Features of the expression of the immunohistochemical markers P16 and KI67 in women with chronic cervicitis associated with bacterial and viral infections
Bokach O.M., Niauri D.A., Tishkov A.V., Selkov S.A.
Objective. To investigate the features of the expression of P16 and Ki67 in women with an abnormal colposcopic pattern and chronic cervicitis associated with bacterial and viral infections. Material and methods. The materials were genitourinary discharge and cervical biopsy samples from women diagnosed with chronic cervicitis. The investigators made microscopic examination of Gram stained smears from the urethra, vagina, and cervical canal, as well as culture and RT-PCR assay of cervicovaginal secretions, cervical cancer cytology, and p16 and Кі-67 histological and immunohistochemical studies of cervical tissues. Results. In women with chronic cervicitis, the association of high oncogenic risk human papillomavirus (HPV) with Chlamydia trachomatis and Mycoplasma genitalium was found to increase the frequency of Ki-67 expression in two thirds of the cervical epithelium by 4 times as compared to that of high oncogenic risk HPV with Mycoplasma hominis and/or Ureaplasma urealyticum. Conclusion. When the abnormal colposcopic pattern is detected in women with chronic cervicitis, a histological study of cervical tissues should be complemented with Ki-67 expression examination for the differential diagnosis of the severity of cervical neoplasia.
Keywords
Inflammatory cervical disorders make up 60-70% of all cases of infectious and inflammatory diseases of the female reproductive system [1]. They impair the protective properties of the cervical canal and may foster the development of inflammatory pelvic disorders, miscarriage, increase the risk of intrauterine fetal infection, postpartum and post-abortion suppurative and septic complications, cervical neoplastic processes. The findings showed that the inflammation in the multilayered flat and cylindrical cervical epithelium, caused by bacterial and viral infections, lead to dysplasia and cervical cancer.
The high-risk human papilloma virus (HPV) has been proven to play a key role in the development of dysplasia and cervical cancer [2, 3]. Herewith, the cervititis associated with bacterial flora stimulates HPV infection.
According to the World Health Organisation, 15 000 new cases of cervical cancer are registered annually in Russia [4]. In the Russian Federation, the incidence rate of cervical cancer in 2015 was 15.2, the mortality rate was 5.2. Cervical cancer continues being the third in the structure of cancer pathology in women [5]. Despite the existing screening, the average annual increase in cervical cancer mortality has amounted to 7.22% over the past 10 years in Russia [5]. Therefore, it is relevant to substantiate the examination methods that will allow expanding the risk group for the development of the cervical neoplastic processes, with a view to their further monitoring.
The study focused on the specific aspects of expression of immunohistochemical p16 and Ki-67 markers in the cervical epithelium in women with chronic cervicitis associated with bacterial and viral infection.
Materials and Methods
Urethral and vaginal discharge, biopsy slices of the cervical tissue were taken from 73 women aged 22 to 48 with a verified diagnosis of “chronic cervicitis”, in which bacterial, viral, bacterial and viral infection was found during the microbiological study of cervicovaginal discharge.
Women aged 22-48, with abnormal colposcopic pattern, chronic cervicitis diagnosed on the basis of clinical and laboratory testing were eligible for inclusion.
Patients were excluded if they were under 18 and over 48; if they were currently pregnant; if they had acute genital inflammation, hemorrhage of unknown etiology, oncology, severe somatic pathology, pre-existing cervical destruction.
All women underwent clinical and laboratory examination based on the Order No. 572n datedNovember 01, 2012 of the Ministry of Health and Social Development: microscopic examination of the urethral, vaginal and cervical smears with Gram staining, study of cervicovaginal discharge by microbiological method and polymerase chain reaction (PCR).
For real-time PCR (PCR–RT) (with the number of copies specified) in order to identify the Chlamydia trachomatis (Сhl. trachomatis), Mycoplasma genitalium (M. genitalium), and Mycoplasma hominis (M. hominis), Ureaplasma urealyticum (U. urealyticum), Trichomonas vaginalis (T. vaginalis), herpes simplex virus (Herpes simplex (HSV)) type I and II, Сytomegalovirus (CMV), Virus Epshtein-Barra DNA, the HPV material was collected from the cervical canal using the universal gynecological probe ZGU “TsM” (manufactured by OOO “CentrMed”, Russia) and placed in special sterile tubes with transport eppendorf medium. Infectious agents (excluding HPV) were identified through PCR-RT using the Cobas 4800 diagnostic system (manufactured by Roche Diagnostics, Switzerland). High-risk (HPV High) (type 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) and low-risk (HPV Low – type 6, 11) HPVs were identified and typed through PCR-RT using hybridization fluorescence detection and the “AmpliSens HCR HPV FL genotype” diagnostic systems (manufactured by InterLabServis, Russia).
For the culture-based study, the material was sampled from the cervical canal and vagina using special microbiological Transystem swabs (manufactured by Copanitalia, Italy). Then, the swab was placed in the same-name container for bacteriological test and sent to the laboratory where the culture media were inoculated to produce the isolated colonies: Escherichia coli (E. coli), Enterococcus spp., Staphylococcus epidermidis, Staphylococcus aureus, Sreptococcus Pyogenesis (Str. Pyogenesis), Candida albicans (C. albicans) according to the standard procedure.
All women underwent the Papanicolaou test with the conclusion termed the 2003 Bethesda system and a colposcopic study, the findings of which were recorded according to the current international terminology adopted in Rio de Janeiro in 2011. Chronic cervicitis was diagnosed when more than 10 polymorphonuclear leukocytes per high power field of a light microscope were found in the endocervical discharge, while viewing more than five HPF at 1000-fold magnification, and when there were mucopurulent secretions from the cervical canal for over two months [6]. Squamous intraepithelial lesions of the cervix were verified by cytological examination of the cervical epithelium and histological examination of cervical tissue biopsy. The colposcopy-guided cervical biopsy was carried out according to the following indications: abnormal colposcopic pattern and cytological smears type HSIL (high-grade squamous intraepithelial lesions), ASC-H (atypical squamous cells that cannot rule out high-grade squamous intraepithelial lesions), ASC-US (atypical squamous cells of undetermined significance). In the biopsy material, p16 and Ki-67 distribution in the cervical epithelium was determined by layers: in the basal layer, in 1/3 of the epithelial layer and in 2/3 of the cervical epithelial layer. The Ki-67 expression rate was estimated as the ratio between the cervical epithelial cells with stained nuclei and the total number of unstained cells per HPF at 400-fold magnification, measured in percentage according to the following criteria: Ki-67 rate is 5%, 10-15%, 15% and over.
The findings were statistically processed using Statistica for Windows, a special-purpose package for statistical data processing. The χ2 was applied to the cross table where the expected values were at least 10. In other cases, the Fisher exact test was applied. The conventional medical р<0.05 value was used as a benchmark of statistical validity of the findings.
Results and Discussion
Groups with different viral and bacterial flora combinations were formed out of 73 women examined. The microflora combinations are given in Table 1.
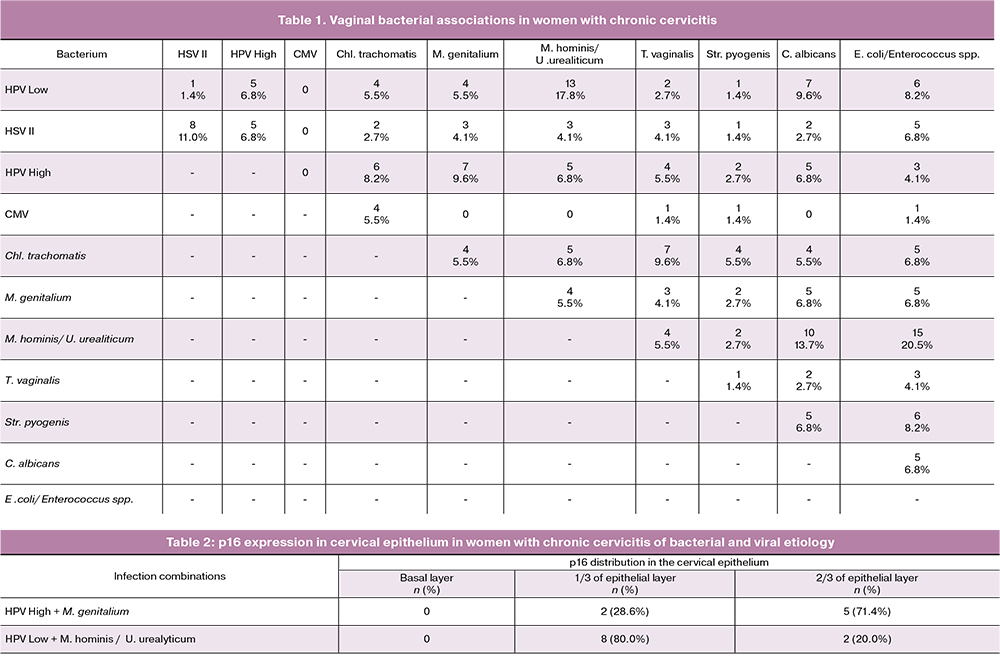
The expression of immunohistochemical markers was comparatively assessed in those groups of women infected with HPV or HSV II where the same bacterial combination was found at least five times. Thus, the study included 41 women, and the groups were compared between the following infection combinations:
- HPV Low +M. hominis / U. urealyticum (n=13);
- HPV High + Chl. trachomatis (n=6);
- HPV High +M. genitalium (n=7);
- HPV High + M. hominis / U. urealyticum (n=5);
- HPV High + HPV Low (n=5);
- HSV II+ intestinal flora: E. coli, Enterococcus spp. (n=5).
Significant differences (p<0.05) in p16 distribution within the epithelial layers of the cervix were obtained by comparing the following bacterial associations (Table 2):
- HPV High + M.genitalium – HPV Low + M. hominis / U. urealyticum (р=0.04).
In this comparison variant, p16 expression was significantly determined in 2/3 of the cervical epithelial layer in women infected with high-risk HPV on a more frequent basis (p<0.05), as compared to women infected with low-risk HPV, which is consistent with the literature data indicating the role of high-risk HPV in the development of dysplasia and cervical cancer [2]. Other comparison variants did not show significant differences in p16 distribution within the cervical epithelial layers (p>0.05).
There were no statistically significant differences in the analysis of Ki-67 expression in women of the studied groups (1-6), p>0.05 is for all of the comparison variants.
Thereby, women with chronic cervicitis and high-risk HPV associated with opportunistic mycoplasmas, herpes simplex virus type II with intestinal flora (E. coli, Enterococcus spp.) and women with high-risk HPV associated with obligate pathogens (Chl. trachomatis, M. genitalium) have a comparable frequency of p16 expression in the cervical epithelial layers and Ki-67 expression rate.
Significant differences (p<0.05) were observed in the following comparison variants in the analysis of Ki-67 distribution in the cervical epithelial layers:
- HPV High+Chl. trachomatis – HPV High+M. hominis / U. urealyticum;
- HPV High+M. genitalium – HPV High + M. hominis / U. urealyticum.
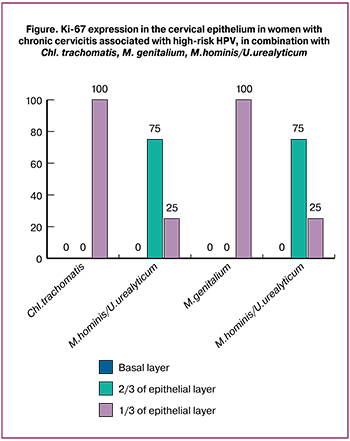 The comparison results are presented in Figure 1 which shows that Ki-67 expression is significantly determined in 2/3 of the cervical epithelial layer (100%) in women with chronic cervicitis associated with high-risk HPV in combination with obligate pathogens (Chl. trachomatis, M. genitalium) on a more frequent basis (p<0.05), as compared to women infected with opportunistic mycoplasmas (25%), whose Ki-67 expression is more often determined in 1/3 of the cervical epithelium (p<0.05).
The comparison results are presented in Figure 1 which shows that Ki-67 expression is significantly determined in 2/3 of the cervical epithelial layer (100%) in women with chronic cervicitis associated with high-risk HPV in combination with obligate pathogens (Chl. trachomatis, M. genitalium) on a more frequent basis (p<0.05), as compared to women infected with opportunistic mycoplasmas (25%), whose Ki-67 expression is more often determined in 1/3 of the cervical epithelium (p<0.05).
As for other comparison variants, including the comparison of HPV High + Chl. trachomatis with HPV High + M. genitalium, there were no significant differences in Ki-67 distribution in the cervical epithelium (p>0.05).
Some authors point to the role of the chlamydial infection as a predisposing HPV infection factor [7, 8] which fosters the development of cervical neoplasia [3]. The study results are consistent with the literature data: Ki-67 expression was significantly determined in 2/3 of the cervical epithelial layer in women with chronic cervicitis associated with high-risk HPV in combination with Chl. trachomatis on a more frequent basis (p<0.05), as compared to women infected with opportunistic mycoplasmas.
According to other authors, any inflammation caused by sexually transmitted infections (Chl. trachomatis, M. genitalium, U. urealyticum, M. hominis) may be a predisposing factor for subsequent HPV infection due to similar routes of infection [9, 10] and, as a consequence, for the development of cervical neoplasia. Our findings are consistent with this opinion. In the comparative analysis of p16 and Ki-67 expression, the women with chronic cervicitis associated with high-risk HPV and infected with obligate pathogens (Chl. trachomatis, M. genitalium) and women infected with opportunistic flora had a comparable frequency of p16 expression in the cervical epithelial layers and Ki-67 expression rate. However, the study findings of Ki-67 distribution in the cervical epithelium differ from the literature data [9, 10]. Thus, Ki-67 expression was significantly determined in 2/3 of cervical epithelium in women infected with Chl. trachomatis or M. Genitalium on a more frequent basis (p<0.05), as compared to women infected with U. Urealyticum, M. hominis. This may indicate the role of Chl. trachomatis and M. genitalium as predisposing factors of HPV infection.
Summary
- Ki-67 distribution in 2/3 of the cervical epithelial layer is four times more frequent in women with chronic cervicitis associated with high-risk HPV and infected with obligate pathogens such as Chl. trachomatis and M. genitalium, as compared to women with chronic cervicitis associated with high-risk HPV and opportunistic mycoplasmas (M. hominis/U. realyticum).
- Women with chronic cervicitis associated with high-risk HPV in combination with Chl. trachomatis and / or M. Genitalium should be included in the risk group for the development of the cervical neoplastic processes.
- When HPV associations and herpes simplex virus type II with bacterial flora are found in women with chronic cervicitis, a therapy aimed at vaginal normocoenosis should be recommended.
- In case of identifying an abnormal colposcopic pattern in women with chronic cervicitis, a histological study of the cervical tissues should be supplemented by the study of Ki-67 expression aimed at differential diagnosis of the severity of neoplasia. The findings will enable to develop a personal pathway for women with mild neoplasia in the setting of chronic cervicitis, based on the childbearing intentions, and will help to reduce the number of unjustified cervical surgeries.
References
- Apolikhina, I.A., Gorbunova, E.A., Dodova, E.G., Gasanova, G.F. Modern aspects of combined antibacterial therapy for nonspecific vaginitis and cervicitis (the results of non-interventional study “Balance”). Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2015; 8: 70-7. (in Russian)
- Maltseva, L.I., Farrakhova, L.N., Akhmetzyanova, A.V. Assessment of HPV-associated chronic cervicitis as a risk factor for development of cervical cancer. Prakticheskaya Meditsina/Practical Medicine. 2012; 9: 73-6. (in Russian)
- Petrova, G.V. Cervical cancer. Changes in the basic statistical measures. In the book: Proceedings of the National Congress “Genital oncology: from prevention and early detection to effective treatment”. M.; 2016: 134. (in Russian)
- Cervical cancer: statistics and prognosis of survivability. [Digital source.] Available at: http://www.oncoforum.ru/o-rake/statistika-raka/rak-sheyki-matki-statistika-i-prognozy-vyzhivaemosti.html Access date: 04.07.2016. (in Russian)
- Aromseree S., Chaiwongkot A., Ekalaksananan T., Kongyingyoes B., Patarapadungkit N., Pientong C. The three most common human papillomavirus oncogenic types and their integration state in Thai women with cervical precancerous lesions and carcinomas. J. Med. Virol. 2014; 86(11): 1911-9.
- Sokolovsky, E.V., Lioznov, D.A., Korneev, I.A., Savicheva, A.M. Clinical guidelines for managing patients with sexually transmittable infections (STIs). Aylamazyan, E.K., ed. St. Petersburg.; 2014. 120p. (in Russian)
- Prilepskaya, V.N., Dovletkhanova, E.R. Chlamydial infection in obstetrics and gynecology. Effective pharmacotherapy. 2014; 35: 28-33. (in Russian)
- Silva J., Cerqueira F., Ribeiro J., Sousa H., Osório T., Medeiros R. Is Chlamydia trachomatis related to human papillomavirus infection in young women of southern European population? A self-sampling study. Arch. Gynecol. Obstet. 2013; 288(3): 627-33.
- Kuznechenkova, T.V., Lysenko, O.V., Iglikov, V.A. Association of urogenital mycoplasmas with genitourinary inflammations in women. In the book: Theses from research papers of the III all-Russian Congress of STD and Skin Specialists. 27-30 October 2009 Kazan; 2009: 84. (in Russian)
- Farag M.A.E., Morad A.W.A., Azzazi A., Fayed S.M., Eldin A.K.Z. Association between genital mycoplasma and cervical squamous cell atypia. Middle East Fertil. Soc. J. 2013; 18(4): 241-5.
Received 05.10.2017
Accepted 27.10.2017
About the Authors
Bokach, Olga M., obstetrician-gynecologist, Family Planning Center “Medica”.194017, Russia, St. Petersburg, Maurice Thorez Avenue 72. Tel.: +79117459631. E-mail: Olga.bokach634@yandex.ru
Selkov, Sergey A., professor, head of the Department of Immunology and Intercellular Interactions of the D.I. Ott Institute of Obstetrics, Gynecology and Reproductology. 199034, Russia, St. Petersburg, Mendeleevskaya line 3. Tel.: +78129553045. E-mail: selkovsa@mail.ru
Niauri Dariko Aleksandrovna, professor, head of Department of Obstetrics, Gynecology and Reproductology of the medical faculty of St. Petersburg State University.
199034, Russia, Saint-Petersburg, Mendeleevskaya line 3. Tel.: +79219196950. E-mail: d.niauri@mail.ru
Tishkov Artem Valerievich, associate professor, head of Physics, Mathematics and Informatics Department of the Pavlov First Saint Petersburg State Medical University. 197022, Russia, St. Petersburg, St. L. Tolstoy, 6-8. Tel.: +79219529185. E-mail: artem.tishkov@gmail.com
For citations: Bokach O.M., Niauri D.A., Tishkov A.V., Selkov S.A. Features of the expression of the immunohistochemical markers P16 and KI67 in women with chronic cervicitis associated with bacterial and viral infections. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (9): 85-90. (in Russian)
https://dx.doi.org/10.18565/aig.2018.9.85-90