Evaluation of human papillomavirus infection in women in the Lipetsk Region, by using a diagnostic self-sampling test
Objective. To improve cervical cancer screening programs via clinical introduction of a diagnostic vaginal swab self-sampling test for the detection of high-risk human papillomavirus (hrHPV).Apolikhina I.A., Bashirova L.K., Letnikova L.I., Khudyakova O.V., Ivanov S.V., Gorbunova E.A., Dolgushina N.V.
Subjects and methods. A total of 455 residents of the Lipetsk Region were examined; vaginal swabs tested for HPV were taken both independently by a woman with a Qvintip device and by a gynecologist with a universal urogenital probe. The women were asked whether it was convenient for them to self-collect a vaginal swab.
Results. In the surveyed sample of 455 women, there were 35 (7.7%) cases of hrHPV identified on the swabs collected by the Qvintip and 38 (8.4%) women with hrHPV detected on those taken by the physician, out of them 26 (68.5%) women had atypical squamous cells of undetermined significance. 70.3% of women preferred the Qvintip self-sampling method.
Conclusion. The Qvintip self-sampling method for hrHPV testing shows high diagnostic efficiency, simplicity, and ease-to-use. The method may be recommended for the detection of hrHPV to increase cervical cancer screening coverage.
Keywords
Cervical cancer (CC) is the fourth most common malignant disease among women [1, 2]. Slow progression of the disease (over several years), the presence of several stages of precancerous conditions and the relative availability of a tumor for manipulations provide ample opportunities for the timely diagnosis and prevention of cervical cancer. Cervical cancer screening most often involves the diagnosis of high-risk human papillomavirus (hrHPV) using DNA or RNA analysis, or searching for cytological and/or molecular markers of the malignant process in cervical cells (Pap test) [3-5].
Highly sensitive PCR (polymerase chain reaction) tests, that can detect HPV DNA, are of great interest today. They are 40% more sensitive in screening than a cytological smear [4, 5]. However, despite the higher sensitivity, PCR diagnostics does not allow to distinguish a clinically significant HPV infection from a clinically insignificant one. Cytological screening also has certain limitations (high individual and general variability, limited sensitivity, high cost, and limited screening coverage) [6].
Currently, the combined use of oncocytological smear and hrHPV-DNA testing is considered to be the best approach for detecting malignant and precancerous conditions of the uterine cervix [7]. In the case of positive test results, the patient is recommended to undergo colposcopy in order to identify the boundaries of pathological areas and subsequent actions (biopsy, conization, excision).
In economically developed countries, nowadays screening for HPV is included in the cervical cancer prevention program as a primary screening. There is a need for an objective and easily reproducible molecular technique of baseline screening for the primary selection of patients with clinically significant pathology. At the same time, while implementing cervical cancer screening programs it is important to use standardized and clinical validated methods: НС 2 , GP 5 +/ 6 + PCR, COBAS 4800 HPV. The use of p16INK4a/Ki-67 dual-staining is also considered as an optimal alternative. However, this method is expensive [8, 9]. In addition, it was shown that p16 may not have sufficient discriminatory capacity, since normal cells also express p16 (albeit less intensely).
Accordingly, nowadays the search for the best screening method is still urgent. However, biomarkers with a high prognostic value (in particular, biomarkers that allow assessing the likelihood of developing cervical carcinoma at the stage of cervical intraepithelial neoplasia (CIN) 2, when treatment is highly effective) have not been found to date [10, 11]. In addition, it is expected that a biomarker panel will be required for the examination capable of distinguishing between CIN stages with high sensitivity and specificity.
A significant obstacle to the implementation of screening programs aimed at preventing cervical cancer is women’s unwillingness to visit a gynecologist. It is due to unpleasant sensations during material sampling for cytological research. Therefore, in recent years, various tools have been provided for self-sampling of vaginal discharge for HPV testing and a number of studies have been conducted to assess their diagnostic effectiveness, convenience and comfort in use, as well as the cost of the method [12, 13].
In 2014, Arbyn M. et al. showed that hrHPV-DNA test by self-sampling makes it possible to include in the screening program those patients, who usually do not participate in regular cytological screening programs [12]. It was noted that self-sampling of the material allows increasing the percentage of target group patients participating in the screening with high efficiency. In addition, it allows expanding the coverage of patients during cervical cancer screening [14].
In many studies involving patients of different ethnic groups, it has been shown that self-sampling with brushes and tampons for obtaining smear or swab is an effective method of sampling the material for subsequent DNA genotyping, cytological or immunohistochemical studies [12]. Self-sampled material is most often placed in a liquid buffer [15]. However, there are also options for dry storage, for example, in an airtight container or by applying a sample on paper containing special chemical reagents. These reagents lyse the cells upon contact, which prevents the possibility of infecting upon contact with the sample and makes it safer and easier for transportation. Then the sample is sent to the laboratory for further analysis.
Thus, self-testing of the cervicovaginal discharge will compensate for a number of factors preventing from the patients’ participation in cervical cancer screening programs. Among them there are practical factors (busy schedule of the patient, the need to visit a medical institution), emotional factors (fear of pain and embarrassment of the patient) and cognitive factors (lack of patient’s awareness of the true risk level, seeming lack of disease symptoms) [16]. It is optimal to use the same independently obtained sample to detect several biomarkers, which requires minimal effort from the patient.
The research goal was to study the prevalence of hrHPV in women of different age groups in the Lipetsk region and to improve the cervical cancer screening programs by introducing a diagnostic self-sampling HPV test into clinical practice.
Materials and Methods
To achieve this goal, a study was conducted in which 455 women were examined. A random stratified sample of the Lipetsk region residents was formed, taking into account the age and place of residence (city/village). The selection of 3 clusters from 20 clusters was done according to the table of random numbers. They were the following: Gryazinsky (urban), Dankovsky (rural) and Izmalkovsky (rural). The sample size was calculated using the WinPepi program, taking into account the estimated prevalence of cervical cancer in the Russian Federation and 95% confidence interval (CI). Within 3 months of enrollment, 455 patients were included in the study.
The criteria for inclusion in the study were age from 21 to 65 years, the presence of registration or living in migrant status in the Lipetsk region during 3 or more years, signed informed consent to participate in the study, fluency in Russian, informed voluntary consent of the patient, the presence of the medical insurance policy.
The exclusion criteria were the absence of the cervix due to surgery, malformations of the uterus and cervix (doubling, aplasia of the uterus or vagina), stricture of the vagina, lack of sexual life in the history, pregnancy at the time of participation in the study, intravaginal injection of drugs or the use of spermicides less than 7 days before the start of the study, mental illness, poor-quality sampling of the material that did not allow to do HPV testing and cytological study of uterine cervix, as well as women who wereundergoing treatment for cervical cancer.
All participants were informed on the objectives and features of the study and familiarized with the instructions for use of the Qvintip device. At the first visit, the study participants were given a kit consisting of a plastic applicator and a small plastic tube. The material was sampled by inserting the applicator deep into the vagina, turning the stick once around its axis and removing the applicator (figure). Then the applicator tip with the sample was placed into a test tube, which was returned to the doctor-researcher at the antenatal clinic, from where it was transported to the laboratory for research. During the first visit, all 455 women were asked to sign an informed consent to participate in the study. All aspects of the study as well as the rights of the subjects were explained and confidentiality of data was guaranteed. Further, study participants were asked to fill in a questionnaire, which reflected the anamnesis data and possible risk factors for developing cervical cancer; it was filled in with the help of a doctor.

The sampling of material for hrHPV testing was performed both by a woman herself from the vagina by means of the Qvintip device (according to the instructions) and by a gynecologist from the cervical canal with the help of universal urogenital probe. The material obtained by the doctor was placed in Eppendorf-type tube with the transport medium; the material selected by the patient was placed in a dry tube without transport medium (according to the Qvintip instructions).
Both samples were examined at the Center for Bacteriological Research of the State Healthcare Institution “Regional Dermatovenerologic Dispensary” in Lipetsk using PCR in real time in the scrape of epithelial cells; reagents were produced by InterLabService Ltd. for detecting hrHPV (16, 18, 31, 33, 35, 39, 45, 52, 58, 59, 67). It was a qualitative test (without determining viral load).
According to examination results, 38 women with positive hrHPV were invited to the second visit. The smear was taken for oncocytological examination. The examination was conducted on the basis of the State Healthcare Institution “Lipetsk Oncology Center”. The Papanicolau staining technique was used, and scrapings from the surface of endocervix and exocervix served as the test material. The smear was placed on two glass slides. The standardized cytology protocol was based on the International Colposcopic Terms classification approved by the 14th IFCPC World Congress in July, 2011 (Rio de Janeiro) BETESDA.
At the third visit, these 38 patients were reported the results of oncocytological examination. Then colposcopy was performed.
Self-sampling and medical sampling of the vaginal discharge for HPV-test were assessed according to the data of a survey of the women about comfort, pain, confidentiality and sensations according to the rating system: “yes - no”.
Statistical processing of the data obtained was performed using the software package Statistica 10 (StatSoft Inc., USA). The distribution of results included in the statistical analysis was assessed for normality. The descriptive statistics of qualitative attributes are represented by absolute and relative frequencies of values. Comparison of groups by qualitative signs was performed using the chi-square test and Fisher’s exact test.
Results
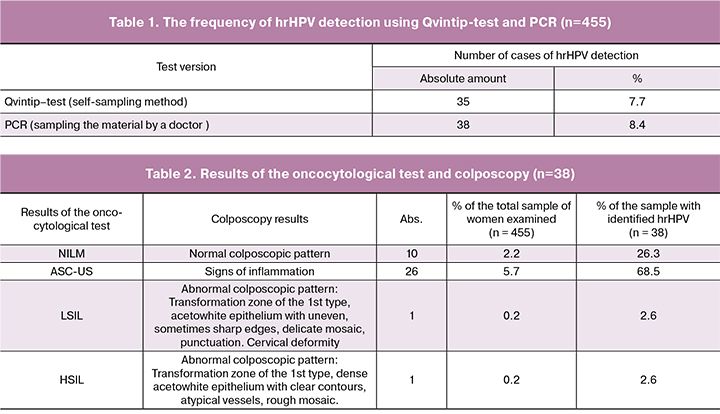
Table 1 presents the absolute and relative number of patients with a positive hrHPV test. As can be seen from the Qvintip test, in the sample of 455 women from the Lipetsk region, 35 such patients were identified (mean age was 31.5 ± 7.2 years), which amounted to 7.7%. The results of PCR in the case of sampling the material by a doctor showed the proportion of patients with identified hrHPV at the level of 8.4%, that is 38 cases. Analysis of HPV-test data showed similar efficacy of the examination using the Qvintip device, as in the case of sampling the material by a doctor.
The social characteristics of patients with positive hrHPV-test and patients not infected with HPV were not significantly different, their average age was comparable: in the group of women with hrHPV-infecting, its value was 30.5 ± 6.4 years, and in HPV-negative patients its value was 32.1 ± 7.8 years. There were also no statistically significant differences in the age of menarche and coitarche, the menstrual function characteristics, the presence of bad habits (smoking), the use of different methods of contraception and the number and outcome of pregnancies. No significant differences were found in the presence of somatic diseases.
Table 2 presents the results of oncocytological test and colposcopy, which were carried out in 38 patients with a positive hrHPV-test, taken by a doctor from the entire sample of subjects. It was found that the number of women with atypical squamous cells of undetermined significance (ASC-US) was the maximum and amounted to 26 cases, that is 68.5% (5.7% of the entire sample). There was one case of low-grade squamous intraepithelial lesions (LSIL) and one case of high-grade squamous intraepithelial lesions (HSIL), amounted to 2.6% (0.2% of the total sample). The number of women with no intraepithelial changes and malignant processes (NILM) was 10, that is 2.2% (26.3% of the entire sample).
In women with NILM, a normal colposcopic pattern was observed, and in the case of ASC-US detection the subjects showed the signs of inflammation. In a woman with LSIL, an abnormal colposcopic pattern (acetowhite epithelium with uneven, sometimes sharp edges, delicate mosaic and punctuation) was revealed, and cervical deformity was noted. In the subject with HSIL, the abnormal colposcopic pattern was manifested due to the presence of dense acetowhite epithelium with a clear contour, atypical vessels, mosaic and punctuation.
Later, a complex of medical diagnostic and prophylactic measures was taken in relation to these subjects. At the same time, women with ASC-US and LSIL were recommended to be monitored at the place of residence with the conduction of Pap-test, extended colposcopy and testing for HPV after one year. A patient with HSIL was offered treatment at the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov. Laser vaporization was carried out; the result of HPV control test after 6 months was negative.
One of the research objectives was also the evaluation of comfort and convenience when using two compared methods of sampling the material for HPV-test. The evaluation was according to a questionnaire survey of women included into the sample under study. It was found that 320 of 455 (70.3%) patients preferred the method of self-sampling of the material for HPV-test using the Qvintip device; the proportion of the women who reported that they would have preferred sampling by a doctor was 29.7%, 135 patients (p < 0.001).
Discussion
According to the research results in the cohort of examined women, who were residents of the Lipetsk region at the age of 21–65 years, the detection rate of hrHPV was 7.7–8.4%.
It is now generally recognized that the prevalence of papillomavirus infection in various populations is determined not only by medical, but also by other factors: age, socio-economic level of society, methods of contraception used, vaginal biotope, and somatic health of patients [17, 18]. Nowadays the main directions for improving cervical cancer screening programs are the increase in the number of examined women and the improvement of hrHPV typing techniques [2, 6]. At the same time, the frequent reasons why women in different countries avoid participating in screening are fear of pain during gynecological examination and fear of a positive result [19, 20].
According to the results of a number of studies conducted in recent years in different countries, it has been shown that women who have not previously undergone screening for cervical cancer prefer self-sampling [20, 21]. The high compliance of women to this method has been found out. For example, in the Scandinavian countries, the number of women who preferred self-sampling of the material for HPV-test was three times higher than the corresponding number of women who came for examination by a specialist. During the survey, the subjects reported that the main reason for their choice was discomfort associated with gynecological examination [22].
Our data are consistent with the results of other researchers. When evaluating the convenience and acceptability of the method of self-sampling of the material for the HPV test using the Qvintip device, 70.3% of patients preferred the method of self-sampling of the material. At the same time, the proportion of women who reported that they would prefer sampling by a doctor was statistically significantly less, it was 29.7% [23].
In the study conducted by Belokrinitskaya T.E. et al. (2017), it was shown that the use of the Qvintip device increases the possibility of detecting hrHPV in the genital tract by 1.6 times compared with sampling the material by a doctor (38% vs. 27.5%). In the case of self-sampling of vaginal discharge using Qvintip, the HPV test was positive 3.8 times more often than in the case of sampling the material by a doctor with the help of genital probe (36.3% and 9.5%). In our study most of the women included in the examination indicated the ease of the device use, the painlessness and privacy of the Qvintiр method [24].
Currently, many authors believe that self-sampling of the material for hrHPV -test can act as an alternative method for cervical cancer screening, which will significantly increase the coverage of population participating in screening programs [16, 21]. At the same time, researchers agree on the need for further research to improve the technical aspects and evaluation of clinical and economic characteristics of using this method in clinical and epidemiological practice.
Conclusion
Thus, high diagnostic efficiency, simplicity and ease of use are typical for the Qvintip device intended for self-sampling of the material for hrHPV testing. The method can be recommended for hrHPV detection in order to increase the coverage of cervical cancer screening programs.
References
1. Левшин В.Ф., Завельская А.Я. Факторы риска и профилактика рака шейки матки. Вопросы онкологии. 2017; 63(3): 506-16. [Levshin VF, Zavelskaya A.Ya. Risk factors and prevention of cervical cancer. Voprosy onkologii. 2017; 63 (3): 506-16. (in Russian)]
2. Crossley B., Crossley J. A review of the use of human papilloma virus (HPV) in cervical screening. Br. J. Biomed. Sci. 2017; 74(3): 105-9.
3. Cummings M.C., Marquart L., Pelecanos A.M., Perkins G., Papadimos D., O’Rourke P. et al. Which are more correctly diagnosed: conventional Papanicolaou smears or Thinprep samples? A comparative study of 9 years of external quality-assurance testing. Cancer Cytopathol. 2015; 123(2): 108-16.
4. Tjalma W.A. The ideal cervical cancer screening recommendation for Belgium, an industrialized country in Europe. Eur. J. Gynaecol. Oncol. 2014; 35(3): 211-8.
5. Ronco G., Dillner J., Elfström K.M., Tunesi S., Snijders P.J., Arbyn M. et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014; 383(9916): 524-32.
6. Saslow D., Solomon D., Lawson H.W., Killackey M., Kulasingam S.L., Cain J. et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. Am. J. Clin. Pathol. 2012; 137(4): 516-42.
7. Zhou H., Mody R.R., Luna E., Armylagos D., Xu J., Schwartz M.R. et al. Clinical performance of the Food and Drug Administration-Approved high-risk HPV test for the detection of high-grade cervicovaginal lesions. Cancer Cytopathol. 2016; 124(5): 317-23.
8. Benevolo M., Allia E., Gustinucci D., Rollo F., Bulletti S., Cesarini E. et al. Interobserver reproducibility of cytologic p16INK4a/Ki-67 dual immunostaining in human papillomavirus positive women. Cancer Cytopathol. 2017; 125(3): 212-20.
9. Uijterwaal M.H., Polman N.J., Witte B.I., van Kemenade F.J., Rijkaart D., Berkhof J. et al. Triaging HPV-positive women with normal cytology by p16/Ki-67 dual-stained cytology testing: baseline and longitudinal data. Int. J. Cancer. 2015; 136(10): 2361-8.
10. Koeneman M.M., Kruitwagen R.F., Nijman H.W., Slangen B.F., Van Gorp T., Kruse A.J. Natural history of high-grade cervical intraepithelial neoplasia: a review of prognostic biomarkers. Expert Rev. Mol. Diagn. 2015; 15(4):527-46.
11. Ebisch R.M., Siebers A.G., Bosgraaf R.P., Massuger L.F., Bekkers R.L., Melchers W.J. Triage of high-risk HPV positive women in cervical cancer screening. Expert Rev. Anticancer Ther. 2016; 16(10): 1073-85.
12. Arbyn M., Verdoodt F., Snijders P.J., Verhoef V.M., Suonio E., Dillner L. et al. Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta-analysis. Lancet Oncol. 2014; 15(2): 172-83.
13. Chen K., Ouyang Y., Hillemanns P., Jentschke M. Excellent analytical and clinical performance of a dry self-sampling device for human papillomavirus detection in an urban Chinese referral population. J. Obstet. Gynaecol. Res. 2016; 42(12): 1839-45.
14. Tamalet C., Le Retraite L., Leandri F.X., Heid P., Garnier H.S., Piana L. Vaginal self-sampling is an adequate means of screening HR-HPV types in women not participating in regular cervical cancer screening. Clin. Microbiol. Infect. 2013; 19(1): 44-50.
15. Dijkstra M.G., Heideman D.A., van Kemenade F.J., Hogewoning K.J., Hesselink A.T., Verkuijten M.C. et al. Brush-based selfsampling in combination with GP5+/6+-PCR-based hrHPV testing: high concordance with physician-taken cervical scrapes for HPV genotyping and detection of high-grade CIN. J. Clin. Virol. 2012; 54(2): 147-51.
16. Arrossi S., Ramos S., Straw C., Thouyaret L., Orellana L. HPV testing: a mixed-method approach to understand why women prefer self-collection in a middle-income country. BMC Public Health. 2016; 16: 832.
17. Bosch F.X., Broker T.R., Forman D., Moscicki A.B., Gillison M.L., Doorbar J. et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine. 2012; 31(Suppl. 7): H1-31.
18. Белокриницкая Т.Е., Фролова Н.И., Тарбаева Д.А., Глотова Е.Ю., Золотарёва А.А., Мальцева Т.В. Конфаундинг-факторы папилломавирусной инфекции и цервикальной дисплазии у молодых женщин. Доктор.Ру. 2015; 14: 7-11. [Belokrinickaya T.E., Frolova I.I., Tarbaeva D.A. i dr. Confounding factors of papillomavirus infection and cervical dysplasia in young women. Doctor. RU. 2015; 14 (115): 7-12 (in Russian)].
19. Zehbe I., Jackson R., Wood B., Weaver B., Escott N., Severini A. et al. Community-randomised controlled trial embedded in the Anishinaabek Cervical Cancer Screening Study: human papillomavirus self-sampling versus Papanicolaou cytology. BMJ Open. 2016; 6(10): e011754.
20. Ortiz A.P., Alejandro N., Pérez C.M., Otero Y., Soto-Salgado M., Palefsky J.M. et al. Acceptability of Cervical and Anal HPV Self-sampling in a sample of Hispanic women in Puerto Rico. P R Health Sci. J. 2012; 31(4): 205-12.
21. Darlin L., Borgfeldt C., Forslund O., Hénic E., Hortlund M., Dillner J. et al. Comparison of use of vaginal HPV self-sampling and offering flexible appointments as strategies to reach long-term non-attending women in organized cervical screening. J. Clin. Virol. 2013; 58(1): 155-60.
22. Verdoodt F., Jentschke M., Hillemanns P., Racey C.S., Snijders P.J., Arbyn M. Reaching women who do not participate in the regular cervical cancer screening programme by offering self-sampling kits: a systematic review and meta-analysis of randomised trials. Eur. J. Cancer. 2015: 51(16): 2375-85.
23. Аполихина И.А., Филиппенкова Е.В., Додова Е.Г., Гасанова Г.Ф., Горбунова Е.А. Современные возможности организованного скрининга рака шейки матки. Акушерство и гинекология. 2016; 9: 12-8. [Apolikhina IA, Filipenkova EV, Dodova EG, i dr. Current possibilities of organized screening of cervical cancer. Akusherstvo i ginekologiya. 2016; 9: 12-8 (in Russian)].
24. Белокриницкая Т.Е., Фролова Н.И., Туранова О.В., Шемякина К.Н., Плетнева В.А., Самбуева Н.Б., Мальцева Е.Е. Результативность и приемлемость обследования на вирус папилломы человека при самостоятельном и врачебном заборе вагинального отделяемого. Акушерство и гинекология. 2017; 2: 97-105. [Belokrinickaya T.E., Frolova N.I., Turanova O.V. i dr. Effectiveness and acceptability of examination for the human papillomavirus virus in an independent and medical fence of the vaginal discharge. Akusherstvo i ginekologiya. 2017; 2: 97-105 (in Russian)].
Received 06.04.2018
Accepted 20.04.2018
About the Authors
Apolikhina, Inna A., MD, head of the Department of Aesthetic Gynecology and Rehabilitation of Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Professor of the Department of Obstetrics, Gynecology and Perinatology of the I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation Ministry of Health of the Russian Federation (Sechenov University), e-mail: i_apolikhina@oparina4.ruBashirova, Lala K., competitor of a scientific degree of candidate of science at the Department of Obstetrics, Gynecology, Perinatology and Reproductology of the Institute
of Vocational Education of Federal State Autonomous Educational Institution of Higher Education I.M. Sechenov First Moscow State Medical University of the Ministry
of Health of the Russian Federation (Sechenov University), e-mail: leyla9296@hotmail.com
Letnikova, Lyudmila I., deputy head of administration of the Lipetsk region, address: 6 Zegel str., Lipetsk, Lipetsk region, 398050
Hudyakova, Olga V., consultant of the department of organization of medical care for children and the obstetric aid service of the health department of the Lipetsk region
Ivanov, Sergey A., head of the department of organization of medical care for children and the obstetric aid service of the health department of the Lipetsk region
Gorbunova, Elena A., obstetrician-gynecologist, physiotherapist of the Department of Aesthetic Gynecology and Rehabilitation of the National Medical Research Center
for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov.
Dolgushina, Natalia V., MD, head of the department of scientific planning and audit of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov.
For citations: I.A. Apolikhina, L.K. Bashirova, L.I. Letnikova, O.V. Khudyakova, S.V. Ivanov, E.A. Gorbunova, N.V. Dolgushina. Evaluation of human papillomavirus infection in women in the Lipetsk Region, by using a diagnostic self-sampling test. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (11): 98-104. (in Russian)
https://dx.doi.org/10.18565/aig.2018.11.98-104