания мочи и генитального пролапса после проведения четырёх сеансов терапии лазером. В табл. 1 представлены медианы баллов и ИКД подразделов POPDI-6, CRAD-8, UDI-6 до и после лечения.
При детальном анализе опросника установлено статистически значимое снижение медианы баллов по всем трем подразделам, что говорит о значительном улучшении состояния пациенток, а также о снижении проявлений стрессового и смешанного типов недержания мочи и генитального пролапса после проведения четырёх сеансов терапии лазером. В табл. 1 представлены медианы баллов и ИКД подразделов POPDI-6, CRAD-8, UDI-6 до и после лечения.
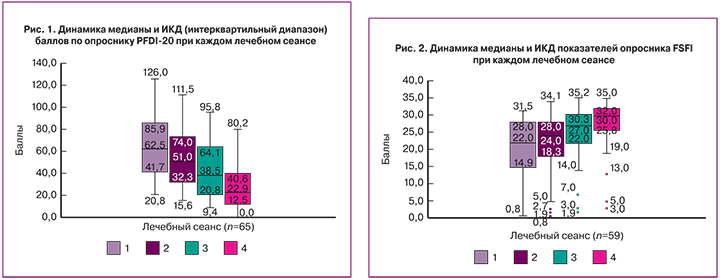
Оценка баллов по опроснику FSFI
В результате лечения по данным опросника FSFI улучшение отмечено у 55 (93%) из 59 пациенток. Как видно на диаграмме, медиана баллов постепенно увеличивалась с каждым лечебным сеансом (рис. 2).
По результатам опросника FSFI выявлено статистически значимое улучшение качества сексуальной функции у пациенток после проведенного лечения по сравнению с данными до начала терапии (Т-критерий Вилкоксона, p<0,05).
Оценка силы мышц тазового дна
Оценка силы мышц тазового дна с помощью системы PMTx с биологической обратной связью производилась в течение 5 секунд всем пациенткам при каждом приеме. Среднее значение величины силы мышц на первом приеме составляло 5,5 Ед, на втором – 6,1 Ед, на третьем – 7 Ед и на четвертом приеме – 7,5 Ед. Стимулирование процессов неоангиогенеза и неоколлагенеза в результате воздействия лазерного излучения обеспечивает улучшение трофики, восстановление тургора и эластичности тканей, что, вероятно, обусловливает улучшение показателей силы тазовых мышц после лечения. По результатам исследования можно сделать вывод о том, что сила мышц у пациенток исследуемой группы увеличилась на 36% после проведения четырех сеансов лазерного воздействия по сравнению с данными до лечения (t-критерий Стьюдента, p<0,05).
Угол Q-tip (тест прямого катетера)
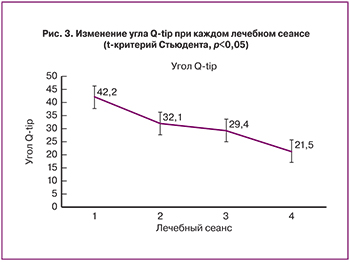
Угол Q-tip уменьшился на 10,1° на втором сеансе, на 12,8° на третьем и на 20,7° на четвертом сеансе по сравнению с данными первого приема. Изменение угла Q-tip говорит о снижении подвижности уретры и шейки мочевого пузыря (рис. 3).
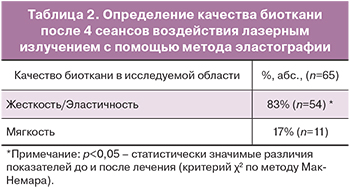
Ультразвуковое исследование и соноэластография
При оценке данных литературы мы отметили, что в других клинических исследованиях уже проводился анализ гистологических препаратов биоптатов стенки влагалища [22–24], поэтому в нашем исследовании мы выбрали менее инвазивный метод и проводили сравнительную оценку качества биологической ткани до и после проведения лазерного воздействия с помощью ультразвукового исследования и соноэластографии. Эластография – метод визуализации мягких тканей, отображающий их механические свойства и показывающий разницу жесткости, эластичности и растяжимости здоровых и патологически измененных тканей. Проводится анализ количества искажений, возникающих во время давления датчиком на стенку влагалища и имеющих цветовую маркировку при получении ультразвукового изображения (плотная ткань – пурпурная, мягкая – красная). Соноэластография проводится с помощью внутриполостного влагалищного датчика с центральной частотой 6,0 мГц.
При проведении контрольного ультразвукового исследования после лечения у 61 (93%) из 65 пациенток наблюдалось увеличение количества визуализируемых сосудов в области влагалищной стенки, что свидетельствует о запуске процесса неоангиогенеза и восстановлении адекватного кровоснабжения данной области. После проведения одного сеанса воздействия лазерным излучением при проведении соноэластографии уже через месяц можно судить о замещении красного цвета пурпурным, что также свидетельствует о запуске процессов неоколлагенеза и восстановлении упругих свойств тканей. У 54 (83%) пациенток из 65 по данным метода эластографии после лечения повышалась степень жесткости стенок влагалища, а значит их упругость (табл. 2).
Изменение степени пролапса тазовых органов
У двоих из 65 пациенток был отмечен переход пролапса тазовых органов II степени в I степень. Для подробного изучения данного лечебного эффекта необходимо большее количество процедур и более длительное время наблюдения.
Обсуждение
За последние несколько лет в литераторе широко освещаются экспериментально-клинические данные об эффективности и безопасности использования неаблативного Er:YAG-лазера (Fotona) в лечении стрессового недержания мочи, пролапса тазовых органов и синдрома релаксированного влагалища [25].
U.B. Ogrinc и соавт. [1] использовали Er:YAG-лазер в лечении цистоцеле II–IV степени у 28 женщин, средний возраст пациенток в данном исследовании составлял 56,1 года. После проведения трех сеансов воздействия лазерного излучения уменьшение пролапса на одну степень было зафиксировано у 27 пациенток, на 2 степени – у 12, на 3 степени – у 2 женщин. Однако по нашим данным уменьшение пролапса тазовых органов на одну степень было зафиксировано у двух пациенток. Вероятно, необходимо проведение большего количества процедур и более длительное время наблюдения за пациентками для детального изучения данного эффекта.
P. Gaviria и соавт. [26] изучили эффективность применения методики IntimaLase для лечения синдрома релаксированного влагалища у 21 пациентки, у 5 из них имелось опущение тазовых органов. После второго сеанса все пациентки, имеющие симптомы генитального пролапса, отмечали улучшение. 20 из 21 пациентки отметили улучшение качества сексуальной жизни. Наше исследование показало похожие результаты: по данным опросника FSFI улучшение качества сексуальной жизни после лечения отмечено у 93% пациенток.
I. Fistonic и соавт. [11] применяли эрбиевый лазер в лечении стрессового недержания мочи у пациенток с наличием или отсутствием опущения органов малого таза. Q-tip тест использовался для оценки подвижности уретры и шейки мочевого пузыря: угол Q-tip уменьшился на 14,7° через 1 месяц, на 15,9° – через 3 месяца и на 22,5° – через 6 месяцев. По данным перинеометрии, результатам опросников ICIQ-UI и PISQ-12 авторами было показано статистически значимое улучшение показателей (p<0,5). Полученные результаты соответствуют нашим данным. В ходе исследования нами отмечено снижение угла Q-tip на 20,7° на четвертом приеме по сравнению с данными первого приема, увеличение силы мышц тазового дна на 36% после завершения лечения (p<0,05). По данным опросников PFDI-20 и FSFI нами также выявлено статистически значимое (p<0,05) улучшение качества жизни пациенток.
А.А. Безменко, А.А. Шмидт и соавт. [13] проводили лечение с помощью Er:YAG-лазера 77 пациенток со стрессовым недержанием мочи. Положительный эффект был достигнут у 41 (70,7%) пациентки с I типом и у 9 (47%) со II типом недержания мочи при напряжении после проведенного лечения. В ходе нашего исследования были получены схожие результаты. По данным подраздела UDI-6 опросника PFDI-20 частота встречаемости такого симптома, как недержание мочи при кашле, смехе, чихании и физической нагрузке в исследуемой группе после проведения 4 сеансов лечения эрбиевым лазером сократилась на 52%.
Е.В. Лешунов, А.Г. Мартов [2] проводили 3 сеанса терапии эрбиевым лазером 6-го поколения Dermablate MCL 31 компании «Asclepion Laser Technologies» (Германия) при лечении стрессового недержания мочи у женщин репродуктивного возраста. До лечения при проведении пробы Вальсальвы уретровезикальный угол составлял в среднем 45,2±4,79°, через 6 месяцев – 36,2±2,42°. Для подсчета индекса сексуальной функции у женщин использовался опросник FSFI, при анализе результатов которого улучшение было достигнуто у 84% пациенток. Наше исследование проводилось на лазерной установке фирмы Fotona, однако полученные данные относительно изменения уретровезикального угла и индекса сексуальной функции у женщин схожи с полученными нами результатами.
Заключение
В заключение можно сказать, что в результате воздействия лазерного излучения уменьшается объем влагалища (по данным ультразвукового исследования и субъективных ощущений пациенток), исчезают дискомфорт во влагалище и диспареуния, симптомы стрессового недержания мочи и дискомфорт в нижних отделах живота снижается более чем на 50% (р=0,0009 и р=0,0002 соответствено), восстанавливаются физиологическая форма и эстетический вид половых органов, повышается либидо. Улучшение качества жизни пациенток после лечения, оцениваемое нами на основании субьективных ощущений, данных опросников, перинеометрии и соноэластографии, выражается в снижении выраженности симптомов генитоуринарных расстройств и улучшении качества сексуальной функции.
На основании проведенного нами клинического исследования можно утверждать, что использование процедур IncontiLase и IntimaLase с технологией Fotona Smooth (SP Spectro, Fotona, Словения) для лечения пациенток с генитоуринарными расстройствами является высокоэффективным и безопасным методом.