Lactobacillus – это род неспорообразующих грамположительных палочек, населяющих слизистые ротовой полости, желудочно-кишечного и мочеполового тракта. Представители рода Lactobacillus в составе отделяемого половых путей женщин половозрелого возраста в норме имеют численное преимущество перед остальными бактериями и микроскопическими грибами рода Candida [1]. Лактобациллы влагалища отличаются от лактобацилл желудочно-кишечного тракта как в видовом отношении, так и зависимостью от гормонального уровня. Превалирование молочнокислых бактерий приводит к тому, что рН биотопа находится в пределах 3,8–4,5, что отличает человека от теплокровных животных, у которых молочнокислые бактерии составляют всего 1% нормобиоты. Кислотно-щелочному балансу отводится основная роль в защите женских половых органов от транзиторной микробиоты, в том числе и той, которая попадает с эякулятом [2]. Долгое время считалось, что у всех женщин одинаковый уровень рН во влагалище, пока не было проведено исследование, в котором выяснили, что для африканских и испанских женщин характерен рН выше 4,5. Эти цифры коррелируют с эпидемиологическими данными о более высокой частоте инфицирования их при половом контакте [3].
Нормобиота влагалища и репродуктивных органов женщины
У Lactobacillus spp. имеются адгезины для связывания с фибронектином эпителиальных клеток, что помогает бактериям заселять организм сразу после рождения. Утилизируя гликоген, лактобациллы продуцируют молочную кислоту, рН понижается, а у бактерий повышается способность связывания с фибронектином. Эстрогены, активно образующиеся при половом созревании, способствуют пролиферации клеток эпителия влагалища и продукции внутриклеточного гликогена, а также влияют на плотность рецепторов эпителиальных клеток, связывающихся с лактобациллами [2]. Прогестерон вызывает цитолиз влагалищных эпителиоцитов, и выделяющийся гликоген утилизируется бактериями с образованием молочной кислоты. Таким образом, количество Lactobacillus spp. увеличивается, и они начинают преобладать над остальными микроорганизмами [1]. Другие бактерии, такие как Atopobium, Megasphaera и Leptotrichia, также могут способствовать снижению рН при ферментации глюкозы. Помимо бактерий, молочная кислота продуцируется клетками вагинального эпителия под контролем эстрогенов [4].
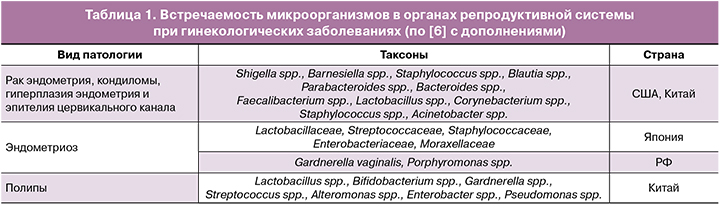
Доказано большое разнообразие бактерий, населяющих репродуктивные органы в норме и при патологии [5]. Поиск микроорганизмов, встречающихся в матке при различных гинекологических заболеваниях, проводился во многих странах (табл. 1).
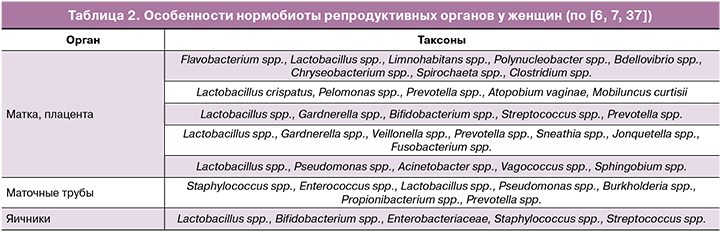
Обнаружено большое разнообразие микробиоты эндометрия, что позволило выделить две группы женщин, в том числе с нормально протекающей беременностью: с доминированием лактобацилл и других родов, когда Lactobacillus spp. составляют менее 90% всех бактерий. Особенности микробиоты генитального тракта и плаценты представлены в таблице 2.
Все проведенные исследования объединяет небольшая выборка по сравнению с работами по исследованию микробиоты влагалища.
При более подробном изучении бактерий влагалища выяснилось, что Lactobacillus spp. – не единственные его резидентные представители. Обнаружено более 250 видов бактерий из нескольких десятков родов [8]. В период фертильности чаще других Lactobacillus spp. встречаются в ассоциации с Bifidobacterium spp. [1], а в пременопаузе – с другими анаэробными бактериями родов Prevotella, Dialister, Atopobium, Gardnerella и Megasphaera [9]. Среди представителей рода Lactobacillus описано более 120 видов. Обычно у женщины доминирующим является один, реже два вида, среди которых наиболее часто встречаются L. crispatus, L. gasseri, L. jensenii и L. iners [8, 10].
Роль лактобацилл
Роль лактобацилл многообразна. Для выживания в аэробных условиях они образуют перекись водорода, которая обладает ингибирующим влиянием на другие резидентные бактерии и вирусы. Бактерии рода Lactobacillus, продуцируя лектины и стимулируя иммунную систему, играют важную роль в колонизационной резистентности. Некоторые из них продуцируют бактериоцины, биосурфактанты и коаггрегирующие молекулы для ингибиции адгезии патогенов [2]. Так, бактериоцинпозитивные штаммы L. acidophilus и L. rhamnosus, выделенные у детей раннего возраста, проявили выраженную антагонистическую активность в отношении бактериальных клеток Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, Enterococcus faecalis и Clostridium perfringens. Антагонистическая активность бактерий L. paracasei, как и L. plantarum ST23LD и ST341LD, продуцирующих бактериоцин B-217 и плантарицины, соответственно проявлялась в отношении S. aureus, Streptococcus pneumoniae, Enterococcus faecalis, E. coli, Bacillus cereus, Salmonella spp., Pseudomonas aeruginosa. Плантарицин низкой молекулярной массы (1558 Да), синтезируемый бактериями L. plantarum Lp31, был активен в отношении тест-культур Listeria monocytogenes, S. aureus, B. cereus и Pseudomonas spp. L. fermentum в опыте препятствовала колонизации 108 КОЕ E. coli. У L. helveticus HY7801 отмечена наибольшая способность к ингибиции грибов рода Candida, как in vivo, так и в культуре клеток HeLa [4, 11].
Большое значение имеет опосредованное действие лактобацилл на физиологические функции организма, в том числе на фертильность и течение беременности. Например, бактероиды, фузобактерии, а также анаэробные стрептококки и гарднереллы продуцируют фосфолипазу А2, которая активирует продукцию простагландинов. У беременных женщин бактериальные протеазы и липазы могут воздействовать на хориоамниотическую мембрану, приводя к ее разрыву и инициации преждевременных родов [2]. Ингибируя рост указанных бактерий и предотвращая продукцию ими перечисленных ферментов и метаболитов, лактобациллы способствуют физиологическому течению беременности. Положительный эффект лактобацилл доказан для успешного экстракорпорального оплодотворения. Но в этом вопросе данные противоречивы, и не всегда авторами учитываются сопутствующие факторы, такие как возраст, гормональный фон, эндокринная патология [12].
Данные по изучению антагонистической активности лактобацилл in vitro иногда расходятся с экспериментальными данными in vivo. Например, при изучении влияния лактобацилл на уровень колонизации влагалища стрептококком группы В (СГВ) в одном исследовании эффекта от приема пробиотического штамма не обнаружили, и у женщин, принимающих плацебо, был такой же уровень СГВ, как и у принимающих пробиотик в течение 3–4 недель [13]. В то же время у 30% женщин, принимающих пробиотический штамм RC-14/GR-1 перорально в течение 14 дней, отмечена обратная связь между возрастанием концентрации лактобацилл и уменьшением численности СГВ. Но назначение того же препарата в виде тампонов успеха не имело [14]. Это еще раз показывает, что нельзя рассматривать бактерии «по отдельности», без учета их естественных мест обитания. Так, биотопом для СГВ является прямая кишка, поэтому пероральное назначение пробиотиков в течение длительного времени представляется более целесообразным.
Интересны данные по изучению колонизационной резистентности лактобацилл по отношению к патогенным бактериям. L. crispatus может обладать защитным эффектом в отношении гонококков и хламидий. И наоборот, в отсутствие лактобацилл диагностируются инфекции, вызванные Chlamydia trachomatis, Mycoplasma genitalium и Neisseria gonorrhoeae [15].
На рисунке представлены данные, полученные при анализе более 20 000 образцов биоматериала жительниц Санкт-Петербурга, обратившихся к гинекологу при вагинитах. Обратная корреляция между наличием патогенных микроорганизмов и лактобацилл доказывала их способность обеспечивать колонизационную резистентность, препятствуя размножению многих условно-патогенных и патогенных микроорганизмов. Важное значение имеет видовая специфичность Lactobacillus spp. L. casei, L. delbrueckii, L. fermentum, L. rhamnosus никогда не сочетались с патогенными бактериями; в то время как L. crispatus и L. jensenii встречались вместе с возбудителями инфекций, передающихся половым путем (ИППП) [10].
Долгое время нормобиотой влагалища считались четыре вида лактобацилл – L. crispatus, L. jensenii, L. gasseri и L. iners, к которым позже добавили G. vaginalis [16, 17]. На сегодняшний день описано пять вариантов микробиоты здоровой половозрелой женщины. Доминирующие виды лактобацилл при разных типах влагалищной микробиоты и их роль представлены в таблице 3.

Дисбиоз: причины и последствия
Женская вагинальная микробиота пластична, подвержена циклическим изменениям и может оказывать как физиологический, так и патологический эффект. Увеличение количества L. iners может быть сигналом к началу вагиноза; такая женщина более подвержена риску заражения хламидиозом. У самой L. iners описаны факторы вирулентности, такие как инеролизин, холестеринзависимый цитолизин – энзим, формирующий поры в клетках эпителия, активность которого была повышена у шестой части женщин с вагинозом. Бактериальный вагиноз, ассоциированный с IV типом, встречается у 12% женщин в Австралии и в странах Африки [15, 19]. Слишком большое количество лактобацилл или удлиненные лактобациллы с атипичной морфологией могут вызвать зуд и дизурию. Такой «цитолитический вагиноз», или «лактобациллез», напоминает по клиническим проявлениям кандидоз и требует проведения дифференциальной диагностики [8].
В 1955 г. H. Gardner и C. Dukes открыли Haemophilus vaginalis, позже переименованную в G. vaginalis, а состояние, которое она вызывает, было названо бактериальным вагинозом. Оно проявляется увеличением содержания в урогенитальном тракте женщин G. vaginalis и представителей родов Atopobium spp., Megasphaera spp., Anaerococcus, Peptoniphilus, Prevotella, а также L. iners, микоплазм и уреаплазм [15].
Бактериальный вагиноз – самая часто встречающаяся патология у женщин (19–24%) на сегодняшний день, в том числе он диагностируется у пятой части беременных. [12]. В то же время около 20% беременных женщин в Германии и половина небеременных женщин с микроскопической картиной бактериального вагиноза не имеют жалоб и клинических проявлений [8], хотя риски развития осложнений не зависят от клинической картины вагиноза.
В качестве одной из причин размножения условно-патогенной микробиоты рассматривают снижение количества лактобацилл из-за вирулентных фагов [1]. На фоне снижения количества лактобацилл размножение Gardnerella, Atopobium, Eggerthella, Leptotrichia/Sneathia и Prevotella приводит к развитию бактериального вагиноза и цервицита [21]. Неблагоприятными периодами в плане снижения количества облигатной бактериальной микробиоты является препубертатный и постменопаузальный возраст. В эти периоды снижается количество гликогена, ухудшается рецепция лактобактерий к влагалищному эпителию, значение рН становится нейтральным, что приводит к преобладанию облигатных анаэробов. Вероятным пусковым механизмом этого может быть низкий уровень эстрогенов [1]. В менопаузе количество вырабатываемого эстрогена снижается, что приводит к развитию патологических изменений в эпителии влагалища в виде атрофии. У таких женщин часто имеется колонизация энтерококком; в 50% встречается A. vaginae, а также Prevotella, Porphyromonas, Peptoniphilus, Bacillus. Иногда чувствительность микроскопического метода с окраской по Граму может оказаться недостаточной, и микроорганизмы не визуализируются [9, 18]. Вредные привычки, например, курение, также способствуют развитию вагиноза. Peptostreptococcus и Veillonella достоверно чаще встречаются у курящих [19]; у 28% отмечен высокий уровень гарднерелл и/или A. vaginae [16]. У 5% некурящих и 40% курящих женщин выявлены маркеры дисбиоза при окраске мазков по Граму [18, 22].
Преждевременные роды являются распространенной акушерской патологией. Они случаются в 5–9% случаев беременности в Европе и в 13% в США. Риск преждевременных родов при дисбиозе в два раза выше, чем у женщин с нормобиотой. Кроме того, женщины имеют более высокий риск прерывания первой беременности во II триместре, когда влагалищная микробиота содержит небольшое количество лактобацилл, или они вообще отсутствуют при микроскопии мазков [12]. Лечение антимикробными препаратами, несмотря на исчезновение клинических симптомов, не предотвращает преждевременные роды [13, 23]. Совершенно противоположные данные были получены в другом исследовании: прием клиндамицина беременными женщинами с дисбиозом, выявленным до 16–20 недель беременности, на 80% сократил количество преждевременных родов [20]. У женщин с трубной беременностью и другими нарушениями беременности достоверно чаще встречаются бактерии, ассоциированные с вагинозом [24]. Вагиноз напрямую коррелирует с высоким уровнем инфицированности вирусами папилломы человека (ВПЧ), в том числе и с высоким онкогенным риском ВПЧ-16 и ВПЧ-18 [19]. Женщины из Южной Африки в большей степени подвержены заражению ВИЧ, что связывают с особенностями нормобиоты и более высоким уровнем распространения бактериального вагиноза [3, 25].
Коррекция дисбиоза
Для лечения бактериального вагиноза традиционно используют антимикробную терапию. Но прием метронидазола и клиндамицина может сопровождаться побочными эффектами, к которым относится и дисбиоз. К тому же после лечения метронидазолом часто наблюдают рецидивы: у 30% женщин симптомы возвращаются через 3 месяца, а у 60% – через полгода после окончания терапии [8]. У 76% повторнолеченных женщин терапия оказывается неэффективной из-за резистентности бактерий. В качестве альтернативы предложено лечение фагами [26, 27].
Так как лактобациллы проявляют зависимость от эстрогенов, то одним из способов лечения дисбиоза является заместительная гормональная терапия [9, 19, 28]. Однако самым перспективным является назначение пробиотиков: микробиоту удалось восстановить в течение 5 дней с помощью L. acidophilus GLA-14 и L. rhamnosus HN001, комбинированными с лактоферрином в качестве адъюванта [29]. В состав пробиотиков добавляют штаммы Streptococcus thermophilus, Propionibacterium acidilactici LN23. Прием пробиотика, состоящего из одного-двух видов лактобацилл, может оказаться более эффективным [22, 27, 30, 31]. Большое влияние на выводы научной работы оказывает организация процесса. Так, в одном из исследований при оральном назначении L. rhamnosus GR-1 и L. reuteri RC-14 в течение 60 дней был отмечен положительный эффект, но так как женщины принимали препарат без контроля, а опрос проводился по телефону, то нормализация микробиоты всего у 14% женщин вызывает сомнение [23]. Перспективным направлением является комбинация пробиотического штамма с гормонами. Совместное применение эстрогена в дозе 0,03 мг с L. acidophilus оказалось достаточно эффективным: исследование с применением плацебо и комбинированного препарата показало, что через 6 месяцев восстановился состав микробиоты до уровня пременопаузы [9].
Новым направлением в лечении дисбиоза является пересадка влагалищных бактерий от здорового донора женщинам с рецидивирующим вагинозом. У четырех из пяти женщин отмечено стойкое улучшение в течение 5–21 месяцев наблюдения, что подтверждалось отсутствием жалоб, клинических проявлений и критериями Amsel. Однако ремиссия у трех пациентов потребовала повторной пересадки микробиоты и смены донора [32]. Возможно, что перед трансплантацией микробиоты надо не только убедиться в безопасности метода как в инфекционном, так и в иммунологическом отношении, но и подобрать донора с генетически близкими лактобациллами. Можно использовать микробиоту самой женщины, но есть риск, что в случае качественного нарушения лактобацилл они окажутся неэффективными после пересадки, ведь количественное преобладание не гарантирует выполнения всех функций нормобиоты. Идея трансплантации микробиоты не нова и пришла в гинекологию из гастроэнтерологии. Реализовать пересадку возможно двумя путями: культивирование донорских бактерий на питательных средах или непосредственная пересадка влагалищного секрета после центрифугирования [33]. Вариант с предварительным накоплением представляется более безопасным в плане передачи инфекционных агентов, таких как ВПЧ или ВИЧ; бактерии можно хранить длительное время и повторять трансплантацию при необходимости.
Появляется возможность создания банков образцов из кишечника и влагалища для использования в качестве материала для гомологичных и аутологичных трансплантаций и выделения штаммов аутопробиотиков. Также возможны подбор пробиотиков c учетом антибактериальной и/или антивирусной активности, иммуномодулирующего эффекта, адгезивности к влагалищному эпителию, создание аутопробиотиков на основе таких облигатных представителей микробиоты влагалища, как L. reuteri, L. rhamnosus и L. acidophilus для персонифицированной терапии вагинитов и коррекции дисбиотических состояний. Несмотря на огромное количество научных публикаций, посвященных использованию пробиотиков в акушерской и гинекологической практике, результаты этих работ противоречивы, часто встречаются повторы одного и того же исследования. Начиная с 1992 г., опубликованы результаты не более 100 оригинальных исследований, хотя количество публикаций составляет несколько тысяч. И даже эти исследования, проведенные по всем правилам, противоречат друг другу. Это объясняется различиями, связанными с используемыми пробиотическими штаммами и с длительностью и способом их приема.
Не получено достоверных данных, что монотерапия пробиотиками более эффективна, чем антибиотиками или гормонами, или что комбинация пробиотика с антибиотиком или гормоном более эффективна, чем традиционное лечение [27, 34, 35]. Восстановление количества лактобацилл должно проводиться комплексно, с учетом микроэкологии влагалища [36], типа микробиоты, которые отличаются у женщин разного возраста и рас, степени нарушения гомеостаза. Очевидно, что пробиотики должны назначаться только по показаниям после комплексного обследования, включающего применение современных методов микробиологии.
Заключение
Классический микроскопический метод не может определить принадлежность женщины к одному из пяти типов по влагалищной микробиоте. Он не позволяет исключить ошибки в идентификации бактерий: так, L. iners и G. vaginalis морфологически очень похожи. В этой области требуются дополнительные исследования для разработки персонифицированной терапии.