Magnetic resonance imaging in the diagnosis of brain abnormalities in patients with severe preeclampsia
Objective. To investigate the prospect of using brain MRI to improve the accuracy of the brain lesions diagnosis in patients with preeclampsia.Shalina R.I., Kurtser M.A., Simukhina M.A., Latyshkevich O.A., Lebedev E.V., Shtabnitskii A.M., Platitsyn I.V.
Material and methods. This retrospective study comprised 36 pregnant and puerperal women with severe preeclampsia who underwent brain MRI.
Results. A total of 47.2% of patients, who had PE with neurological manifestations were found to have MRI-detected brain abnormalities; 88% of them, including PRES (13.9%), stroke (5.6%), and vascular lesions (22.2%) were associated with arterial hypertension. In 66.7% of patients, preeclampsia was atypical.
Conclusion. Using brain MRI in patients with PE who have neurological manifestations results in more accurate assessment of its severity, timely delivery, and appropriate therapy, which may contribute to a reduction in the incidence of severe PE complications, in particular in the incidence of a cerebral hemorrhage.
Keywords
Over the past five years, there has been a 6-fold global increase in the number of brain hemorrhages in patients with hypertensive disorders of pregnancy [1]. When evaluating patients with preeclampsia (PE), physicians are mainly focused on hypertension (AH) and proteinuria as the two main symptoms of PE, while neurological manifestations are often underestimated, and this can lead to serious complications [2]. The consequences of severe PE and eclampsia (E) may extend beyond the early postpartum period and predispose a patient to complications later in life manifesting in an increased risk of cardiovascular and cerebrovascular diseases, renal complications, vision impairment, diabetes mellitus, and memory loss [3]. These facts once again emphasize the need for additional diagnostic modalities that are as objective as possible in detecting both changes in the central nervous system and the severity of PE.
A headache and visual impairment are the most frequent complaints associated with lesions of the central nervous system (CNS) in PE. Patients with these symptoms have a high risk of such serious complications as eclampsia, stroke, cortical blindness, retinal detachment, transient ischemic attack (TIA), and coma. A definite diagnosis of the cause of these conditions is often difficult. In such situations, magnetic resonance imaging (MRI) can be used for diagnostic imaging of the brain. The indications for MRI in patients with PE are not clearly defined, and it is mainly used in patients who develop a coma, signs of impaired cerebral circulation, and changes in the level of consciousness (stupor, coma).
This study aimed to evaluate the prospect of using brain magnetic resonance imaging to improve the accuracy of diagnos
Material and methods
This retrospective study comprised 36 patients with severe PE who underwent brain MRI at the Family Planning and Reproduction Center of the Moscow Health Department. Brain MRI was performed during pregnancy (n = 16) and in the early postpartum period (n = 20). Pregnant and puerperal women with PE and headache complaints were included in the study. The diagnosis of PE was made based on the main criteria of the disease (AH and proteinuria) according to current clinical guidelines for hypertensive disorders of pregnancy. Moderate PE was diagnosed if systolic blood pressure (SBP) was 140-159 and/or diastolic blood pressure (DBP) 90- 109 mm Hg; severe PE was diagnosed in patients with SBP ≥ 160 and/or DBP ≥ 110 mm Hg.
Moderate proteinuria corresponds to a 24-hour urinary protein >0.3 g or> 0.3 g/l in two urine samples taken at 6-hour intervals; massive proteinuria corresponds to a 24-hour urinary protein ≥ 5 g or> 3 g/l or> 0.3 g/l in two urine samples taken at 6-hour intervals. Additional diagnostic criteria for PE were thrombocytopenia, elevated liver transaminases, edema, etc. The exclusion criterion was the history of previous MRI-confirmed organic brain lesions.
Diagnostic evaluation included age, medical history (blood pressure before pregnancy, acute and chronic cardiovascular diseases, disorders of kidney, liver, blood, central nervous system, head injury), parity, obstetric and gynecologic history (pelvic organ diseases, the course of previous pregnancies and childbirth), complications and weight gain during current pregnancy. Assessment at hospital admission included gestational age, complaints, general physical examination, blood pressure measurement, and testing for proteinuria, presence and severity of edema, changes in the findings of laboratory tests (CBC, urinalysis, blood biochemistry, blood coagulation evaluation), ultrasound (fetometry, Doppler), indications for brain MRI.
The brain scans were performed with a Siemens Magnetom 1.5 T high-field MRI scanner using FLAIR, DWI, Hemo, T1, and T2 modes. MRI sequence parameters are given in table 1.

Statistical analysis was performed with SPSS Version 24.0 statistics software for Mac OS (SPSS inc., USA). The differences in frequencies of the explored parameters were considered statistically significant at p <0.05.
Results and discussion
The patients’ age ranged from 23 to 46 years. More than a third (n = 14, 38.9%) were over 35 years; the age of 12 (33.3%) and 10 (27.8%) patients was 30–35 and 23–29 years, respectively.
There were twice fewer multiparous (n = 12, 33.3%) than primiparous women (n = 24, 66.7%); almost half of multiparous patients (n = 5, 41.7%) had a history of PE during previous pregnancy.
Every second study participant had a complicated medical history, including lipid metabolism disorders (LMD) (n = 7, 19.4%), arterial hypertension (AH) (n = 6, 16.6%), urinary diseases (chronic cystitis and pyelonephritis) (n = 6, 16.6%), which is twice more common than in the general population.
In 29 (80.6%) patients moderate PE was diagnosed before current hospitalization. In 9 (25%) and 20 (55.6%) patients, PE symptoms manifested at 30-32 and 34-36 weeks’ gestation, respectively. All of them received antihypertensive therapy and were observed in an outpatient setting.
Subsequently, 16 patients were hospitalized in the intensive care unit (ICU) and 20 in the postpartum department with PE symptoms and headache complaints. One patient who was admitted after childbirth had partial loss of vision in the right eye in addition to a headache.
At the time of hospital admission, 10 and 6 patients were at 34–36.6 and 37–40.6 weeks’ gestation, respectively. In the postpartum period, patients were transferred 12–48 hours after delivery.
Of the 16 pregnant women, who were hospitalized in the ICU, at the time of admission 2, 8 and 6 patients had blood pressure 130/90, 140-159/100, 160-180/100-100 mm Hg, respectively. Moderate and severe proteinuria were detected in 8 and 5patients, respectively. Of the additional PE symptoms, almost all pregnant women (14 out of 16) had edema in the legs and hands, 7 had thrombocytopenia (110–150*109/l). Four patients had a 2-3-fold increase in liver transaminase (ALT, AST) levels. According to fetal ultrasound and Doppler ultrasound of the uteroplacental circulation, 4, 7 and 8 patients were found to have stage I fetal growth restriction, moderate oligohydramnios, and impaired uterine arterial blood flow, respectively.
Among the 20 patients, who were admitted to the ICU after childbirth, blood pressure at the time of headache occurrence was 130/90, 140–159/100, 160–180/100–100 mm Hg in 2, 10 and 8 patients, respectively. Therefore, in more than in half of them, BP was consistent with moderate PE. Upon admission to the hospital and during childbirth, as well as in the postpartum period before the worsening of patients’ condition, the level of blood pressure in them varied from 120/80 to 135/85 mm Hg. Moderate and severe proteinuria were detected in 5 and 4 of them, respectively. Of the additional symptoms of PE, almost all (14 out of 16) patients had edema in the legs and hands; 9 had thrombocytopenia (110–150*109/l); 4 patients had a 2-3-fold increase in liver transaminase levels. Twelve patients had a normal vaginal delivery with epidural anesthesia, and 8 underwent a cesarean section. Four of them received elective cesarean section due to previous cesarean uterine scar, and 4 were operated on because of the acute fetal hypoxia in the first stage of labor. In the postpartum period, all patients were on antihypertensive therapy; however, none of them received magnesium sulfate.
More than half (n = 24, 66.7%) of patients had atypical PE with the levels of blood pressure and proteinuria - the “classical” criteria of PE - inconsistent with the real severity of their condition (Fig. 1) owing to additional PE symptoms (edema, thrombocytopenia, elevated levels of liver transaminases - Fig. 2) and signs of CNS involvement (headache).

For an objective assessment of the brain and better diagnostic accuracy, the patients underwent a brain MRI. Seventeen (47.2%) patients were diagnosed with various brain changes (Table 2). In 15 of them (41.7%), the identified abnormalities were associated with arterial hypertension, including posterior reversible encephalopathy syndrome (PRES) (n = 5, 13.9%) (Fig. 1a), stroke (n = 2, 5.6%) (Fig. 1b), vascular brain lesions (n = 8, 22.2%);
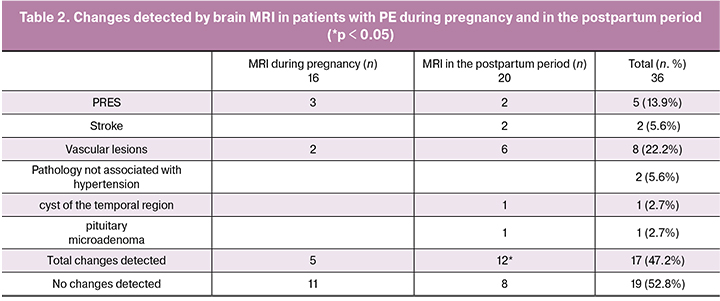
In 2 patients the identified brain lesions were not associated with arterial hypertension and included a cyst of the left temporal region in 1 (2.8%) patient and a pituitary microadenoma in 1 (2.8%) patient (Fig. 1c). The patients were referred to specialists. In 19 (52.8%) patients, brain MRI showed no abnormalities.
The table shows brain MRI findings in relation to the study time (during pregnancy or in the postpartum period). MRI-detected changes in the brain were found significantly more often (p < 0.05) in the postpartum period. Taking into account the atypical course of PE in half of the patients, special attention was paid to the analysis of the characteristics of the course and manifestations of the disease depending on brain MRI findings.
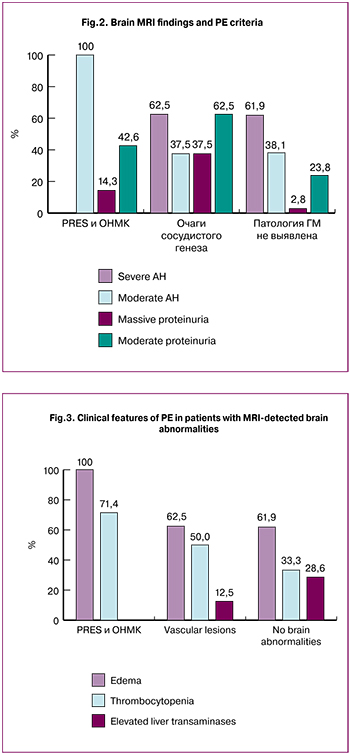 PRES was diagnosed in 3 patients during pregnancy and in 2 during the postpartum period. This syndrome is characterized by a reversible leukoencephalopathy without significant destruction of white matter. In the absence of timely and appropriate treatment, it can result in delayed irreversible damage to the brain, which underscores the need for an early diagnosis to identify the appropriate patient management strategy [4]. PRES is believed to occur in response to a sudden and sharp increase in blood pressure with subsequent impairment of cerebral autoregulation. In these cases, the absolute value of blood pressure is not of much significance [5], which is confirmed by the results of our study (Fig. 2). It is noteworthy that 3 out of 5 patients with PRES were hospitalized with the first episode of arterial hypertension during pregnancy, and their blood pressure at the onset of a headache was in the range of 130–159/90–100 mm Hg, while the blood pressure to which they are adapted was 100–110/70 mm Hg. Only 2 of these patients had moderate proteinuria. Of additional PE criteria, edema in the shins and feet was observed in all patients and thrombocytopenia in 2 of 5 (Fig. 3).
PRES was diagnosed in 3 patients during pregnancy and in 2 during the postpartum period. This syndrome is characterized by a reversible leukoencephalopathy without significant destruction of white matter. In the absence of timely and appropriate treatment, it can result in delayed irreversible damage to the brain, which underscores the need for an early diagnosis to identify the appropriate patient management strategy [4]. PRES is believed to occur in response to a sudden and sharp increase in blood pressure with subsequent impairment of cerebral autoregulation. In these cases, the absolute value of blood pressure is not of much significance [5], which is confirmed by the results of our study (Fig. 2). It is noteworthy that 3 out of 5 patients with PRES were hospitalized with the first episode of arterial hypertension during pregnancy, and their blood pressure at the onset of a headache was in the range of 130–159/90–100 mm Hg, while the blood pressure to which they are adapted was 100–110/70 mm Hg. Only 2 of these patients had moderate proteinuria. Of additional PE criteria, edema in the shins and feet was observed in all patients and thrombocytopenia in 2 of 5 (Fig. 3).
Based on detected abnormalities, 3 pregnant women underwent an emergency cesarean section, and 2 puerperal women were transferred to the ICU; that is, the brain MRI led to a more accurate diagnosis, resulting in improved management strategies without unnecessary prolongation of pregnancy.
The Nationwide Inpatient Sample of women aged 15 to 44 years has shown that the majority of stroke associated with pregnancy occurred in the postpartum period [5]. In our study, 2 patients had postpartum hemorrhagic strokes. Patients were admitted to the hospital with the first episode of arterial hypertension during pregnancy, and the blood pressure at the time of the headache attack, which in one of them was accompanied by partial loss of vision in the right eye, was 140–159/100 mm Hg. (Fig. 2) One of them had moderate, and the other massive proteinuria, both of them had swelling and thrombocytopenia (Fig. 3). The current literature reported some evidence suggesting the relationship between ischemic and hemorrhagic stroke in PE with PRES, which indicates the need for timely diagnosis of the latter to avoid the brain hemorrhage [6].
The vascular lesions detected in our study in 2 pregnant and 6 puerperal women reflect brain tissue ischemia co-occurring with periodic rises in blood pressure. In the all 8 patients, hypertension was diagnosed before pregnancy, and they received irregular antihypertensive therapy. According to the literature, such brain lesions are most characteristic of patients with a history of hypertension, hypertensive disorders of pregnancy, especially with hypertension crises and in the absence or inadequate antihypertensive therapy [7]. Although this type of brain changes is not an acute condition and is often asymptomatic, without adequate antihypertensive therapy, they may lead to a stroke in ischemic zones [1, 7].
All 8 patients with MRI-detected vascular brain lesions were diagnosed with PE before they were admitted to the hospital. Their PE symptoms were first noted at 30–34.6 weeks’ gestation, and at the time of hospital admission, the disease lasted at least 4 weeks, which explains the identified brain abnormalities. At the time of hospital admission, their blood pressure was in the range of 140–170/100 mm Hg, all of them had proteinuria (5 - moderate, 3 - massive) (Fig. 2). Besides, 5 of them had edema, 4 - thrombocytopenia, 2 – increased liver transaminases (Fig. 3). During pregnancy, 2 patients in this group underwent MRI due to a headache. Given the identified brain changes and the presence of all PE criteria, both pregnant women underwent a cesarean section. In 6 patients a headache manifested during the postpartum period. Of them, 2 patients had a vaginal delivery, and 4 underwent cesarean section due to high blood pressure in combination with other PE criteria and ineffective therapy; in the postpartum period, they received antihypertensive therapy.
Thus, the brain MRI offers an opportunity for the timely detection of changes in the central nervous system, thus improving the identification of the appropriate patient management strategy and reducing the risk of severe complications, in particular, cerebral hemorrhages.
Nineteen patients had no brain abnormalities detected on MRI. In 5 of them, MRI scans were performed during pregnancy and in 14 after childbirth. Despite the absence of MRI-detected brain abnormalities, all pregnant women underwent cesarean section due to high blood pressure at the hospital admission (155–170/100 mm Hg), ineffective therapy and various combinations of hypertension with proteinuria (n = 10), edema (n = 13), thrombocytopenia (n = 7) and increased transaminase values (n = 6). In these patients, as a rule, the severity of the “classic” PE symptoms was consistent with the severity of their condition, which helped to avoid unnecessary prolongation of pregnancy. Of the 14 patients, who underwent MRI after delivery, 12 were diagnosed with PE before pregnancy. They were on antihypertensive therapy before delivery and in the postpartum period. However, none of them received magnesium sulfate, which probably caused the progression of the disease and a headache in the postpartum period. Adequate therapy helped stabilize their condition.
Thus, the use of brain MRI along with an objective assessment of the central nervous system, allowed us to more accurately determine the severity of PE, which contributed to a safe and timely delivery and appropriate therapy.
Results
- A total of 47.2% of patients, who had PE, headache complaints and/or visual impairment were found to have MRI-detected brain abnormalities; 88% of them, including PRES (13.9%), stroke (5.6%), and vascular lesions (22.2%) were associated with arterial hypertension.
- Cerebral complications of PE (PRES and a stroke) had atypical manifestations when the severity of the “classic” PE symptoms was inconsistent with the severity of the patient’s condition.
- The findings of the objective brain assessment contributed to an adequate assessment of PE severity, timely delivery, and appropriate therapy in the postpartum period in 41.7% of patients.
- Using brain MRI in patients with PE of any severity at the onset of neurological manifestations results in a reduction in the incidence of its severe complications, in particular in the incidence of a cerebral hemorrhage.
References
- Sperling J.D., Dahlke J.D., Huber W.J., Sibai B.M. The role of headache in the classification and management of hypertensive disorders in pregnancy. Obstet. Gynecol. 2015; 126(2): 297-302.
- Попков А.В., Долгошапко О.Н. Новые подходы в оценке неврологического статуса у пациенток с преэклампсией. Медико-соціальні проблеми сім’ї. 2011; 16(1): 41-3. [Popkov A.V., Dolgoshapko O.N. New approaches in the assessment of neurological status in patients with preeclampsia. Medico-social problems of si’’ї. 2011; 16 (1): 41-3. (in Russian)]
- Перфилова В.Н., Михайлова Л.И., Тюренков И.Н. Последствия гестоза (преэклампсии). Российский вестник перинатологии и педиатрии. 2014; 59(2): 13-8. [Perfilova V.N., Mikhailova L.I., Tyurenkov I.N. The effects of preeclampsia (preeclampsia). Russian Bulletin of Perinatology and Pediatrics. 2014; 59 (2): 13-8. (in Russian)]
- Скворцова В.И., Губский Л.В., Мельникова Е.А. Синдром задней обратимой энцефалопатии. Журнал неврологии и психиатрии им. С.С.Корсакова. 2010; 110(5): 104-9. [Skvortsova V.I., Gubsky L.V., Melnikova E.A. Syndrome posterior reversible encephalopathy. Journal of Neurology and Psychiatry. S.S. Korsakova. 2010; 110 (5): 104-9. (in Russian)]
- Попова Н.А., Хафизова И.Ф., Якупов Э.З. Неврологические проявления гестоза (клиническое наблюдение). Вестник современной клинической медицины. 2014; 7(2): 150-4. [Popova N.A., Khafizova I.F., Yakupov E.Z. Neurological manifestations of preeclampsia (clinical observation). Bulletin of modern clinical medicine. 2014; 7 (2): 150-4. (in Russian)]
- Лихачев С.А., Астапенко А.В., Осос Е.Л. Неврологические проявления гестоза. Международные обзоры: клиническая практика и здоровье. 2013; 6: 54-63. [Likhachev S.A., Astapenko A.V., Osos E.L. Neurological manifestations of preeclampsia. International reviews: clinical practice and health. 2013; 6: 54-63. (in Russian)]
- Staykov D., Schwab S. Posterior reversible encephalopathy syndrome. J. Intensive Care Med. 2012; 27(1): 11-24.
Received 22.02.2018
Accepted 02.03.2018
About the Authors
Shalina, Raisa I., MD, professor at the Department of Obstetrics and Gynecology, Pediatric Faculty of N.I. Pirogov RNRMU of Minzdrav of Russia.117997, Russia, Moscow, Ostrovityanov str. 1. Tel.: +74957183472. Е-mail: raisa.shalina@gmail.com
Kurtser, Mark A., professor, head of the Department of Obstetrics and Gynecology, Pediatric Faculty of N.I. Pirogov RNRMU of Minzdrav of Russia, Dr.Med.Sci.,
Academician of the RAS. 117997, Russia, Moscow, Ostrovityanov str. 1. Tel.: +74957183472. Е-mail: m.kurtser@mcclinics.ru
Simukhina, Mariya A., PhD, student at the Department of Obstetrics and Gynecology, Pediatric Faculty of N.I. Pirogov RNRMU of Minzdrav of Russia.
117997, Russia, Moscow, Ostrovityanov str. 1. Tel.: +79104675239. Е-mail: msimuhina@gmil.com
Latyshkevich, Oleg A., PhD, teaching assistant at the Department of Obstetrics and Gynecology, Pediatric Faculty of N.I. Pirogov RNRMU of Minzdrav of Russia.
117997, Russia, Moscow, Ostrovityanov str. 1. Tel.: +74957183472. E-mail: agpf.gms@gmail.com
Lebedev, Evgenii V., associate professor at the Department of Obstetrics and Gynecology, Pediatric Faculty of N.I. Pirogov RNRMU of Minzdrav of Russia.
117997, Russia, Moscow, Ostrovityanov str. 1. Tel.: +74957183472. Е-mail: agpf.gms@gmail.com
Shtabnitskii, Andrei M., deputy chief physician for Anesthesiology and Intensive Care, Perinatal Medical Center. Address:
117209, Russia, Moscow, Sevastopolsky Prosp., 24, build. 1. Phone: +74957197896
Platitsyn, Igor’ V., PhD, head of Diagnostic Imaging 4, Lapino Clinical Hospital.
143081, Russia, Moscow Region, Odintsovo District, 1st Uspenskoye Shosse, Lapino, 111. Tel.: +74955266161.
For citation: Shalina R.I., Kurtser M.A., Simukhina M.A., Latyshkevich O.A., Lebedev E.V., Shtabnitskii A.M., Platitsyn I.V. Magnetic resonance imaging in the diagnosis of brain abnormalities in patients with severe preeclampsia. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (1): 68-73. (in Russian)
https://dx.doi.org/10.18565/aig.2019.1.68-73