The fallopian tubes in genital pathology and intratubal therapy for female infertility
Objective. To conduct a retrospective, comparative study of the morphological state of the fallopian tubes.Brodsky G.V., Adamyan L.V., Sukhikh G.T.
Subjects and methods. Histological, immunohistochemical and morphometric examinations were used to examine the histological specimens of the fallopian tubes in 714 reproductive-aged women. Among them, there were 127 women diagnosed with nonspecific cervical inflammatory processes, 122 with uterine fibroids, 177 with genital endometriosis and uterine adenomyosis, and 223 women with benign ovarian cysts. The fallopian tube specimens from 65 women without genital pathology served as a control.
Results. The findings were analyzed taking into account the assessment of structural elements in different parts of the fallopian tube, the thickness of its wall layers, the characteristics of arterial and venous blood supply and microarchitecture of the fallopian tube wall in different phases of the ovarian and menstrual cycle in concomitant extratubal pathology of the genital tract. The findings were compared with the histological and morphometric data of the control group, without indicating concomitant genital pathology in the clinical protocol.
Conclusion. The finding may lead to the conclusion that the observed changes in the fallopian tube wall in various types of genital tract pathology play an important role as a morphological substrate for the clinical data related to the low efficiency of assisted reproductive technologies. This study makes it possible to clarify a diagnostic algorithm and to introduce a novel method for the treatment of patients in a female infertility clinic.
Keywords
One of the actual problems in modern gynecology practice is tubal infertility and restoration of anatomical and functional patency of the fallopian tubes [1-5]. One of the reasons reducing the treatment efficiency is pathology of the uterus and appendages [1-3]. Its influence on the state of the fallopian tubes arouses interest in connection with performing organ-preserving operations, reproductive technologies and functional recovery treatment.
Among the existing lifetime assessment and treatment methods of the fallopian tubes patency, hysterosalpingography (HSG), contrast enhanced HSG, chromopertubation, hydrotubation and pneumotubation of the fallopian tubes, also salpingoscopy and microsalpingoscopy should be noted.[5-8].
The disadvantage of all above-mentioned diagnostic methods is the impossibility of assessing the functional state of the fallopian tubes and lack of information on correlation with the accompanying genital tract pathology.
The most informative and invasive of the lifetime methods of diagnosting the state of the fallopian tubes ismicrosalpingoscopy (transcervical or transabdominal in the mode of hydroperitoneum, chromosalpingoscopy and hysteroscopy); however, it does not allow to assess the condition of the mucous membrane, muscular layers, peculiarities of vasculature, nerve suupply and lymphatic system of the fallopian tube wall. Each of them performs a special function composing anatomic and functional integrity of the fallopian tube. Microsalpingoscopy as a part of fertiloscopy allows to define only patency of the fallopian tubes or to restore patency of the fallopian tube without determiningits functional ability. Dysfunction of the fallopian tube is indirectly demonstrated by the excessive staining of the mucous layer with methylene blue in carrying outchromopertubation of the fallopian tube.
The aim of this investigation is to develop and introduce in clinical practice less traumatic methods of diagnosing and treating the fallopian tubes with non tubal associated genital pathology cases using the revealed morphological regularities of macro-and microchanges in the fallopian tube wall.
Material and Methods
Morphological part of the research was carried out retrospectively to compare histological archival material of the fallopian tubes from 714 women of reproductive age (25–40 years) whose uterus and uterine appendages suspected to have benign pathologyof the genital tract were removed. According to surgical protocols, 127 women had nonspecific inflammatory processes of the cervix uteri, uterus myoma was diagnosed in 122 cases, external genital endometriosis and adenomyosis uteri were found in 177 cases, 223 cases had benign cysts of ovaries. The samples of the fallopian tubes obtained from 65 women without the genital tract pathology were taken during tubal sterilization and removal of the part of the uterine tube. They composed the control group. For studying microtopography and macro-microscopic anatomy of the fallopian tube, the serial hystotopograms stained by hematoxylin-eosin and by van Gison methods were used.
There was hystotopography investigation of the following sites of the fallopian tube: the middle of the ampullary, the site between the ampullar and isthmus, the middle of the isthmus, the junction zone of the fallopian tube and uterus and the uterine part of the fallpian tube.
The quantitative assessment of the lumen, wall, various parts of the fallopian tube, its coats and layers, and blood vessels was carried out. Calculations of distances, perimeters and areas were performed using the computerized morphometric MAGICSCAN system.
On the basis of the revealed regularities, we estimated the condition of the mucous membrane, the muscular layer (namely, its circular and longitudinal muscular layer), the arterial and venous micro-architecture, the lymphatic tissues and nerve supply of the fallopian tube wall. Each factor was estimated on three-point system. The maximum score from 7 to 9 corresponded to severe degree of the functional disorder of the fallopian tube, the sum of 4-6 points referred to the middle degree and the sum of 0-3 points corresponded to the light degree of the functional disorder of the fallopian tube.
Results and Discussion
The morphometric research has allowed to reveal the changes in thickness of the fallopian tube wall, its coats and layers, and blood vessels in some non-tubal pathologies of the genital tract (Fig. 1).
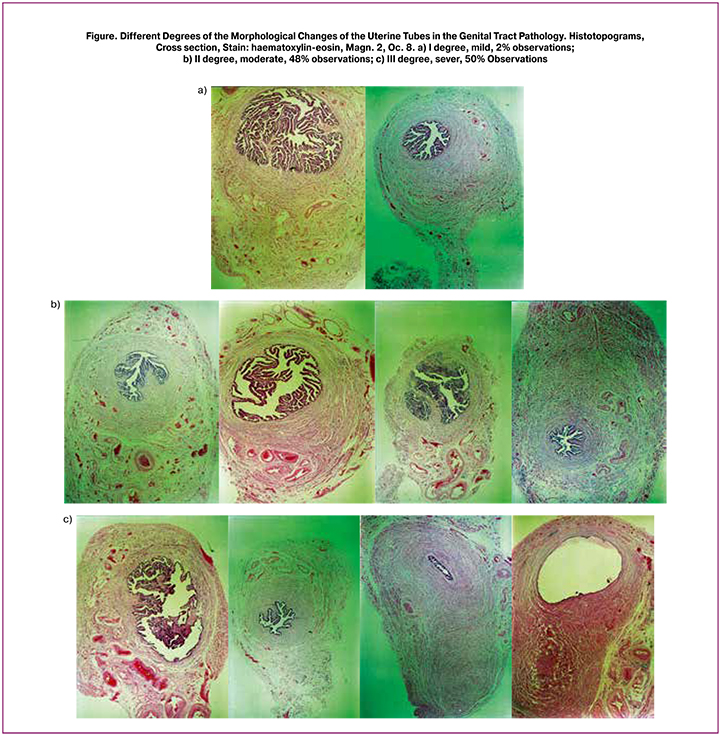
Thus, it has been revealed that nonspecific inflammatory changes of the uterine cervix are associated with the primary change of superficial epithelium of the mucous membrane, its desquamation. Adenomyosis uteri is associated with the changes characteristic of chronic inflammatory process of the fallopian tube, atrophic changes of the mucous membrane of the fallopian tube which are manifested in reduced quantity of primary, secondary and tertiary fimbriae, reduced quantity of folds and smoothing relief of the mucous membrane of the fallopian tube. In uterine myoma with interstitial localization of nodes, predominantly change of the muscular layer of the fallopian tube wall, both the longitudinal and circular, has been determined. It is connected with disintegration of the muscle fibres in combination with the changes in hemodynamic and microcirculation of the fallopian tube wall playing an important role in propulsive and transport function of the fallopian tube.
There has been a redistribution of the arterial blood supply of the fallopian tube from a subtubal vascular bunch with concentration of the small arteries and capillaries mainly on the anterior and posterior walls to the loose small arterial vessels and capillaries on the anterior, posterior and superior walls of the fallopian tube, along with reduction of intensity of the subtubal vascular bunch and its sizes. The processes of neoangiogenesis and formation of the collateral blood supply system in the uterine tube wall have been noted. Along with this, the vasodilatation of vessels of the venous system testifying venous stasis in the fallopian tube wall has been revealed.
The reduction of a number of nerve endings in the fallopian tube wall and randomness of their distribution in its limits have been noted. The changes in the fallopian tube wall in the presence of the benign ovarian cyst primarily are connected with the mechanical pressure on structures of the fallopian tube wall and are characterized by the changes of congestive character of the venous system of the fallopian tube and the lymphatic system of the fallopian tube wall.
The special subgroup should include the long-term benign tumour of the ovary and mesosalpinx (teratoma), making mechanical pressure on the fallopian tube wall and causing changes similar to the changes in uterine myoma with interstitial localization of node.
The combination of hysteroscopy and fertiloscopy as two minimally invasive, high-informative methods of diagnosing patency of the fallopian tubes and its correction, provide a direct access to the fallopian tube and also a complex of diagnostic and medical procedures in clinic of female infertility [5–8].
The disadvantage of above-mentioned methods of diagnostics and treatment is the difficulty in assessment of the functional condition of the fallopian tubes and performing the adequate treatment in the presence of anatomic integrity and absence of any occlusions in the fallopian tube.
The revealed morphological regularities have allowed to develop a new “diagnostic method of the condition of the fallopian tubes in uterine myoma, uterine adenomyosis, benign ovarian tumours, non-specific inflammatory processes of the cervix uteri “ (the Patent of the Russian Federation No. 2437615) [9] and also “The methods of medical treatment of the fallopian tubes in tubal and idiopathic forms of female infertility”. It involves inserting a thin (1 mm in the diameter) irrigational catheter into the uterine part of the fallopian tube on the whole length of the uterine tubethrough an instrumental opening of the hysteroscope, under optical control. It allows to carry out the local medication therapy aimed at restoring anatomic and functional integrity of the fallopian tubes and reproductive function of women without using artificial reproductive technologies (the Patent of the Russian Federation No. 2442545) [10]. The performed differentiated intra-tubal therapy according to the type of the revealed genital pathology has allowed achieving spontaneous pregnancy and birth in 64% of cases in women who denied using artificial reproductive technologies.
Conclusion
Our research allows conducting the comparative analysis of morphological changes of the fallopian tubes in reproductive-aged women having non-tubal genital pathology.
The method of the indirect assessment of the fallopian tubes state in some genital pathologies, such as uterine myoma, adenomyosis, benign ovarian tumours, non-specific inflammatory processes of the cervix uteri allows to perform noninvasive evaluation of the functional state of the fallopian tubes in the above-mentioned genital pathologies which cause female infertility. The offered method of medical treatment of the fallopian tubes in tubal and idiopathic forms of female infertility allows carrying out intratubal therapy in the clinic of female infertility.
The conclusions drawn from the research are the most important for assessingthe state of the fallopian tubes in patients with tubal and idiopathic forms of infertility. Practical application of our research can be recommended in performing operations on reconstruction of anatomical and functional activity of the fallopian tubes and artificial reproductive technologies. These recommendations are of greater importance for the patients who cannot achieve desired pregnancy after the surgical intervention or artificial reproductive technologies and who in their case history have indicators of non-tubal genital pathology which cause tubal infertility.
The participation of the fallopian tube in the processes of fertilization and transportation of the fertilised ovum into the uterine cavity allows to consider the changes in micro-architecture and vasculature of the fallopian tube wall in non-tubal genital pathology as the morphological substrate explaining increase in frequency of tubal pregnancy and low efficiency of uterine pregnancy in performing reconstructive plastic surgeries or transferring gametes or zygotes into the lumen of the fallopian tubes in the IVF procedure. Our research allows to define the algorithm of making diagnosis and to introduce a new method of treatment of patients with the functional form of tubal infertility and the accompanying pathology of the genital tract.
References
- Adamyan L.V., Bragina E.E., Arslanyan K.N., Kharchenko E.I. Possibilities of electron microscopy in assessing the state of fallopian tubes in infertility. In: Adamyan L.V., ed. Modern technologies in the diagnosis and treatment of gynecological diseases. Guideline. Moscow: FGU NC AGIP of Rosmedtechnologies; 2007: 133-4. (in Russian)
- Bezhenar V.F., Maksimov A.S. Pipe-peritoneal infertility. Problems and prospects. Zhurnal akusherstva i zhenskikh bolezney. 1999; 48(3): 48-55. (in Russian)
- Krasnopolskaya K.V., Shtyrov S.V., Bugerenko A.E., Chechenova F.K. Surgical treatment of tubal infertility. Literature review. Problem reproduktsii. 2000; 6(4): 31-5. (in Russian)
- Kulakov V.I., Selezneva N.D., Krasnopolsky V.I. Operative gynecology. Guideline. Kulakov V.I., ed. Moscow: Meditsina; 1990. 464p. (in Russian)
- Brodsky G.V., Adamyan L.V. Intralumenal treatment of uterine tubes in tubal and idiopathic form of female infertility with using minimal invasive technique. Geburtshilfe Frauenheilkd. 2014; 74 (Suppl. 1): PO_Endo01_10.
- Watrelot A., Gordts S., Andine J.P., Brosens I. Une nouvelle approche diagnostique. La Fertiloscopie Endomag. 1997; 21: 7-8.
- Watrelot A., Dreyfus J.M., Cohen M. Systematic salpingoscopy and microsalpingoscopy during fertiloscopy. J. Am. Assoc. Gynaecol. Laparosc. 2002; 9(4): 453-9.
- Watrelot A., Nisolle M., Chelli H., Hocke C., Rongières C., Racinet C. International Group for Fertiloscopy Evaluation. Is the lapascopy still thegood standard in infertility assessment? A comparision of fertiloscopy versus laparoscopy in infertility: Results of an international multicentre prospective trial: The “FLY” (Fertiloscopy-LaparoscopY) study. Hum. Reprod. 2003; 18(4): 834-9.
- Patent for invention № 2437615, Russia. Brodsky G.V., Adamyan L.V., Sukhikh G.T. A method for diagnosing the state of fallopian tubes in uterine myomas, benign ovarian tumors, nonspecific inflammatory processes of the cervix. Reported on September 20, 2010, published on the 27.12.2011. Bulletin of Inventions. 2011; No. 3. (in Russian)
- Patent for invention № 2442545, Russia. Brodsky G.V., Adamyan L.V., Sukhikh G.T. The method of treatment of female infertility of tubal etiology. Reported on September 20, 2010, published on February 20, 2012. Bulletin of Inventions. 2012; №5. (in Russian)
Received 16.01.2018
Accepted 02.03.2018
About the Authors
Brodsky, Gregory V., MD, Specialist Obstetrics and Gynaecology, Head of Practice – Clinic for Gynaecology and Obstetrics, Munich, Germany.80807, Germany Munich, Oberhofer Platz 4. E-mail: 150665@gmx.net
Adamyan, Leila V., MD, professor, academician of RAS; deputy director on science, head of department of operative gynecology, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4
Sukhikh, Gennady T., MD, PhD, Professor, Academician of Russian Academy of Sciences, Director of National Medical Research Center of Obstetrics,
Gynecology and Perinatology, Ministry of Health of Russia. 117997, Russia Moscow, Ac. Oparina str. 4. Tel.: +74954381800. E-mail: gtsukhikh@mail.ru
For citations: Brodsky G.V., Adamyan L.V., Sukhikh G.T. The fallopian tubes in genital pathology and intratubal therapy for female infertility. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (9): 74-8. (in Russian)
https://dx.doi.org/10.18565/aig.2018.9.74-78