Ovarian reserve and surgical hemostasis methods for benign ovarian tumors
Ibragimova U.D., Kozachenko I.F., Adamyan L.V.
The surgical strategy for benign ovarian tumors (BOTs) in women of reproductive age should focus on completely removing the pathological formation while minimizing the impact on healthy ovarian tissue to preserve the ovarian reserve. A key aspect of surgical treatment is the implementation of intraoperative hemostasis using various types of energy and hemostatic matrices.
Objective: To assess the state of ovarian reserve in reproductive-aged patients with BOT using different methods of surgical hemostasis.
Materials and methods: The study included 156 patients of reproductive age diagnosed with ovarian teratoma and/or cystadenoma who presented to the V.I. Kulakov NMRC for OG&P between 2022 and 2024. All the patients underwent surgical treatment with laparoscopic access. Two study groups were formed based on the method of surgical hemostasis: fibrin glue was used in group 1 (n=78), while bipolar coagulation was used in group 2 (n=78). Clinical and laboratory examinations were conducted for all patients, including the determination of anti-Müllerian hormone (AMH), estradiol, inhibin B, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) levels in the blood serum on the 3rd-5th day of the menstrual cycle, as well as tumor marker levels (CA-125, CA 19-9, HE 4, CEA). Ultrasound evaluations of the pelvic organs were performed on the 5th–7th day of the menstrual cycle to assess ovarian volume, antral follicle count (AFC), and intraovarian blood flow before and after surgery.
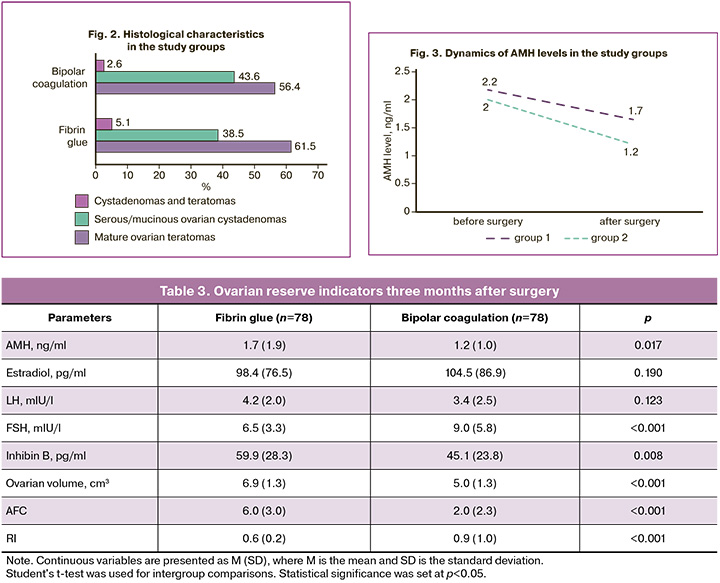
Results: The average age of patients in group 1 was 30.0 (6.7) years, while in group 2 it was 31.0 (7.5) years. Histological examination revealed mature ovarian teratomas in 92/156 (59%) women, serous/mucinous ovarian cystadenomas in 64/156 (41%), and cystadenomas and teratomas in 6/156 (4%). Unilateral formations were observed in 130/156 (83%) patients, while bilateral cysts were present in 26/156 (17%) cases. The sizes of cystic formations ranged from 1.5 to 20.0 cm; the average tumor size in group 1 was 4.0 (3.2) cm, and in group 2 it was 5.0 (4.2) cm. The volume of the ovary with the tumor in group 1 averaged 46.6 (50.4) cm³, with an AFC of 5.0 (5.2) and a resistance index (RI) of 0.9 (0.2). In group 2, the volume of the ovary with the tumor was 45.4 (52.9) cm³, with an AFC of 4.0 (2.6) and an RI of 0.9 (0.1). In group 1, AMH before surgery averaged 2.2 (1.5) ng/ml, while in group 2 it was 2.0 (1.6) ng/ml. After surgery, the volume of the ovary in group 1 averaged 6.9 (1.3) cm³, with an AFC of 6.0 (3.0) and an RI of 0.6 (0.2); in group 2, the ovarian volume was 5.0 (1.3) cm³, with an AFC of 2.0 (2.3) and an RI of 0.9 (1.0). In group 1, AMH after surgical treatment averaged
1.7 (1.9) ng/ml, while in group 2 it was 1.2 (1.0) ng/ml.
Statistically significant differences between the groups were noted in the following parameters: AMH (p=0.017), inhibin B (p=0.008), FSH (p<0.001), ovarian volume (p=0.001), AFC (p<0.001), and RI (p<0.001).
Conclusion: In the surgical treatment of BOT, a critical issue is the maximum preservation of healthy ovarian tissue and reproductive potential of women. Assessing the ovarian reserve before and after surgical treatment allows for the identification of risk factors for its reduction and the selection of the optimal surgical hemostasis method that minimizes trauma to healthy ovarian tissue.
Authors’ contributions: Adamyan L.V., Kozachenko I.F. – conception and design of the study; Kozachenko I.F.,
Ibragimova U.D. – collection and processing of material; Ibragimova U.D., Kozachenko I.F. – statistical analysis, drafting of the manuscript; Adamyan L.V. – editing of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P (Ref. 10.11.2022).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Ibragimova U.D., Kozachenko I.F., Adamyan L.V. Ovarian reserve and
surgical hemostasis methods for benign ovarian tumors.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (8): 150-158 (in Russian)
https://dx.doi.org/10.18565/aig.2025.175
Keywords
Benign ovarian tumors (BOT) are a common issue among women of reproductive age [1, 2]. Research indicates that incidental findings of ovarian formations occur in 6.6% of women aged 25–40 years, with 80–85% of these tumors being benign [1–4]. Over the past decade, the global incidence of BOT has doubled [5]. The most prevalent morphological variants are epithelial and germ cell tumors [5, 6]. BOT and tumor-like lesions of the ovaries manifest in various age groups: in childhood, 65% of cases are functional cysts [4, 7]; in reproductive age, serous cystadenoma and mature teratoma are predominant [4, 6]; and in women over 50 years, both tumor-like and true ovarian formations are present [4]. BOT encompasses pathological formations that arise from disruptions in the cell proliferation and differentiation processes of ovarian tissue [8].
Mature ovarian teratomas, commonly referred to as dermoid cysts, are benign germ cell tumors of the ovary that consist of well-differentiated tissues derived from at least two germ layers [9]. In contrast to malignant immature teratomas, mature teratomas lack primitive embryonic elements and are entirely composed of various types of mature tissues [9]. Macroscopically, a mature teratoma typically appears as a cystic formation (dermoid cyst) containing sebaceous detritus, hair, and other tissues of ectodermal origin. Dense inclusions, such as fragments of bone tissue or teeth, are often found within the cyst cavity [8–10]. Histologically, the tumor displayed a disorganized mixture of mature tissues, originating from all three germ layers. Characteristic findings include areas of skin with appendages (hair, sebaceous glands), adipose and muscle tissue, cartilage, and bone, as well as epithelial structures resembling intestinal or respiratory epithelium. This polymorphism reflects the original germ cell's ability to differentiate into various cell lines [8–10]. Mature ovarian cystic teratomas comprise 15 to 20% of all ovarian tumors [11, 12].
Benign serous ovarian tumors account for 16% of all epithelial neoplasms of the ovaries and cover two-thirds of benign epithelial ovarian tumors [13]. They occur in women whose average age ranges from 40 to 60 years old. They are bilateral in 10–20% of the cases. They have a smooth outer surface and contain one or more thin-walled cysts filled with clear fluid. Serous cystadenomas are usually single-chambered, but can also be multichambered. Approximately 80% of mucinous ovarian tumors are benign [13]. Ovarian cystadenoma is a common benign epithelial neoplasm with favorable prognosis. The two most common types are serous and mucinous cystadenomas, whereas endometrioid and clear cell cystadenomas are rare. Mucinous cystadenomas have a smooth surface and are usually multi-chambered, but single-chambered cystadenomas are also found [13].
The standard treatment for patients of reproductive age is cystectomy, with maximum preservation of healthy ovarian tissue [1]. However, surgical treatment can have a detrimental effect on the ovarian reserve, which can occur due to thermal damage to the follicles during surgical hemostasis [1]. Therefore, in gynecological surgery, the development, optimization, and implementation of new methods of surgical hemostasis are constantly underway, while maintaining a balance between effective hemostasis and minimal damage to the ovarian tissue [1].
The ovarian reserve is the functional reserve of the ovary, which determines the ability of the latter to develop a healthy follicle with a full-fledged egg and an adequate response to ovarian stimulation [14]. Various tests and markers are used to assess ovarian reserve, such as serum levels of estradiol, follicle-stimulating hormone (FSH), anti-Müllerian hormone (AMH), inhibin-B, and the number of antral follicles (AFC), of which AMH is the main marker [2, 12, 15]. This hormone is a glycoprotein produced by granulosa cells of ovarian follicles [2].
The main methods of stopping bleeding after removal of ovarian cysts are electrosurgical bipolar coagulation, suturing of the ovary, and the use of fibrin glue [16]. In laparoscopy, the most commonly used method of hemostasis is bipolar coagulation [17]. In gynecological surgery, bipolar forceps with 3 mm wide electrodes are preferred. When precise and limited coagulation is required or when it is necessary to reduce the degree of thermal effect, bipolar branches of 1.5 mm should be used [17]. New rotary bipolar instruments (bipolar grasping forceps and RoBi scissors) meet the basic requirements of surgery, including dissection, grasping, and hemostasis [17].
The modern method used for this purpose is fibrin glue [1]. Glue is applied locally to bleeding surfaces or wound edges. The tissues are grasped (glued) within a few minutes [1, 18]. Fibrin glue is a two-component biological glue containing high concentrations of blood clotting factors (fibrinogen, thrombin, calcium ions, factor VIII, etc.) [1, 18]. When the components are mixed, it reproduces the final stage of the coagulation cascade: a fibrin clot is formed, gluing the tissues. The resulting fibrin clot firmly adheres to the tissues, closes defects, and stops bleeding (hemostatic effect), and also serves as a framework for cells and growth factors that promote wound healing. Fibrin glue is biocompatible and gradually dissolves enzymatically, leaving no foreign material in the tissue [1, 18]. In surgery, fibrin glue is used to improve hemostasis, seal tissues, and accelerate wound healing [1, 18]. Fibrin glue is indicated as a hemostatic agent when it is necessary to stop bleeding and close a defect in ovarian tissue while preserving ovarian function as much as possible [16].
The advantage of using fibrin glue lies in its application, which does not result in tissue trauma or ischemia while simultaneously achieving adhesive, hemostatic, and sealing effects that positively influence wound healing [19, 20]. In contrast, standard hemostasis methods can lead to irreversible neurogenic and microcirculatory disorders in the ovarian tissue, damage to the follicular apparatus, and ultimately ovarian failure [21, 22]. In gynecology, the use of glue in organ-preserving surgery is a potential means of enhancing fertility preservation. By maintaining the ovarian reserve and reducing the formation of adhesions, the likelihood of a successful pregnancy in the future is increased [21].
This study aimed to evaluate the state of ovarian reserve in reproductive-aged patients with BOT, employing various methods of surgical hemostasis and subsequently analyzing their effects on the preservation of the follicular apparatus.
Materials and methods
An analysis of treatment results was conducted for 156 reproductive-age patients (18–45 years old) hospitalized in the gynecological department of the V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, all diagnosed with "ovarian cystic formation (cystadenoma and/or teratoma)" during the period from 2022 to 2024. Patients provided informed consent to participate in the study, which was reviewed and approved by the Research Ethics Committee of V.I. Kulakov NMRC for OG&P (Ref. 10.11.2022).
All patients underwent a standard examination according to an accepted algorithm, which included clinical and laboratory assessments; oncological marker level studies (CA-125, CA 19-9, HE 4, CEA); measurements of serum AMH, estradiol, inhibin B, luteinizing hormone (LH), FSH; and pelvic ultrasound (US) to measure ovarian volume, antral follicle count (AFC), and intra-ovarian blood flow with determination of the resistance index (RI).
The patients were divided into two groups based on the selected surgical hemostasis method: group 1 used fibrin glue (n=78), and group 2 used bipolar coagulation (n=78).
All the patients underwent organ-sparing laparoscopic surgery using a standard technique. After creating the pneumoperitoneum, a Karl Storz laparoscope and trocar for the second puncture were sequentially introduced into the abdominal cavity. Typically, 3–4 trocars were used (an optical trocar in the periumbilical area and additional trocars in the left/right iliac and suprapubic areas), depending on the cyst size and anatomy. The main stages of the procedure included tumor enucleation, hemostasis, ovarian edge approximation, and extraction of the operational material.
On the ovarian surface above the cyst, the thinnest and least vascularized area of the tunica albuginea was grasped with an atraumatic clamp and a longitudinal incision was made to initiate cyst enucleation. After incision, the plane between the cyst wall and the surrounding ovarian tissue was carefully identified. The ovarian cyst was shelled out using atraumatic clamps. The macro preparations were removed in an endoscopic container through a trocar opening. Hemostasis was achieved using one of the selected methods: bipolar coagulation (n=78) or fibrin glue (n=78).
During the procedure, the operative field was periodically irrigated to cool the tissue and identify bleeding vessels. Bipolar coagulation was applied point-wise at the bleeding sites, with fragments of ovarian stroma captured or pressed with bipolar forceps tips until bleeding stopped.
The technique for introducing fibrin glue was as follows: after cyst enucleation, the ovary was removed and fixed in a "bowl" shape, oriented with the bed facing upwards. A thin layer of fibrin glue was evenly applied to cover the entire bleeding surface using a catheter applicator. Glue polymerization occurred within 1-2 minutes, achieving complete hemostasis with no additional hemostatic measures required.
Intraoperatively, macropreparations were sent for histological examination at the 1st Pathological Department of the V.I. Kulakov NMRC for OG&P, utilizing standard techniques with 4–5-micron cryosection preparation and subsequent hematoxylin and eosin staining.
The evaluation criteria for the surgical hemostasis methods included dynamics in ovarian reserve parameters before and three months after surgical treatment as well as reproductive outcomes.
Statistical analysis
Statistical analysis was performed using Microsoft Office Excel 2015 and MedCalc v.12. The normality of distribution in the samples was assessed using the Kolmogorov–Smirnov test. For normally distributed continuous data, results were described using arithmetic mean (M) and standard deviation (SD); comparisons between groups were performed using Student's parametric t-test. Categorical variables were described using counts and percentages. Pearson’s chi-square (χ2) test was used for group comparisons. Differences were considered statistically significant at p<0.05.
Results
The mean age of patients in the 1st group was 30.0 (6.7) years, and in the 2nd group – 31.0 (7.5) years. In both groups, the majority of patients were aged 30–34 years (Table 1). The main complaints were lower abdominal pain, painful menstruation, and the absence of pregnancy. The average age at menarche was 13.0 (0.8) years. The duration of the menstrual cycle was 28.0 (2.5) days, and the duration of menstruation was 5.0 (0.8) days. Heavy menstruation was observed in 61/156 (39%) women, moderate in 95/156 (61%), and scanty was not detected. Painful menstruation was noted in 31/156 (20%) patients. Regarding the medical history, 46/156 (29%) women had timely deliveries, 16/156 (10%) had missed miscarriages, and 6/156 (4%) had ectopic pregnancies.
In 83/156 (53%) women, a combined pathology of the pelvic organs was detected, including adhesions, uterine fibroids, endometrial polyps, and developmental anomalies of the reproductive organs.
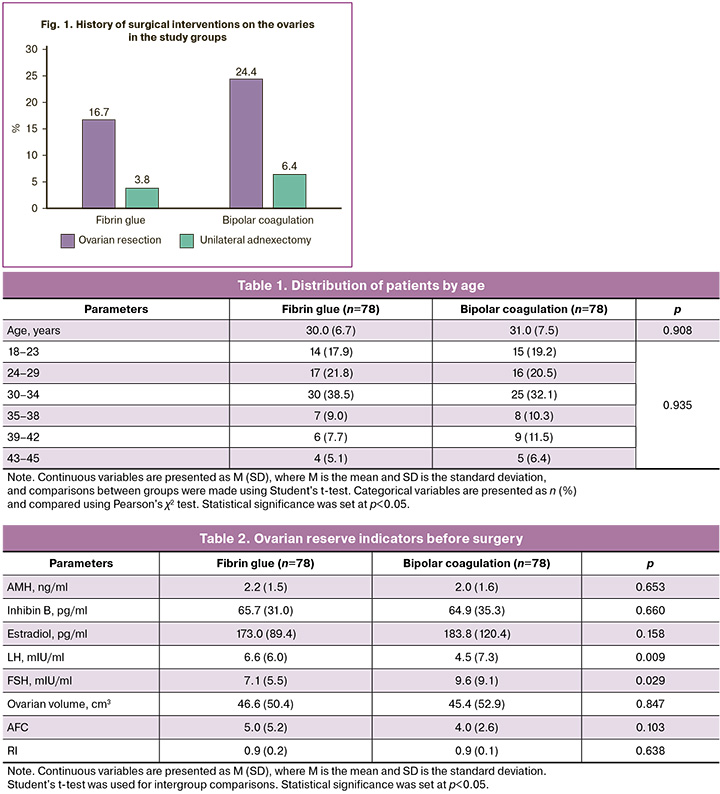
A total of 32/156 (21%) women had previously undergone surgical treatment for ovarian cystic formation, and 8/156 (5%) had undergone unilateral adnexectomy (Fig. 1).
Pelvic US revealed cystic formations (teratomas and/or cystadenomas) of various sizes. The ovarian volume in the 1st group averaged 46.6 (50.4) cm³, AFC – 5.0 (5.2), RI – 0.9 (0.2). In the 2nd group, the ovarian volume was 45.4 (52.9) cm³, AFC – 4.0 (2.6), RI – 0.9 (0.1) (Table 2).
Before surgical treatment, the AMH level in the 1st group was on average 2.2 (1.5) ng/mL, LH – 6.6 (6.0) mIU/mL, FSH – 7.1 (5.5) mIU/mL, estradiol – 173.0 (89.4) pg/mL, inhibin B – 65.7 (31.0) pg/mL, CA-125 – 13.6 (5.4) U/mL, CA 19-9 – 12.1 (16.5) U/mL, N4 – 43.7 (9.2) pmol/L, REA – 0.8 (1.2) ng/mL (Table 2).
In the 2nd group, the AMH level before surgery was on average 2.0 (1.6) ng/mL, LH – 4.5 (7.3) mIU/mL, FSH – 9.6 (9.1) mIU/mL, estradiol – 183.8 (120.4) pg/mL, inhibin B – 64.9 (35.3) pg/mL, CA-125 – 11.2 (10.3) U/mL, CA 19-9 – 10.3 (21.9) U/mL, N4 – 44.5 (16.5) pmol/L, REA – 1.1 (0.8) ng/mL (Table 2).
In 92/156 (59%) women, histological examination revealed mature ovarian teratomas; in 64/156 (41%), serous/mucinous ovarian cystadenomas; and in 6/156 (4%), cystadenomas and teratomas (Fig. 2). In 130/156 (83%) patients, the formations were unilateral, and bilateral cysts were found in 26/156 (17%) cases. The sizes of the cystic formations ranged from 1.5 to 20.0 cm. The average tumor size in the 1st group was 4.0 (3.2) cm, and in the 2nd group – 5.0 (4.1) cm.
The operation time in the 1st group averaged 55 (17.1) minutes, and in the 2nd group – 55 (14.2) minutes, depending on the tumor size, extent of damage, and presence of adhesions. Blood loss in the 1st group averaged 20.0 (23.1) mL in the 2nd group – 30.0 (21.5) mL in the second group. No postoperative complications occurred.
After surgery, patients were monitored and examined at their place of residence, and of 2/156 (1%) women experienced recurrences three months post-operation. At the time of the study, 94/156 (60%) patients had planned pregnancy, including 50/78 (64%) in the 1st group and 44/78 (56%) in the 2nd group. Pregnancy occurred in 32/78 (41%) patients in the 1st group and in 29/78 (37%) in the 2nd group, with assisted reproductive technologies used in 9/32 (28%) in the 1st group and 12/29 (41%) in the 2nd group. The time to pregnancy ranged from three to seven months after surgery. There were no cases of pregnancy termination or miscarriages.
Laboratory and ultrasound data were analyzed three months after surgery.
The ovarian volume in the 1st group was on average 6.9 (1.3) cm³, AFC – 6.0 (3.0), RI – 0.6 (0.2). In the 2nd group, ovarian volume was 5.0 (1.3) cm³, AFC – 2.0 (2.3), RI – 0.9 (1.0) (Table 3).
After surgery, the AMH level in the 1st group was on average 1.7 (1.9) ng/mL, LH – 4.2 (2.0) mIU/mL, FSH – 6.5 (3.3) mIU/mL, estradiol – 98.4 (76.5) pg/mL, inhibin B – 59.9 (28.3) pg/mL, CA-125 – 8.5 (9.3) U/mL, CA 19-9 – 8.4 (3.8) U/mL, N4 – 33.0 (8.5) pmol/L, REA – 1.2 (0.5) ng/mL (Table 3).
In the 2nd group, the AMH level was 1.2 (1.0) ng/mL, LH – 3.4 (2.5) mIU/mL, FSH – 9.0 (5.8) mIU/mL, estradiol – 104.5 (86.9) pg/mL, inhibin B – 45.1 (23.8) pg/mL, CA-125 – 12.3 (8.6) U/mL, CA 19-9 – 8.5 (8.8) U/mL, N4 – 31.6 (10.6) pmol/L, REA – 1.2 (1.1) ng/mL (Table 3).
Statistically significant differences between the groups were found for the following indicators: AMH (Fig. 3), FSH, inhibin B, ovarian volume, AFC, and RI, indicating a more pronounced reduction in ovarian reserve with traditional hemostasis methods. In the group in which surgical hemostasis with fibrin glue was used, AFC, AMH, and inhibin B levels before and after surgery did not change significantly (p>0.05).
Discussion
The social and medical significance of BOTs arises not only from the increasing incidence of the condition but also from the demographic shift in the disease: 48.8% of women diagnosed with ovarian neoplasms are of an early reproductive age [5].
Patient management should be tailored to individual characteristics, including cyst size, access to the ovaries, ovarian reserve, age, previous adnexal surgeries, and symptoms [23]. The primary treatment for BOT is surgery, predominantly laparoscopy [4, 10, 24]. In the surgical management of BOT, key considerations include the timeliness and accuracy of diagnosis, preservation of reproductive potential, especially ovarian reserve, use of sparing techniques for hemostasis, adherence to ablastics principles, and prevention of recurrence [4, 10, 24]. Prior to undergoing surgical interventions on the ovaries, patients should be informed about the risk of decreased ovarian reserve and the option for cryopreservation of oocytes to facilitate delayed motherhood [17]. Organ-preserving surgical procedures on the ovaries of young women should be conducted by highly skilled surgeons, and it is advisable to employ sparing hemostatic methods that minimize thermal damage to the ovarian tissue [1].
All surgical energy modalities – mechanical, electrical, thermal, welding, laser, or ultrasonic scalpel, as well as chemical adhesives—can negatively affect ovarian tissue and diminish ovarian reserve in reproductive-age women, depending on various pathophysiological mechanisms [25]. Bipolar electrocoagulation is the conventional method for achieving surgical hemostasis during laparoscopic cystectomy. However, it can cause local thermal damage, potentially reducing ovarian reserve. Given that preserving healthy and functional ovarian tissue is paramount during cystectomy, it is crucial to evaluate which hemostatic technique is the least aggressive regarding ovarian reserve [23]. Traditional methods typically involve electrocoagulation of the bleeding areas or suturing for hemostasis after ovarian cystectomy. Electrocoagulation induces coagulation necrosis in the tissues, leading to localized inflammation during healing process [18]. Fibrin glue, which closely resembles natural blood clots, elicits minimal tissue reactions, thus promoting faster healing and reducing scar tissue formation [18]. This glue can seal wound defects without thermal or mechanical effects [16].
Currently, there is no standardized approach for managing bleeding during ovarian surgery that maximally preserves the primordial pool and minimizes the loss of a woman's reproductive potential [22]. The use of hemostatic matrices for intraoperative hemostasis during surgical treatment has been shown to have a lesser negative impact on key indicators of ovarian reserve than bipolar coagulation [26]. In contrast to diathermy, which can cause diffuse damage to the surrounding tissue, fibrin glue acts locally, affecting only the area to which it is applied [21]. Therefore, the use of fibrin glue for ovarian cysts is justified, as it provides reliable hemostasis with minimal tissue trauma, which is particularly important for reproductive-age patients [21].
Conclusion
Preserving ovarian reserves is crucial for patients of reproductive age who wish to realize their reproductive potential in the future. While laparoscopic removal of benign cysts is considered an organ-preserving procedure, the presence of a cyst and its surgical removal can unintentionally decrease the ovarian reserve. However, the selection of an optimal hemostatic method can help minimize this risk. Careful and gentle execution of the operation, with atraumatic isolation of the cyst capsule and minimal loss of healthy tissue, combined with sparing hemostatic techniques, supports the preservation of reproductive potential. The use of modern hemostatic materials, particularly two-component fibrin glue, facilitates reliable control of bleeding without causing additional damage to ovarian tissue.
The findings of this study indicate that favoring fibrin hemostasis over electrocoagulation results in a significantly smaller decrease in ovarian reserve indicators. Thus, fibrin glue has emerged as a promising hemostatic agent in ovarian surgery, offering a greater sparing effect on reproductive function.
References
- Su Y.Y., Lin Y.S., Yang L.Y., Pan Y.B., Huang Y.T., Weng C.H. et al. Use of human fibrin glue (Tisseel) versus suture during transvaginal natural orifice ovarian cystectomy of benign and non-endometriotic ovarian tumor: a retrospective comparative study. BMC Surg. 2021; 21(1): 49. https://dx.doi.org/10.1186/s12893-021-01061-1
- Baracat C.M.F., Abdalla-Ribeiro H.S.A., Araujo R.S.D.C., Bernando W.M., Ribeiro P.A. The impact on ovarian reserve of different hemostasis methods in laparoscopic cystectomy: a systematic review and meta-analysis. Rev. Bras. Ginecol. Obstet. 2019; 41(6): 400-8. https://dx.doi.org/10.1055/s-0039-1692697
- Rocha R.M., Barcelos I.D.E.S. Practical recommendations for the management of benign adnexal masses. Rev. Bras. Ginecol. Obstet. 2020; 42(9): 569-76. https://dx.doi.org/10.1055/s-0040-1714049
- Матейкович Е.А., Шевлюкова Т.П., Чернова А.Л. Доброкачественные опухоли и опухолеподобные поражения яичников: структура, методы диагностики, тактика оказания медицинской помощи. Медицинская наука и образование Урала. 2021; 22(1(105)): 100-4. [Mateykovich E.A., Shevlyukova T.P., Chernova A.L. Benign tumors and tumor-like lesions of the ovaries: structure, diagnostic methods, tactics of medical care. Medical Science and Education of Ural. 2021; 22(1(105)): 100-4 (in Russian)]. https://dx.doi.org/10.36361/1814-8999-2021-22-1-100-104
- Соломатина А.А., Михалёва Л.М., Тюменцева М.Ю., Братчикова О.В., Хамзин И.З., Тумасян Е.А., Гашимова А.И., Исмайилова П.Д. Морфофункциональное состояние эндометрия у пациенток до и после органосохраняющих операций по поводу доброкачественных опухолей яичников. Вопросы гинекологии, акушерства и перинатологии. 2022; 21(3): 45-52. [Solomatina A.A., Mikhaleva L.M.,
- Tyumentseva M.Yu., Bratchikova O.V., Khamzin I.Z., Tumasyan E.A., Gashimova A.I., Ismayilova P.D. Morphological and functional features of the endometrium in patients before and after ovary-sparing surgery for benign ovarian tumors. Gynecology, Obstetrics and Perinatology. 2022; 21(3): 45-52 (in Russian)]. https://dx.doi.org/10.20953/1726-1678-2022-3-45-52
- Волченок Д. А., Тихоновская О. А., Петров И. А., Логвинов С. В., Мунгалова А. Д. Состояние овариального резерва у пациенток с функциональными кистами яичников. Journal of Siberian Medical Sciences. 2019; (1): 18-27. [Volchenok D.A., Tikhonovskaya O.A., Petrov I.A., Logvinov S.V., Mungalova A.D. The state of ovarian reserve in patients with functional ovarian cysts. Journal of Siberian Medical Sciences. 2019; (1): 18-27 (in Russian)]. https://dx.doi.org/10.31549/2542-1174-2019-1-18-27
- Matalliotakis M., Matalliotaki C., Zervou M. I., Krithinakis K., Goulielmos G. N., Kalogiannidis I. et al. Retrospective evaluation of pathological results among women with ovarian endometriomas versus teratomas. Mol. Clin. Oncol. 2019; 10(6): 592-6. https://dx.doi.org/10.3892/mco.2019.1844
- Мелкозерова О.А., Клепиков Ю.В., Окулова Е.О. Герминогенные опухоли яичников у детей и подростков: молекулярно-биологические аспекты и проблемы хирургической тактики с позиции сохранения фертильности. Лечение и профилактика. 2021; 11(2): 62-70. [Melkozerova O.A., Klepikov Yu.V., Okulova E.O. Herminogenous ovarian tumors in children and adolescents: molecular-biological aspects and problems of surgical tactics from the position of preserving fertility. Treatment and Prevention. 2021; 11(2): 62-70 (in Russian)].
- Heskett M.B., Sanborn J.Z., Boniface C., Goode B., Chapman J., Garg K. et al. Multiregion exome sequencing of ovarian immature teratomas reveals 2N near-diploid genomes, paucity of somatic mutations, and extensive allelic imbalances shared across mature, immature, and disseminated components. Mod. Pathol. 2020; 33(6): 1193-206. https://dx.doi.org/10.1038/s41379-019-0446-y
- Шевякова Е.В., Байрамкулова Л.М., Шахназарян Н.Г. Анализ лечения зрелых тератом яичника. В кн.: Актуальные проблемы науки и техники: сборник научных статей по материалам II Международной научно-практической конференции, Уфа, 22 мая 2020 г. Уфа: Вестник науки; 2020: 362-7. [Shevyakova E.V., Bayramkulova L.M., Shahnazaryan N.G. Analysis of treatment of mature ovarian teratomas. In: Current problems of science and technology: collection of scientific articles based on the materials of the II International scientific and practical conference, Ufa, May 22, 2020. Ufa: Bulletin of Science; 2020: 362-7 (in Russian)].
- Abramova S., Simfukwe K., Gladkova O., Grachev D., Iseev D. Modern aspects of etiology, mechanisms, pathogenesis and diagnostics of ovarian formations. Bulletin of Science and Practice. 2019; 5(5): 38-45. [Абрамова С.В., Симфукве К., Гладкова О.Н., Грачев Д.С., Исеев Д.Б. Современные аспекты этиологии, механизмов, патогенеза и диагностики образований яичников. Бюллетень науки и практики. 2019; 5(5): 38-45. (in English)]. https://dx.doi.org/10.33619/2414-2948/42/05
- Аradağ C., Demircan S., Turgut A., Çalışkan E. Effects of laparoscopic cystectomy on ovarian reserve in patients with endometrioma and dermoid cyst. Turk. J. Obstet. Gynecol. 2020; 17(1): 15-20. https://dx.doi.org/10.4274/tjod.galenos.2020.37605
- Limaiem F., Lekkala M.R., Mlika M. Ovarian cystadenoma. [Updated 2022 Oct 24]. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2022 Jan.
- Филиппова Е.С., Козаченко И.Ф., Адамян Л.В., Дементьева В.О. Влияние хирургического лечения эндометриоидных кист яичников на состояние овариального резерва у женщин репродуктивного возраста. Проблемы репродукции. 2018; 24(4): 71-80. [Filippova E.S., Kozachenko I.F., Adamyan L.V., Dementyeva V.O. Influence of surgical treatment of ovarian endometrioid cysts on ovarian reserve in women of reproductive age. Russian Journal of Human Reproduction. 2018; 24(4): 71-80 (in Russian)]. https://dx.doi.org/10.17116/repro20182404171
- Салимова Д.К., Данусевич И.Н., Наделяева Я.Г., Лазарева Л.М., Аталян А.В., Новикова Е.А., Шолохов Л.Ф., Рашидова М.А., Сутурина Л.В. Клинико-лабораторные показатели сниженного овариального резерва у женщин репродуктивного возраста: кросс-секционное исследование. Экология человека. 2022; 29(8): 587-97. [Salimova M.D., Danusevich I.N., Nadelyaeva Y.G., Lazareva L.M., Atalyan A.V., Novikova E.A., Sholokhov L.F., Rashidova M.A., Suturina L.V. Clinical manifestations of decreased ovarian reserve in premenopausal women: a cross-sectional study. Human Ecology. 2022; 29(8): 587-97 (in Russian)]. https://dx.doi.org/10.17816/humeco106718
- Lim H., Park S.J., Paik H., Mun J., Lee E.J., Lee S. et al. Preservation of the ovarian reserve and hemostasis during laparoscopic ovarian cystectomy by a hemostatic agent versus suturing for patients with ovarian endometriosis: study protocol for randomized controlled, non-inferiority trial (PRAHA-2 trial). Trials. 2021; 22(1): 473. https://dx.doi.org/10.1186/s13063-021-05431-1
- Нажмутдинова Д.К., Абдуллаева Л.М., Клычев С.И., Сапаров А.Б., Ашурова У.А. Влияние на овариальный резерв лапароскопической цистэктомии. Журнал теоретической и клинической медицины. 2020; 3: 159-62. [Nazhmutdinova D.K., Abdullaeva L.M., Klychev S.I., Saparov A.B., Ashurova U.A. Effect of ovarian cystectomy on ovarian reserve. Journal of Theoretical and Clinical Medicine. 2020; (3): 159-62 (in Russian)].
- Goczyńska P., Lasocka J., Lachert E. Fibrin glues – the current state of knowledge. Journal of Transfusion Medicine. 2021; 14(4): 214-24. https://dx.doi.org/10.5603/JTM.2021.0012
- Kostrzewa M., Wilczyński J.R., Głowacka E., Żyła M., Szyłło K., Stachowiak G. One-year follow-up of ovarian reserve by three methods in women after laparoscopic cystectomy for endometrioma and benign ovarian cysts. Int. J. Gynaecol. Obstet. 2019; 146(3): 350-6. https://dx.doi.org/10.1002/ijgo.12884
- Адамян Л.В., Мынбаев О.А. Оценка эффективности применения фибринового клея при гинекологических реконструктивно-пластических операциях. В кн.: Кулаков В.И., Адамян Л.В., ред. Эндоскопия в диагностике и лечении патологии матки: Mеждународный конгресс с курсом эндоскопии, Москва, 9-13 июня 1997. М.: Гарант; 1997. Т. 1: 48-56. [Adamyan L.V., Mynbaev O.A. Evaluation of the effectiveness of the use of fibrin glue in gynecological reconstructive and plastic surgeries. In: Kulakov V.I., Adamyan L.V., eds. Endoscopy in the diagnosis and treatment of uterine pathology: International congress with a course of endoscopy, Moscow, June 9-13, 1997. Moscow: Garant; 1997. Vol. 1: 48-56 (in Russian)].
- Chung J.P.W., Law T.S.M., Mak J.S.M., Sahota D.S., Li T.C. Ovarian reserve and recurrence 1 year post-operatively after using haemostatic sealant and bipolar diathermy for haemostasis during laparoscopic ovarian cystectomy. Reprod. Biomed. Online. 2021; 43(2): 310-8. https://dx.doi.org/10.1016/j.rbmo.2021.05.003
- Соломатина А.А., Хамзин И.З., Тюменцева М.Ю., Чабиева Л.Б., Тумасян Е.А., Дулаева А.О. Органосберегающие операции у пациенток с доброкачественными образованиями яичников в аспекте сохранения репродуктивного потенциала. Лечебное дело. 2019; 3: 34-41. [Solomatina A.A., Khamzin I.Z., Tyumentseva M.Yu., Chabieva L.B., Tumasyan E.A., Dulaeva A.O. Organ-preserving surgery in patients with benign ovarian masses in terms of maintaining reproductive potential. Lechebnoe Delo. 2019; 3: 34-41 (in Russian)]. https://dx.doi.org/10.24411/2071-5315-2019-12138
- Пивазян Л.Г., Унанян А.Л., Пойманова О.Ф., Бондаренко Е.Н., Ищенко А.И. Эндометриома: овариальный резерв и тактика ведения. Проблемы репродукции. 2021; 27(5): 77-83. [Pivazyan L.G., Unanyan A.L., Poymanova O.F., Bondarenko E.N., Ishchenko A.I. Endometrioma: ovarian reserve and management. Russian Journal of Human Reproduction. 2021; 27(5): 77-83 (in Russian)]. https://dx.doi.org/10.17116/repro20212705177
- Nowak-Psiorz I., Ciećwież S., Brodowska A., Starczewski A. Treatment of ovarian endometrial cysts in the context of recurrence and fertility. Adv. Clin. Exp. Med. 2019; 28(3): 407-13. https://dx.doi.org/10.17219/acem/90767
- Венцковский Б.М., Жегулович В.Г., Жегулович Ю.В. Овариальный резерв при хирургии яичника. Гемостаз путем временной компрессии как альтернатива воздействия физических энергий и химических средств на яичник. Репродуктивное здоровье. Восточная Европа. 2019; 9(2): 120-6. [Ventskovsky B.M., Zhegulovich V.G., Zhegulovich Yu.V. Ovarian reserve in ovarian surgery. Hemostasis by temporary compression as an alternative to the effects of physical energies and chemicals on the ovary. Reproductive Health. Eastern Europe. 2019; 9(2): 120-6 (in Russian)].
- Кузьмина Н.С., Беженарь В.Ф., Калугина А.С. Опыт интраоперационного использования гемостатических матриц для сохранения овариального резерва у больных с эндометриомами. Проблемы репродукции. 2018; 24(2): 54-62. [Kuzmina N.S., Bezhenar’ V.F., Kalugina A.S. Experience in intraoperative use of hemostatic matrices to preserve the ovarian reserve in patients with endometriomas. Russian Journal of Human Reproduction. 2018; 24(2): 54-62 (in Russian)]. https://dx.doi.org/10.17116/repro201824254-62
Received 27.06.2025
Accepted 29.07.2025
About the Authors
Ummusalimat D. Ibragimova, PhD student, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, amintaeva_umm@mail.ru, https://orcid.org/0009-0008-6984-7193
Irena F. Kozachenko, Dr. Med. Sci., Leading Researcher, obstetrician-gynecologist, Gynecological Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, irenakozachenko@rambler.ru,
https://orcid.org/0000-0003-1822-9164
Leila V. Adamyan, Academician of the Russian Academy of Sciences, Dr. Med. Sci., Professor, Deputy Director for Research, Head of the Department of Operative Gynecology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia,
117997, Russia, Moscow, Ac. Oparin str., 4; Chief Specialist in Gynecology of the Ministry of Health of Russia; Head of the Department of Reproductive Medicine and
Surgery of the Faculty of Postgraduate Education, Russian University of Medicine, 127473, Russia, Moscow, Delegatskaya str., 20-1, adamyanleila@gmail.com,
https://orcid.org/0000-0002-3253-4512
Corresponding author: Ummusalimat D. Ibragimova, amintaeva_umm@mail.ru