Недостаточность мышц тазового дна – состояние, которое в настоящее время во всем мире имеет тенденцию к увеличению среди пациенток репродуктивного возраста. Позднее обращение за медицинской помощью, отсутствие симптомов при начальных формах заболевания, отсутствие стандартов по диагностике и лечению, а также выжидательная тактика относительно ранних форм приводят к росту заболеваемости пролапсом тазовых органов у пациенток в старшем возрасте [1].
Недостаточность промежности (англ.: deficient perineum) по МКБ-10 классифицируется кодом N81.8 – Другие формы выпадения женских половых органов – и в русскоязычном варианте документа обозначается термином «недостаточность мышц тазового дна» (НМТД). Синонимом можно считать термин «дисфункция тазового дна» (pelvic floor dysfunction), который часто используется и в англоязычной, и в русскоязычной литературе и является собирательным понятием, включающим пролапс тазовых органов (ПТО), недержание мочи (НМ), анальную инконтиненцию, сексуальную дисфункцию и тазовую боль [2].
Некоторые русскоязычные авторы часто пользуются терминами «несостоятельность мышц тазового дна», «синдром несостоятельности тазового дна». Использование термина «несостоятельность», скорее всего, является неправильным, так как толкование этого слова имеет значение «лишенный ocнoвaтeльнocти, yбeдитeльнocти» [Ожегов С.И., 2006], в словаре медицинских терминов отсутствует и не является синонимом слова «недостаточность» (англ.: insufficiency; от лат.: in – не и sufficere – быть достаточным, удовлетворять) – недостаточное функционирование какого-л. органа или его части [Боева Т., 2014].
В обзоре [3] показано, что симптомы НМТД по крайней мере у 40% женщин имеют место уже во время беременности, сохраняясь в течение 6–8 недель послеродового периода у большинства из них. Через 1 год после родов частота НМ и ПТО увеличивается на 7–10%.
По данным Г.Ф. Тотчиева и соавт., симптомокомплекс, определяющий синдром НМТД, включает зияние половой щели, что приводит к нарушению микробиоценоза влагалища у 79% пациенток и развитию доброкачественных заболеваний шейки матки – у 36% [2].
Нарушение микробиоценоза влагалища, или «дисбиоз», в настоящее время рассматривается как изменение количественного и качественного состава, а также свойств локальной микрофлоры [4], и включает не только бактериальный вагиноз (БВ), но и другие неспецифические инфекции – кандидозный вульвовагинит (КВВ), аэробный вагинит (АЭ) и их сочетания, которые наблюдаются у большинства пациенток. Особую актуальность приобретает проблема рецидивирующего течения вагинальных инфекций. Так, в течение первого года после лечения рецидивы БВ возникают у 58% пациенток, у 68% – имеются другие аномальные показатели микрофлоры [5].
Описание клинического наблюдения
Пациентка Б., 33 года, обратилась на прием для осмотра перед планируемой беременностью. Согласие пациентки на обследование, лечение и обработку полученных данных получено. Жалобы предъявляла на дискомфорт во влагалище, иногда – зуд и ощущение сухости, болезненность во время половых контактов. В анамнезе: беременность – 1, завершившаяся нормальными родами через естественные родовые пути 1,5 года назад (вес ребенка при рождении 3650 г, родовых травм и оперативных пособий в родах не было). Соматические заболевания – хронический пиелонефрит, гинекологические – отрицает, в анамнезе – диатермоконизация шейки матки (через один год после родов). Менархе с 13 лет, менструации по 4–6 дней, через 28–30 дней. Половая жизнь с 20 лет; контрацепция – презерватив.
Данные объективного осмотра: рост 162 см, вес 58 кг, ИМТ – 24. Телосложение нормостеническое, кожа и видимые слизистые оболочки нормальной окраски, без высыпаний, со стороны внутренних органов особенностей не выявлено. Фенотипические признаки дисплазии соединительной ткани не выявлены.
Гинекологический статус: наружные половые органы развиты правильно, при визуализации промежности отмечено небольшое зияние половой щели, усиливающееся при пробе Вальсальвы (рисунок), оволосение по женскому типу, слизистая влагалища – обычной окраски, складчатость выражена. Выполнена рН-метрия содержимого влагалища, для чего использовали индикаторные рН-полоски с шагом деления 0,2–0,3–0,5 (чувствительность 90%, специфичность 85%); результат – 6,0.

Вагинальная пальпация для оценки тонуса, тургора и силы сокращений мышц тазового дна (МТД) с оценкой по шкале Оксфорда [6] позволила выявить, что тургор тканей (толщина задней промежности) был нормальным, тонус промежности снижен (при введении во влагалище пальцев исследователя в поперечном положении) – 5 см, сила сокращений по шкале Оксфорда – 2 балла (слабая).
Шейка матки в зеркалах цилиндрической формы, без патологических изменений. При бимануальном исследовании тело матки в правильном положении, не увеличено, подвижно, безболезненно; придатки с обеих сторон не увеличены, подвижны, безболезненны; выделения слизистые с серым оттенком, с запахом.
Для объективной оценки силы сокращений МТД выполнена проба с влагалищными конусами [7] – максимальный вес, удерживаемый путем волевого сокращения МТД в течение 10 минут, составил 20 г. Оценка с помощью цифрового перинеометра iEASE XFT-0010 [8] показала значения 61–65 мм рт. ст. (4 балла – слабое).
При специальном дополнительном опросе выявлены жалобы: «хлюпающие» звуки при половом контакте, недержание мочи при кашле (умеренно), попадание воздуха во влагалище при физических упражнениях, разбрызгивание мочи при мочеиспускании.
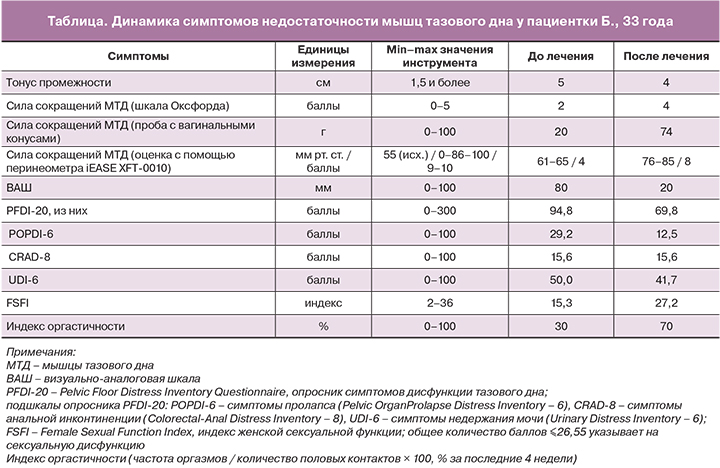
С помощью валидированных опросников выполнена оценка степени дискомфорта/боли (визуально-аналоговая шкала, ВАШ), симптомов дисфункции тазового дна (Pelvic Floor Distress Inventory Questionnaire, PFDI-20), индекса женской сексуальной функции (The Female Sexual Function Index, FSFI) и рассчитан индекс оргастичности [6] (таблица).
В связи с выявлением жалоб на недержание мочи при кашле проведена кашлевая проба, которая в положении на гинекологическом кресле была отрицательной, стоя – слабоположительной. Стрессовый тип НМ был определен на основании оценки симптомов и дневника мочеиспускания (отсутствие поллакиурии, возможность удержать мочу при ургентном позыве, потеря мочи малыми порциями, отсутствие потери мочи в положении лежа, возможность остановить мочеиспускание волевым усилием, наличие слабости мышц тазового дна, частота дневного мочеиспускания 6–8 раз, ночного – отсутствовала, частота эпизодов потери мочи при напряжении – 0–2 в сутки). Комплексное уродинамическое исследование подтвердило диагноз.
Микроскопия мазка влагалищного содержимого показала наличие лейкоцитов в количестве 4–6 в поле зрения, «ключевых» клеток, палочек (G. vaginalis), кокков, дрожжеподобных грибов в небольшом количестве, отсутствие лактобактерий. Обследование на инфекции, передаваемые половым путем (Neisseria gonorrhoeae, Chlamydia trachomatis, Trichomonas vaginalis, Mycoplasma genitalis), методом ПЦР дало отрицательные результаты. По результатам бактериологического исследования отделяемого цервикального канала выявлено наличие условно-патогенной бактериальной флоры (Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum, Gardnerella vaginalis) в концентрации 106 КОЕ/мл и более.
Диагноз: N81.8 Недостаточность мышц тазового дна. Осложненная форма. R39.1 Другие трудности, связанные с мочеиспусканием. N39.3 Непроизвольное (стрессовое) мочеиспускание легкой степени. N88 Другие невоспалительные болезни женских половых органов (бактериальный вагиноз). N94.1 Диспареуния.
На первом этапе лечения была рекомендована санация влагалища комбинированным препаратом, содержащим метронидазол (микронизированный) 750 мг, миконазола нитрат (микронизированный) 200 мг, лидокаин 100 мг и вспомогательное вещество витепсол S55 1436,75 мг (Нео-Пенотран Форте Л). Препарат назначали по 1 суппозиторию во влагалище на ночь в течение 7 дней. Метронидазол и миконазола нитрат входят в рекомендуемые схемы лечения БВ и КВВ соответственно [9, 10].
Контроль результата лечения был выполнен через 14 дней после его окончания, во время которого жалоб пациентка не предъявляла. При объективном осмотре – слизистые оболочки обычного цвета, выделения слизистые в умеренном количестве, без запаха, рН – 4,6. Микроскопия мазка: лейкоциты – единичные, лактобактерии – в умеренном количестве.
После санации влагалища были рекомендованы тренировки МТД (упражнения Кегеля) с применением тренажеров для домашнего использования. Было предложено использовать два вида тренажеров – для статических (вагинальные конусы Yolana/Elanee Phase I весом от 20 до 100 г) и динамических (тренажер Magic Kegel Master) тренировок [7].
Вагинальный конус, смазанный любрикантом, пациентка вводила во влагалище на 10–15 минут ежедневно в утренние часы, 1 раз в день. После того как пациентка могла удерживать самый легкий конус, использовались все более тяжелые. Механизм тренировок заключается в том, что при стоянии или ходьбе конус создает ощущение «выпадения», которое заставляет мышцы тазового дна сокращаться, чтобы его удержать.
Тренажер Magic Kegel Master использовался вечером в режиме «Планирую ребенка» (повышение тонуса мышц тазового дна, подготовка организма к родам и восстановление после них, улучшение кровообращения и работы лимфатической системы).
С пациенткой был установлен контакт с помощью электронных средств связи, поддерживалась мотивация и выполнялся контроль за регулярностью тренировок.
Тренировки МТД выполнялись пациенткой в течение 11 мес до наступления беременности. В связи с наступлением беременности тренировки были завершены в начале II триместра и после родов возобновлены через 8 недель.
Во время беременности, которая протекала физиологически, при плановых микроскопических исследованиях отделяемого женских половых органов в I, II, III триместрах (в соответствии с Приказом МЗ РФ №572н, приложение 5) рецидивов дисбиоза не наблюдалось. Во время беременности имели место эпизоды стрессового недержания мочи (редко). Беременность завершилась срочными родами через естественные родовые пути без осложнений. Вес ребенка при рождении 3800 г, рост 53 см. Послеродовый период протекал без особенностей.
Контроль над состоянием МТД и результатами тренировок был выполнен через 28 месяцев от их начала (общая их продолжительность составила 18 мес). Жалоб не было. За 6 месяцев послеродового периода, по словам пациентки, недержания мочи не наблюдалось, улучшилась сексуальная функция (отсутствие явлений диспареунии, повышение любрикации и частоты оргазма).
Динамика симптомов НМТД, представленная в таблице, была положительной: увеличение силы сокращений мышц тазового дна (с 4 до 8 баллов по показаниям перинеометра) сопровождалось значимым уменьшением частоты и выраженности симптомов недостаточности по опроснику PFDI-20 – на 25 баллов (или на 26%). По мнению M. Wiegersma и соавт., улучшение на 13,5 балла (или снижение на 23%) можно считать клинически значимым. Это минимально важное изменение, по мнению авторов, может быть использовано для оценки эффектов лечения у женщин, состояние которых считается подходящим для консервативного лечения [11]. Наиболее выраженной была динамика по подшкале POPDI-6 (снижение суммы баллов более чем в 2 раза). Частота мочевых симптомов (по подшкале UDI-6) уменьшилась на 20%, из них частота стрессового недержания мочи снизилась с 3 баллов (умеренно) до 1 (нет, но испытывала ранее).
Улучшение клинического состояния пациентки сопровождалось и улучшением сексуальной функции: если до лечения она оценивалась в 15,3 балла по опроснику FSFI, что указывало на сексуальную дисфункцию (≤26,55 балла [12]), то после лечения достигла 27,2 балла, и индекс оргастичности увеличился в 2 раза.
Таким образом, проведенное комплексное лечение позволило снизить частоту и выраженность симптомов дисфункции тазового дна и диспареунии, улучшить сексуальную функцию, предотвратить прогрессирование НМТД и рецидивы дисбиоза влагалища.
Обсуждение
Зияние половой щели – наиболее ранний патогномоничный признак НМТД, встречающийся у 31,4% женщин репродуктивного возраста [3], достигающий 53,1% к 65 годам [13] и наблюдающийся во всех случаях при выявлении начальной формы ПТО. Это состояние сопровождается повышением частоты дисбиоза влагалища в 1,7 раза по сравнению с пациентками без него, что объясняется нарушением первого уровня защиты от распространения экзогенных и эндогенных условно-патогенных микроорганизмов, которым является сомкнутое состояние половой щели [3].
При выборе терапевтической тактики для лечения дисбиоза в условиях недостаточности промежности следует учитывать высокую частоту полимикробных инфекций и их рецидивов, необходимость использования антимикробных средств широкого спектра действия с доказанной эффективностью для эрадикации всех возбудителей и не оказывающих подавляющего влияния на восстановление пула лактобактерий. При этом необходимы средства с коротким курсом лечения и высокой скоростью ликвидации тягостных клинических проявлений, соответствующие современным схемам лечения, указанным в Клинических рекомендациях [9, 10].
Метронидазол входит в международные и российские протоколы лечения. Максимальная эффективность его в лечении БВ составляет 80–90% [14–16]. Это может быть объяснено активностью гидроксильных метаболитов препарата in vivo, которые эффективны в отношении БВ-ассоциированных микроорганизмов. Кроме того, метронидазол изменяет микрофлору влагалища путем эрадикации чувствительных к нему бактерий (анаэробных и некоторых других), что способствует излечению от БВ [17].
Миконазол обладает многогранным фармакологическим действием и активен в отношении широкого спектра грибов, вследствие чего и сегодня остается одним из самых востребованных средств, используемых в терапии КВВ. Миконазол – единственный из всех азолов, обладающий не только фунгистатическим, но и фунгицидным действием. Более того, наряду с некоторыми другими азолами (флуконазол, кетоконазол, клотримазол), миконазол обладает свойством индуцировать продукцию фарнезола чувствительными штаммами Candida spp. Фарнезол представляет собой экстрацеллюлярную молекулу «чувства кворума» (quorum sensing – QS), продуцируемую C. albicans, которая ингибирует образование мицеллярной формы данного патогена – псевдогифов и гифов, которые принимают участие в образования биопленок C. albicans, что является ключевым фактором выживания микроорганизмов. Накопление фарнезола выше порогового уровня препятствует превращению дрожжевой формы в мицелий, заставляя культуру гриба расти, как активно почкующиеся дрожжи, и предотвращает образование биопленок C. albicans, что может являться еще одним механизмом его комплексного антимикотического действия [18].
В исследованиях in vitro показана высокая активность миконазола в отношении грамположительных кокков и бацилл, включая S. aureus и S. epidermidis, Strep. faecalis, С. diphtheria, B. subtilis и Listeria monocytogenes, а также некоторых анаэробных патогенов (Bacteroides fragilis и B. оvatus) [19]. В недавнем исследовании, проведенном P. Nenoff и соавт. (2017), миконазол также демонстрировал высокую активность в отношении различных грамположительных бактерий: минимальная ингибирующая концентрация (МИК) для S. aureus, S. spp., Streptococcus spp. и Enterococcus spp. была в пределах 0,78–6,25 мкм/мл [20].
Содержание метронидазола и миконазола в составе комплексного препарата в повышенных дозах (750 и 200 мг соответственно) позволяет провести эрадикацию возбудителей за короткое время, а добавление лидокаина – достичь максимально быстрого эффекта в отношении тягостных клинических проявлений заболевания (в течение 4–5 минут). Суппозиторная основа витепсол обеспечивает дополнительное увлажнение слизистой оболочки, что наиболее актуально для женщин старшего возраста с явлениями урогенитальной атрофии [21].
Изучение Н.Н. Минаевым и соавт. клинической и микробиологической эффективности препарата метронидазол/миконазол/витепсол (Нео-Пенотран Форте Л) показало устойчивое снижение количества G. vaginalis, A. vaginae и Mobiluncus spp. на протяжении 6 месяцев, при этом нормальный титр лактобактерий наблюдался у 98% пациенток после лечения и сохранялся у 62% к концу наблюдения [22].
Методы консервативного лечения НМТД, включая ПТО на ранних стадиях, в том числе осложненных недержанием мочи и кала, в качестве «первой линии» включают тренировки мышц тазового дна (ТМТД), которые могут быть активными или пассивными. К активным методам тренировки относят выполнение упражнений по методу Кегеля с использованием вагинальных конусов и других вагинальных тренажеров, тренировку в режиме биологической обратной связи (biofeedback), к пассивным – электростимуляцию мышц тазового дна.
В зарубежных публикациях отмечается эффективность ТМТД по критерию уменьшения степени пролапса у 17% пациенток, что было показано в 4 рандомизированных клинических исследованиях, отличающихся высокой степенью доказательности [23]. При этом снижение выраженности симптомов со стороны мочевого пузыря и кишечника достигается у 40–60% пациенток, а отсутствие прогрессирования – более чем у 94%. Эффективность подтверждается также данными УЗ-исследования (увеличение объема мышц, сокращение длины мышц и повышение позиции мочевого пузыря и прямой кишки) [24].
Влагалищные конусы рекомендованы в качестве профилактики пролапса тазовых органов и лечения недержания мочи Международным обществом по удержанию мочи (ICS) [25].
Описана высокая результативность лечения стрессового НМ с помощью электромиостимуляции, в том числе российскими исследователями [26]. Тренажеры, которые применялись в настоящем клиническом наблюдении, также показали высокую эффективность.
Влагалищные конусы могут применяться при слабости мышц тазового дна, недержании мочи при напряжении легкой и средней степени (продолжительностью не более 2 лет), наличии факторов риска пролапса тазовых органов, во время беременности (без осложнений) и после родов (не ранее 6 недель), что полностью отвечало потребностям наблюдаемой пациентки.
Тренажер Magic Kegel Master способствует повышению тонуса мышц тазового дна, улучшению интимных отношений, подготовке организма к родам и восстановлению после них, улучшению кровообращения и работы лимфатической системы, профилактике непроизвольного мочеиспускания. Комбинированное применение тренажеров позволило в короткие сроки добиться положительного результата и предотвратить прогрессирование недостаточности промежности после вторых родов.
Учитывая многообразие современных тренажеров для домашнего использования, важно правильно выбрать наиболее подходящий из них на основе целей предполагаемой терапии, оценки степени выраженности НМТД, наличия/отсутствия пролапса и недержания мочи, а также с учетом противопоказаний [7].
Многочисленные исследования показали, что женщины, которые использовали ТМТД, в 8 раз чаще испытывали улучшение состояния по сравнению с контрольной группой [27].
Технологии, обеспечивающие обратную связь, способствуют лучшему пониманию женщинами, как правильно выполнять упражнения, и позволяют следить за динамикой результатов в процессе тренировок. Метаанализ более чем 100 рандомизированных исследований выявил положительные результаты ТМТД по сравнению с противоречивыми эффектами почти всех других методов лечения [28].
Однако в настоящий момент ТМТД среди российских врачей все еще не являются популярным методом коррекции НМТД. Так, опрос среди 450 акушеров-гинекологов, опубликованный нами в 2017 г., показал, что только 53,7% из них считают ТМТД эффективным методом преодоления расстройств, связанных с НМТД [13]. При этом начало лечения с консервативных методов с целью профилактики ПТО поддержали только 12,9% врачей. Однако и оперативное лечение ПТО на ранних стадиях порекомендовали бы только 7,2%. Очевидно, 80% врачей предпочитают наблюдательную тактику либо затрудняются в выборе метода из-за недостаточной информированности.
Заключение
Комплексное лечение пациентки с НМТД с применением влагалищных конусов Yolana/Elanee Phase I и тренажера Magic Kegel Master в период прегравидарной подготовки позволило снизить частоту и выраженность симптомов стрессового недержания мочи и диспареунии, предотвратить прогрессирование НМТД после родов и рецидивов дисбиоза влагалища, а также улучшить сексуальную функцию.