Assessment of effectiveness of treatment in pregnant women with pyelonephritis
Relevance of the issue. High prevalence of pyelonephritis (up to 10%) in pregnant women is an acute problem. The issues of pathogenesis, early diagnosis, prevention of recurrence of the disease remain unsolved. Due to anatomical and physiological changes in the body during pregnancy, urinary tract infection becomes complicated, and effective therapy is especially important.Khudovekova A.M., Mozgovaya E.V., Nagorneva S.V., Prokhorova V.S., Selkov S.A., Chepanov S.V.
Aim. Optimization of treatment and prevention of recurrent pyelonephritis in pregnant women.
Materials and methods. 60 pregnant women with gestational pyelonephritis and acute chronic pyelonephritis, who received standard antibiotic therapy. Additionally, the patients in the main group (n = 30) were prescribed systemic enzyme therapy (Wobenzym). Before and after therapy, all patients underwent Doppler ultrasound examination to determine the blood flow rates in renal and interlobar arteries.
Results. The women in both groups were comparable in terms of age, gestation period and clinical characteristics of the disease. Before treatment blood flow indices in renal and interlobar arteries were high in both groups. However, in the group of women, who received Wobenzym, Doppler iindices for blood flow were of normal range in the renal artery (p=0.004) and in the interlobar artery (p=0.001), while standard therapy did not show statistically significant differences. Adding Wobenzym to therapy increased the chances for normalization of the blood flow in renal artery by 7 times (95% CI: 1,38–35,5; p=0,01). Systemic enzyme therapy reduced the recurrence of the disease by 4,5 times (95% CI: 1,09–18,5) compared to the comparison group (p=0.0287).
Conclusion. Thus, the use of Wobenzym in complex therapy versus standard therapy had a beneficial effect on statistically significant improvement in renal blood flow and a decrease in the frequency of recurrence of the disease.
Keywords
Pyelonephritis is one of the most common kidney diseases in pregnant women. It is an extragenital disorder causing inflammation, which predominantly damage the interstitial tissue due to specific bacterial infection and involving the renal pelvis and calyces in the inflammatory process [1].
In the absence of treatment of the lower urinary tract infections, pyelonephritis develops in 20–40% of pregnant women. The disease can lead to complications during pregnancy and childbirth, such as preeclampsia (44%), anemia in pregnant women (64%), preterm births (17%) and intrauterine infections (8.4%). According to some publications, the incidence of pyelonephritis in pregnant women may vary from 1–2.5% to 10%, and relapses are noted in 10–30% of patients. In every third case, pyelonephritis occurs for the first time during pregnancy or in the postpartum period [2, 3].
Pyelonephritis in the first trimester of pregnancy occurs relatively rare (up to 5%). In most cases, it develops in the second and the third trimesters (65– 80%) or in the postpartum period (up to 25% of cases) with right kidney damage in 65–75% of cases [4, 5].
The choice of tactics is still disputable. Over the past few years, an increasing trend in antibiotic resistance to urinary tract infections is noted. Antibiotic resistance dictates the need for dynamic monitoring of treatment and prevention of urinary tract infections [6].
Recent studies presented convincing evidence that impaired humoral and cellular immunity is an important link in the pathogenesis of gestational pyelonephritis and development of chronic pyelonephritis. Immunosuppression observed in normal pregnancy aggravates in pyelonethritis. Immunodeficiency is found in vast majority of pregnant women with pyelonephritis. There is a marked decrease in T-lymphocytes and an increasein B-lymphocytes. Immunereactivity(phagocytic activity of leukocytes) decreases, nonspecific defense factors (complement and concentration of lysozyme) are inhibited. Increased circulating immune complexes levels are noted. The impairment of immunity is likely due to the persistent course of pyelonephritis, even in the absence of previous urogenital pathology. [7].
Therefore, it is very important to use immunomodulatory agents to prevent recurrent urinary tract infections. Wobenzym included in the complex therapy of pyelonephritis in this study is a systemic enzyme therapy drug, and according to the published data, has a positive effect on cellular and humoral immunity [8].
Aim of the study. Optimization of treatment and prevention of recurrent pyelonephritis in pregnant women.
Materials and methods
60 pregnant women with upper urinary tract infection (gestational pyelonephritis or exacerbation of chronic pyelonephritis) were included in the study. They were divided into two groups: the main group and the comparison group. During the study all patients underwent renal Doppler ultrasonography and assessment of blood flow in renal and interlobar arteries. Inclusion criteria: pregnant women in the third trimester, aged 18–40 years, voluntary informed consent to participate in the study. Exclusion criteria: diabetes mellitus, preeclamsia (including in medical history), complicated urinary tract infection requiring surgical intervention (acute hydronephrosis, purulent exudate in the urinary tract), autoimmune diseases.
The main group included 30 pregnant women at 29–37 weeks of gestatation, who received combination therapy with the use of antimicrobial therapy, herbal uroseptics and Wobenzym (5 tablets 3 times a day for two weeks). The comparison group included 30 pregnant women at 28–37 weeks of gestation. They received standard therapy without immunomodulatory drugs. Along with clinical examination all patients underwent urine culture test to determine antibiotic susceptibility. The number of days from onset of symptoms, the number of exacerbations of pyelonephritis for the last 6 months before the start of the study, as well as after treatment up to labor onset, the presence of the bacterial agents of urinary tract infections based on urine culture results were assessed in all pregnant women.
Doppler ultrasound was used to assess the blood flow in renal and interlobar arteries. The renal artery was visualized in the sagittal section of kidney using Doppler colour flow mapping. Further, division of the artery into segmental arteries was observed, which then subdivided into interlobar arteries. First, renal artery blood flow was assessed, then in one of the interlobar arteries. Resistance indices (RI) in these arteries were used to analyze the results of Doppler measurements. Normal values of RI were 0.5–0.7, as adopted by the majority of Russian and foreign authors [9].
Statistical analysis
Database collection, statistical processing and design of the material was carried out using Microsoft Office 2016 and Statistica 10.0 sofrware. Normality of distribution was checked using the Kolmogorov– Smirnov test, equality of variances using Levene’s test. Continuous variables with normal distribution were described – using mean (M) and standard deviation (SD): M (SD). Abnormally distributed data were described using median (Me) and quartiles: Me (Q1–Q3). Comparison of independent normally distributed variables was carried out using Student's test, deviation of a normal distribution – using Mann–Whitney test. The statistical significance of differences between quantitative dependent variables in abnormal distribution was assessed using the Wilcoxon test. The differences were considered statistically significant at p<0.05. When statistically significant differences were found between the nominal variables, Pearson’s χ2-test was used, followed by building of four-fold contingency table and the calculation of the odds ratio (OR).
Results
60 pregnant women with gestational pyelonephritis or exacerbation of chronic pyelonephritis were studied. They were comparable in terms of age and gestation period. The age of patients was 22–40 years: in the main group – 31,6 (4,97) years, in the comparison group – 30,6 (5,2) years. Gestation period was 28–37 weeks: in the main group – 31,5 (3,73) weeks, in the comparison group – 32,8(2, 33) weeks. The average number of days from symptoms onset to starting therapy in the main group was 4 (3–5) days and in the comparison group – 3 (2–4) days. Relapses for the 6 months were noted in 30.2% of patients in the main group and in 23.3% of patients – in the comparison group.
Doppler sonography used for renal blood flow assessment showed that blood flow values tended to increase both in renal and interlobar arteries in both groups before treatment, but there were no statistically significant differences between the groups (Table1).
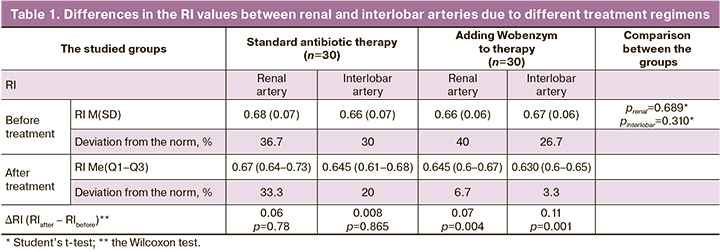
After treatment, there was a statistically significant decrease in the renal (p=0.007) and in the interlobar (p=0,001) arteries only in the group of patients, who took Wobenzym in complex therapy, whereas in standard therapy these values only tended to decrease.
Further, four-fold contingency tables were built to assess the effectiveness of Wobenzym added to standard treatment of the disease (Table 2).
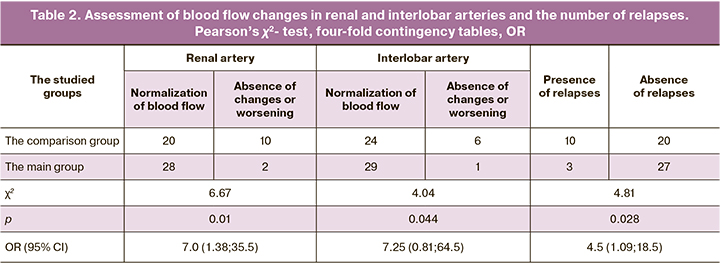
The assessment of the dynamics of renal blood flow changes depending on the type of therapy showed statistically significant differences both in the renal artery (p=0.01) and in the interlobar artery (p=0.044). The chances to normalize the blood flow in renal artery increased by 7 times, when Wobenzym was added to therapy (95% CI: 1.38–35.5); however, in the interlobar artery, 95% CI – OR 7.25 (0.81–64.5), the intersection was 1. This makes the statistical significance of this indicator doubtful.
When comparing the frequency of relapses depending on therapy, statistically significant differences were obtained (p=0.028). The chances of recurrence of pyelonephritis after treatment with Wobenzym before delivery in the main group was 4.5 times less frequent than in the comparison group (95% CI: 1.09– 18.5).
Discussion
Urinary tract infections are among the most common infectious diseases during pregnancy and are the cause of 1 hospitalized patient in 10 cases of hospitalizations during pregnancy. Pyelonephritis during pregnancy can lead to the development of serious maternal and fetal complications, such as anemia, arterial hypertension, sepsis, premature birth, low birth weight. Therefore, timely diagnosis and treatment determines the prognosis for both the mother and the fetus.
Over the past few years, the increasing trend in resistance of causative pathogens in pyelonephritis to antibacterial drugs traditionally used in treatment of such infections is noted. Thus, to prevent progression of acute pyelonephritis to a chronic form, it is necessary to administer complex therapy including antimicrobial therapy, herbal uroseptics, antioxidants, eubiotics, as well as immunomodulatory drugs prescribed for pregnant women, who are prone to exacerbation of chronic pyelonephritis. This study showed, that the use of Wobenzym in complex therapy with antibiotics in pregnant women is more effective compared to the use of only antimictobial drugs. The therapeutic effect of Wobenzym is associated with normalization of renal blood flow affected by improvement in blood rheology.
Conclusion
The study showed that combination therapy of pyelonephritis in pregnant women using Wobenzym leads to a statistically significant improvement in blood flow in renal arteries and a decrease in the number of relapses.
References
- Горин В.С., Ким В.Л., Серебренникова Е.С. Беременность и хронический пиелонефрит: клинические и иммунологические аспекты (обзор). Российский вестник акушера-гинеколога. 2016; 16(5): 19-28. [Gorin V.S., Kim V.L., Serebrennikova E.S. Pregnancy and chronic pyelonephritis: Clinical and immunological aspects (a review). Russian Bulletin of Obstetrician-Gynecologist. 2016; 16(5): 19-28. (in Russian)]. http://dx.doi.org/10.17116/rosakush201616519-28.
- Каптильный В.А. Инфекция мочевыводящих путей во время беременности. Архив акушерства и гинекологии им. В.Ф. Снегирева. 2015; 2(4): 10-9. [Kaptilnyy V.A. Urinary tract infection in pregnancy. Archive of Obstetrics and Gynecology named after V. F. Snegirev. 2015; 2(4): 10-9.(in Russian)].
- Боташев М.И., Байрамкулов У.М., Ураскулов А.Б., Семенов А.Р., Коркмазов А.М. Особенности лечения острого пиелонефрита беременных. Дискуссионные статьи. Вестник урологии. 2019; 7(4): 29-34.https://dx.doi.org/10.21886/2308-6424-2019-7-4-29-34. [Botashev M.I., Bayramkulov U.M., Uraskulov A.B., Semenov A.R., Korkmazov A.M. Acute pyelonephritis in pregnant women: features of treatment. Urology Herald. 2019; 7(4): 29-34. (in Russian)]. https://doi.org/10.21886/2308-6424-2019-7-4-29-34.
- Михайлова О.И., Арушанова А.Г., Аношин А.С., Кан Н.Е., Тютюнник В.Л. Принципы антибактериальной терапии при инфекции мочевыводящих путей у беременных. Акушерство и гинекология: новости, мнения, обучение. 2016; 2: 12-7. [Mikchailova O.I., Arushanova A.G., Anoshin A.S., Kan N.E., Tyutyunnik V.L. Antibacterial therapy principles of urinary tract infections in pregnant women. Obstetrics and Gynecology: News. Opinions. Training. 2016; 2: 12-7. (in Russian)].
- Курбаналиев Х.Р., Чернецова Г.С. Пиелонефрит беременных. Современный взгляд урогинекологов. Вестник Киргизско-Российского славянского университета. 2017; 17(7): 33-6. [Kurbanaliev H.R., Chernetsova G.S. Pyelonefritis pregnant women. The modern view on the problem of urogynecologic (review). Vestnik KRSU. 2017; 17(7): 33-6.(in Russian)].
- Будник Т.В. Антибиотикорезистентность в контексте инфекции мочевыводящих путей. Семейная медицина. 2015; 4: 77-84. [Budnik T.V. Antibiotic resistance in the context of urinary tract infection. Family medicine. 2015; 4: 77-84. (in Russian)].
- Мальцев С.В., Мансурова Г.Ш. Показатели аутоиммунитета как биомаркеры риска развития и хронизации пиелонефрита. Практическая медицина. 2009; 7: 99-104. [S.V. Maltsev S.V., Mansurova G.Sh. Indicators of autoimmunity as biomarkers of risk of development and chronization of pyelonephritis. Journal of practice medicine. 2009; 7: 99-104. (in Russian)].
- Рищук С.В., Кахиани Е.И., Россолько Д.С., Савина Л.В., Душенкова Т.А., Дудниченко Т.А. Урогенитальная эндогенная бактериальная инфекция и системная энзимотерапия. Медицинский совет. 2016; 17: 124-32. [Rischuk S.V., Kakhiani E.I., Rossolko D.S., Savina L.V., Dushenkova T.A., Dudnichenko T.A. Urogenital endogenous bacterial infection and systematic enzymotherapy. Medical Council. 2016; 17: 124-32. (in Russian)].
- Tublin M.E., Bude R.O., Platt J.F. The resistive index in renal Doppler sonography: where do we stand? AJR Am. J. Roentgenol. 2003; 180(4): 885-92. http://dx.doi.org/10.2214/ajr.180.4.1800885.
Received 10.09.2020
Accepted 15.12.2020
About the Authors
Alexandra M. Khudovekova, graduate student, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology. E-mail: alexandra-ruskhud@yandex.ru.199034, Russia, Saint Petersburg, Mendeleevskaya Line, 3.
Elena V. Mozgovaya, MD, PhD, DSci (Medicine), the Head of Department Obstetricsand and Perinatology. D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology. E-mail:elmozg@mail.ru.
199034, Russia, Saint Petersburg, Mendeleevskaya Line, 3.
Stanislava V. Nagorneva, physician of ultrasound department, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology. E-mail: stanislava_n@bk.ru.
199034, Russia, Saint Petersburg, Mendeleevskaya Line, 3.
Victoria S. Prokhorova, the Head of Ultrasound Department, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology. E-mail: viprokhorova@yandex.ru.
199034, Russia, Saint Petersburg, Mendeleevskaya Line, 3.
Sergey A. Selkov, Dr. Med. Sci., Professor, Head of the Department of Immunology and Intercellular Interactions, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology. Tel.: +7(812)328-98-50. E-mail: selkovsa@mail.ru.
199034, Russia, Saint Petersburg, Mendeleevskaya Line, 3.
Sergey V. Chepanov, PhD, Senior scientist, Proteom Immunoregulation Group, Department of Immunology and Intercellular Interactions, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology. Tel.: +7(812)328-98-50. E-mail: chepanovsv@gmail.com.
199034, Russia, Saint Petersburg, Mendeleevskaya Line, 3.
For citation: Khudovekova A.M., Mozgovaya E.V., Nagorneva S.V., Prokhorova V.S., Selkov S.A., Chepanov S.V. Assessment of effectiveness of treatment in pregnant women with pyelonephritis.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2020; 12: 117-121 (in Russian)
https://dx.doi.org/10.18565/aig.2020.12.117-121