Клиническая пельвиметрия (измерение наружных размеров таза с помощью тазомера) традиционно остается важной составляющей акушерского обследования [1–3]. Целью пельвиметрии является прогнозирование клинического несоответствия между размерами предлежащей части плода и таза матери, приводящего к затруднению или невозможности рождения ребенка (цефалопельвическая диспропорция или клинически узкий таз) [4, 5]. Клинически узкий таз – одна из главных причин материнского родового травматизма, перинатальной заболеваемости и смертности, экстренного оперативного родоразрешения [6–8].
При выраженном сужении таза (уменьшение наружных размеров более чем на 2 см) [8, 9] клиническая пельвиметрия позволяет уверенно прогнозировать затрудненные роды, обусловленные уменьшением размеров его полости. Вместе с тем в современной практике преобладают умеренные и незначительные степени сужения таза, при которых толщина костей, индивидуальные особенности формы таза существенно снижают точность прогноза [9].
В связи с этим было предложено использовать рентгеновскую пельвиметрию, первые публикации о применении которой датируются 20-ми годами прошлого столетия. Одним из существенных недостатков метода являлось наличие ионизирующего излучения. В конце прошлого столетия для снижения лучевой нагрузки была разработана низкодозная рентгеновская пельвиметрия, которая, к сожалению, унаследовала основные недостатки оригинальной методики, а именно большую погрешность изменений. С появлением и широким внедрением компьютерной томографии (КТ) удалось избавиться от недостатков рентгеновской пельвиметрии и значительно снизить лучевую нагрузку при выполнении низкодозной КТ-пельвиметрии [10–16]. Тем не менее наличие лучевой нагрузки, высокая стоимость исследования, а также погрешность измерений, связанная с ограничениями методики, привели к тому, что методы рентген-пельвиметрии стали применять у ограниченной группы женщин (тазовое предлежание, рубец на матке). Проведенный в Кокрановском обзоре анализ не показал клинической эффективности рентгеновских методов пельвиметрии [13]. Более того, частота кесарева сечения была выше в группе женщин, у которых была проведена рентген-пельвиметрия, по сравнению с пациентками после клинической пельвиметрии или в ее отсутствие.
В 1985 г. в клиническую практику была внедрена магнитно-резонансная пельвиметрия (МР-пельвиметрия) [14, 15]. С появлением МР-томографов, оснащенных сверхбыстрыми одноимпульсными последовательностями, появилась возможность выполнять МР-пельвиметрию за считаные минуты; при этом лучевая нагрузка на пациентку и плод полностью отсутствует [16, 17].
В настоящее время имеется большое количество отечественных и зарубежных публикаций, в которых показано значение метода в прогнозировании патологических родов [18], выявлении риска дистоции плечиков [5], диагностики узкого таза [18–21], в том числе «стертых» форм [9, 22], выборе метода родоразрешения при тазовом предлежании плода [23].
На сегодняшний день магнитно-резонансная томография является технологией, которая активно развивается во всех сферах медицинской диагностики, включая акушерство, гинекологию и неонатологию, и соответствующим оборудованием оснащены перинатальные центры. Вместе с тем анализ литературы свидетельствует о наличии разночтений как техники выполнения самой процедуры, так и референсных значений размеров таза, определяемых при данном исследовании [24–28].
Таким образом, для дальнейшего развития и эффективного внедрения в клиническую практику метода МР-пельвиметрии важное значение имеет его стандартизация и отработка методики.
Целью нашей работы явилось представление используемой нами методики МР-пельвиметрии и сравнение референсных значений с данными других авторов.
Материалы и методы
В данной работе представлены показания, противопоказания, методика и референсные значения МР-пельвиметрии, которая используется на регулярной основе в ФГБУ «Национальный медицинский исследовательский центр акушерства, гинекологии и перинатологии имени академика В.И. Кулакова» Министерства здравоохранения Российской Федерации с 1998 г. За прошедший период проведено более 2500 МР-пельвиметрических исследований.
Показания для проведения МР-пельвиметрии (являются относительными и применяются с учетом клинической ситуации) [26].
1. Высокий риск перинатальной патологии: повторнородящие с осложненным течением и неблагоприятным исходом предыдущих родов (влагалищные оперативные роды, интранатальная смерть плода, родовая травма, нарушение неврологического статуса у ребенка или ранняя неонатальная смертность доношенных детей в результате родовой травмы) [26].
2. Сужение наружных размеров таза более чем на 1,5–2 см, травма таза в анамнезе, перенесенные рахит и полиомиелит, врожденный вывих тазобедренных суставов [26].
3. Признаки формирующейся диспропорции между тазом матери и головкой плода: неустойчивое положение, косое положение, тазовое предлежание плода (если нет другой причины: многоводие, аномалия развития матки, миома матки) [26].
4. Симфизиопатия, расхождение лонных костей [26].
МР-пельвиметрия также может быть проведена в послеродовом периоде (клинически узкий таз, родовая травма, затяжное течение родов и пр.) [26].
Противопоказания к проведению МР-пельвиметрии [26].
Абсолютные противопоказания.
1. Наличие кардиостимулятора либо других электронных имплантируемых устройств (протез внутреннего уха, инсулиновая помпа и т.д.).
2. Наличие ферромагнитных инородных тел (например, осколок внутри или вблизи глазного яблока, клипсы на сосудах головного мозга и т.д.).
Следует обратить внимание, что на сегодняшний день существуют отдельные модели вышеуказанных устройств (кардиостимулятор, клипсы), которые специально разработаны и испытаны в сильном магнитном поле; с данными моделями проводить магнитно-резонансную томографию возможно.
Остальные противопоказания являются относительными и к ним относят.
1. Беременность в I триместре.
2. Наличие имплантированных металлических устройств и конструкций (остеосинтез, искусственные клапаны сердца, протез сустава, кава-фильтр и т.д.).
Известно, что большинство выпускаемых на сегодняшний день имплантируемых изделий изготавливаются из немагнитных сплавов и не могут причинить вред здоровью пациента во время исследования, однако таковыми являются не все. Если у пациентки имеются имплантированные металлические конструкции либо устройства, рекомендована консультация врача-рентгенолога [26]. Окончательное решение о возможности либо невозможности проведения исследования принимает врач-рентгенолог на основании медицинской документации производителя имплантированного устройства.
Характеристика оборудования и протокол исследования
Исследование проводится на МР-томографах с индукцией поля 1,5 и 3Т по следующему протоколу (табл. 1). Рекомендуемые сроки проведения: III триместр, оптимально – после 36 недель. Используют импульсные последовательности (одноимпульсное, быстрое спин-эхо – SSFSE, HASTE). Продолжительность исследования составляет 5–10 минут. Результатами исследования служат полученные внутренние размеры таза, лобно-затылочный и битемпоральный размеры головки плода, а также выявленные признаки симфизита, наличия экзостозов, последствий травматического повреждения костей таза, копчика и их деформация, идиопатических переломов боковых масс крестца.
Методика выполнения МР-пельвиметрии
1. Позиционирование пациентки: пациентка укладывается на спину, в III триместре – с поворотом на правый бок приблизительно на 15 градусов для предотвращения компрессии нижней полой вены, фиксируется с помощью валиков и подушек. На зону интереса накладывается поверхностная катушка, при этом центр катушки позиционируется на зону интереса. При невозможности пациентки лежать на спине возможно проведение исследования на боку (вынужденное положение). Центровка осуществляется по центру катушки для достижения оптимальных условий сканирования.
2. Исследование начинается с обзорной программы для планирования последующих последовательностей. Обзорная программа получает изображения в трех ортогональных проекциях и служит исключительно для планирования последующих срезов.
3. Т2-взвешенные изображения (Т2ВИ) (SSFSE/HASTE) в сагиттальной плоскости (по отношению к осям тела), толщина среза 3–4 мм, матрица квадратная не менее 320×320, поле обзора 320–400 мм (рис. 1). Сагиттальные томограммы служат для измерения прямых размеров таза: входа, широкой части полости, узкой части полости, выхода (расстояние от нижнего края лонного сочленения до копчика), длины и деформации копчика и кривизны крестца. Все измерения проводятся на срединном срезе, проходящем через лонное сочленение.
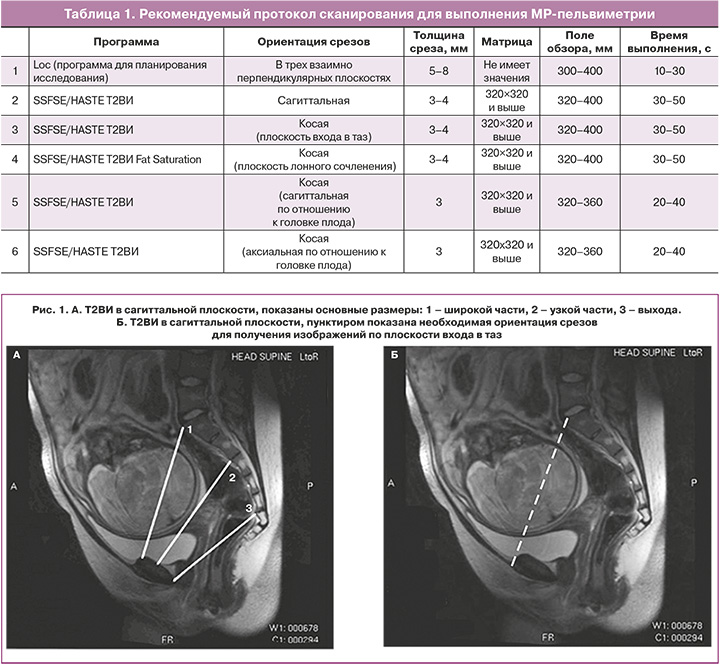
4. Т2ВИ (SSFSE/HASTE) в косой поперечной плоскости (плоскость входа в таз), толщина среза 3–4 мм, матрица квадратная не менее 320×320, поле обзора 300–340 мм томограммы позиционируют, как показано на рисунке 1, с использованием полученных сагиттальных срезов параллельно linea innominata. На полученных томограммах измеряют поперечные размеры таза: наибольший размер входа, широкой части, межостного, битуберозного (рис. 2).

5. При исследовании после 36-й недели необходимо оценить лонное сочленение с помощью Т2ВИ (SSFSE/HASTE) с подавлением МР-сигнала от жировой ткани. При выявлении расширения лонного сочленения, отека хряща, неровности контуров лонных поверхностей, узурации, зон отека костного мозга смежных поверхностей лонного сочленения (имеют повышенную интенсивность МР-сигнала), устанавливается диагноз симфизита (рис. 3). Толщина среза должна составлять 3–4 мм, матрица квадратная не менее 320×320, поле обзора 300–340 мм томограммы позиционируют, как показано на рисунке 3, с использованием ранее полученных сагиттальных и косых срезов.

6. Для оценки размеров головки плода выполняются две взаимно перпендикулярные программы Т2ВИ (SSFSE/HASTE), ориентированные по аксиальной и сагиттальной плоскостям головки с измерением лобно-затылочного и битемпорального размеров (рис. 4). Толщина среза должна составлять 3 мм, матрица квадратная не менее 320×320, поле обзора 320–360 мм томограммы позиционируют с использованием ранее полученных срезов.
Все измерения размеров таза производят в соответствии с классическим определением плоскостей [5, 8, 9, 26–30]: прямой размер входа – от наиболее выступающей точки мыса крестца до наиболее выступающей точки середины верхней поверхности симфиза (акушерская конъюгата); поперечный – наиболее удаленное расстояние между терминальными линиями; прямой широкой части полости таза – от сочленения второго-третьего крестцовых позвонков до середины внутренней поверхности симфиза; поперечный – между проекциями середин вертлужных впадин на внутреннюю поверхность таза; прямой узкой части – от крестцово-копчикового сочленения до середины нижнего края симфиза; поперечный узкой части – между седалищными остями (межостный); прямой выхода – от верхушки копчика до середины нижнего края симфиза; поперечный выхода – между седалищными буграми (битуберозный) [5, 8, 9, 26–30].
По результатам исследования, проведя все необходимые измерения, врач-рентгенолог заполняет таблицу полученных размеров таза (табл. 2), сравнивая полученные значения с референсными (нижняя граница нормальных размеров приведена в табл. 2). Следует отдельно отметить, что патологическими считаются размеры таза, отличающиеся от нормальных на 0,6–1,2 см, и в таблице уже приведены размеры, соответствующие нижней границе условно нормальных размеров [5, 8, 9, 25–30]. Также врач указывает наличие либо отсутствие признаков симфизита (после 36 недели) и размеры головки плода (рекомендуется после 38 недели). Типичные формы анатомического сужения таза в зависимости от размеров приведены в таблице 3 [28].

Результаты и обсуждение
Оценка собственных данных и результатов, полученных при МР-пельвиметрии другими исследователями, свидетельствует об одинаковом подходе к определению размеров полости таза. Некоторые исследователи не выделяют поперечный размер плоскости входа и прямой размер выхода таза. Данное положение может быть обусловлено крайне низкой вероятностью существенного сужения поперечного размера плоскости входа и наличием подвижности крестцово-копчикового сочленения. Вместе с тем, по нашему мнению, отсутствие этих сведений уменьшает ценность результатов исследования, так как может затруднять оценку формы таза, а ограничение или неподвижность крестцово-копчикового сочленения при уменьшении прямого размера будет мешать продвижению головки плода. Определение этих размеров не требует применения дополнительных сечений и не сопровождается существенной потерей времени. Поэтому, с целью информирования клинициста, данные размеры рекомендуется учитывать при оценке результатов МР-пельвиметрии.Как было указано выше, в литературе имеются некоторые расхождения в значениях результатов измерений таза. Данное положение может быть обусловлено как антропологическими особенностями изучаемой популяции, так и применяемой методикой исследования (рентген, компьютерная томография, магнитно-резонансная томография). Так, по сравнению с нашими данными, в исследовании F. Hampel et al. (2018) [20] прямой размер входа в таз составлял в среднем 130,8±8,4 мм, что значительно выше, чем в нашей популяции, а также результатов, полученных другими авторами. В то же время средние значения поперечных размеров узкой части и выхода таза в данном исследовании соответствовали минимально допустимым в нашей когорте, 105,2±8,4 и 118,4±13,1 мм соответственно. Однако следует обратить внимание, что в исследование F. Hampel et al. (2018) [20] было включено только 25 первородящих женщин.
В то же время, при сравнении с результатами более широких исследований, наши данные существенно не отличались. Так, в исследовании M. Zaretsky et al. (2005) [18] (78 женщин с неосложненными родами и 23 с клинически узким тазом) акушерская конъюгата у женщин с неосложненным течением родов составляла в среднем 119,6±8,6 мм; поперечный размер входа – 130,2±7,6 мм; переднезадний широкой части – 124,6±8,2 мм; межостный – 119,1±8,4 мм. При этом акушерская конъюгата, переднезадний размер полости и межостный были достоверно больше, чем в группе клинически узкого таза: 115,0±9,3 мм (р<0,03); 116,2±8,0 мм (р<0,001) и 113,0±9,7 (р<0,004).
Также наши результаты не отличались от данных исследования T. Keller et al. (2003) [24], которое включало 100 женщин со спонтанными родами и 130 родоразрешенных путем кесарева сечения по поводу клинически узкого таза. По данным этого исследования, прямой размер входа составлял в среднем 121,7±8,6 мм; узкой части – 115,8±9,9 мм; поперечные широкой, узкой и выхода – 129,5±8,7, 112,3±7,9 и 120,6±11,3 мм соответственно. При этом средние значения всех указанных размеров в группе клинически узкого таза были достоверно меньше: 113,7±10,0 мм (р<0,0001); 111,1±10,3 мм (р=0,0004); 124,3±9,7 мм (р=0,0002); 105,0±8,4 мм (р<0,0001); 112,7±9,6 мм (р<0,0001).
Заключение
Диагноз анатомического сужения таза и его формы должен опираться на объективные данные, что имеет важное значение при выборе тактики родоразрешения беременных группы риска. В настоящее время МР-пельвиметрия представляет собой наиболее эффективный и безопасный метод объективной оценки размеров полости таза.
Представленная методика МР-пельвиметрии и референсные значения показателей сопоставимы с результатами других исследователей и могут применяться в отделениях лучевой диагностики по назначению акушера-гинеколога. Использование данного метода будет способствовать снижению частоты осложнений в родах и дальнейшему его совершенствованию на основе продолжения научных исследований.