Железодефицитная анемия (ЖДА) является одним из самых распространенных заболеваний в мире и стоит на первом месте по частоте встречаемости у женщин детородного возраста [1, 2]. Распространенность ЖДА зависит от многих причин: социально-экономических условий проживания, питания, кровотечений различной локализации, поражения паразитарными заболеваниями и др. Экспертами ВОЗ было показано, что анемия чаще встречается в развивающихся странах и наиболее подвержены анемии две группы населения – дети раннего возраста и беременные женщины [3]. Известно, что ЖДА составляют 90% всех анемий в детском возрасте [4] и 80% всех анемий у взрослых [5]. По мнению экспертов ВОЗ, распространенность ЖДА в популяции может быть умеренной – от 5 до 19,9%, средней – от 20 до 39,9% и высокой – 40% и более [3]. Основными причинами развития ЖДА у женщин репродуктивного возраста служат обильные менструальные кровотечения (ОМК), беременность, роды (особенно повторные) и лактация. Развитие ЖДА возможно у доноров крови, постоянно сдающих кровь в течение многих лет, а также у пациентов с хронической почечной недостаточностью, находящихся на программном гемодиализе (еженедельные потери 30–40 мл крови в контуре диализатора) [1, 5, 6]. До 29% небеременных женщин в возрасте 15–49 лет имеют анемию, что соответствует приблизительно 500 млн жительниц планеты [7]. Наиболее частой причиной анемии является дефицит железа [1, 8]. Причиной дефицита железа у женщин репродуктивного возраста в большинстве случаев становится менструальная кровопотеря [8, 9]. ЖДА является независимым фактором риска повышенной заболеваемости и смертности [10]. При этом часто причина дефицита железа и ЖДА у женщин долго не диагностируется: за медицинской помощью к гинекологу обычно обращаются женщины с нерегулярными аномальными маточными кровотечениями, но не с обильными менструациями [8]. Низкая обращаемость за помощью женщин с ОМК обусловлена субъективной оценкой и зачастую неверным пониманием причин как обильных менструаций, так и неспецифичных симптомов, связанных с дефицитом железа и анемией [11]. Поэтому врачи общей практики и акушеры-гинекологи, осуществляющие прием условно здоровых женщин с целью диспансерного осмотра или консультирования по вопросам планирования семьи, должны прицельно интересоваться характеристиками менструации и своевременно выявлять ЖДА и латентный дефицит железа (ЛДЖ), требующие обязательной коррекции [11]. Более того, на этапе прегравидарной подготовки в восстановлении запасов железа нуждаются женщины с ЛДЖ, диагностируемым по уровням ферритина [11].
Цель исследования: представить собственный опыт применения препарата «Ферретаб комп.» для лечения ЖДА и железодефицитных состояний у пациенток с ОМК.
Материалы и методы
Проведены обследование и лечение 34 женщин репродуктивного возраста от 18 до 45 лет с ОМК на клинической базе кафедры акушерства и гинекологии Клиника «Медицинский консультативный центр» ФГБОУ ВО НГМУ Минздрава России в период 2020–2022 гг.
Критерии включения: возраст 18–45 лет, диагностированное хроническое обильное маточное кровотечение – чрезмерная менструальная кровопотеря, которая оказывает влияние на физическое, социальное, эмоциональное и/или материальное благополучие женщины.
Критерии исключения: возраст младше 18 и старше 45 лет, олиго- и аменорея, беременность, менопауза и кровотечение в постменопаузе, применение гормональных препаратов (в том числе препаратов гормональной контрацепции и менопаузальной или заместительной гормональной терапии), кровоостанавливающих лекарственных средств.
Клинико-анамнестическое обследование включало опрос с уточнением репродуктивного анамнеза, наличия соматических и гинекологических заболеваний, жалоб, потенциально связанных с дефицитом железа. Для оптимизации диагностики ОМК группой HELP был создан алгоритм диагностического поиска, который начинается со сбора анамнеза и объективизации чрезмерной менструальной кровопотери, и с этой целью группа HELP разработала специальный краткий опросник, который поможет докторам во время приема за очень короткое время выявить проблему, выяснив характеристики менструального цикла и оценку менструального кровотечения с помощью ответа женщин на 3 главных вопроса [13].
1. Насколько обильны Ваши кровотечения?
- Меняете ли Вы санитарные средства ночью/просыпаетесь ли для того, чтобы сменить прокладки?
- Во время дней наиболее обильного кровотечения промокают ли полностью Ваши средства защиты после 2 ч?
2. Влияет ли это на Ваше физическое состояние?
- Наблюдаете ли Вы выделение больших сгустков во время менструации?
- Была ли у Вас выявлена анемия или дефицит железа во время менструаций?
3. Влияет ли это на качество жизни?
- Вынуждены ли Вы специально организовывать Вашу социальную жизнь в эти дни?
- Беспокоитесь ли Вы о неприятных моментах, связанных с кровотечением?
У всех участниц исследования определяли уровень сывороточного ферритина и показатели общего анализа крови: уровень гемоглобина, количество эритроцитов, гематокрит. ЖДА определялась при уровне гемоглобина <120 г/л. При уровне гемоглобина ≥120 г/л ЛДЖ устанавливали по уровню ферритина <30 мкг/л (учитывали в анализе показатель гемоглобина, на основании которого установлен диагноз ЖДА, и показатель ферритина, на основании которого диагностировали ЛДЖ) [14–16].
Пациентки были разделены на 2 группы: 1-я группа – 22 женщины с ЖДА легкой степени тяжести; 2-я группа – 12 пациенток с ЛДЖ.
Для лечения дефицита железа использовали препарат, содержащий в одной капсуле для перорального приема 163,56 мг железа (II) фумарата (эквивалентно 50 мг железа) и фолиевую кислоту 500 мкг. Режим терапии выбирался в зависимости от диагноза: при ЖДА суточная доза составила 2 капсулы, при ЛДЖ – 1 капсулу.
Оценка эффективности терапии проводилась через 8 недель по динамике концентрации гемоглобина и сывороточного ферритина, а также жалоб пациенток, связанных с дефицитом железа.
Результаты
В исследование были включены 34 пациентки от 18 до 45 лет, соответствовавшие критериям включения и исключения. Среди включенных в исследование пациенток 9/34 (26,5%) в анамнезе не имели беременностей, 12/34 (35,3%) рожали, у 13/34 (38,2%) беременности были прерваны спонтанно или путем искусственного аборта. У 21/34 (61,8%) пациентки соматические заболевания не выявлены. Сердечно-сосудистые заболевания отмечали 2/34 (5,9%), бронхолегочные заболевания – 4/34 (9,3%), болезни желудочно-кишечного тракта – 4/34 (11,8%), заболевания мочевыделительной системы – 3/34 (8,8%), эндокринные заболевания – 6/34 (17,6%) женщин. Среди гинекологических заболеваний диагностирована миома матки – у 8/34 (23,5%), генитальный эндометриоз – у 8/34 (23,5%), хронические воспалительные заболевания органов малого таза – у 1/34 (2,9%) пациенток.
При консультировании было выявлено, что неспецифические симптомы (усталость, снижение работоспособности), связанные с дефицитом железа, испытывали все пациентки. Эпизоды головокружения, головную боль отмечали 7/34 (20,6%) женщин; онемение конечностей, зябкость, «беспокойные ноги» – 4/34 (11,7%) больных; шум в ушах, потемнение в глазах – 1/34 (2,9%); учащенное сердцебиение, чувство нехватки воздуха – 3/34 (8,8%); выпадение волос, ломкость ногтей – 22/34 (64,7%) пациенток. Связь ухудшения самочувствия с менструацией отметили все женщины.
Утвердительные ответы на дополнительные вопросы об обильности менструаций дали все пациентки.
- Отмечаете ли Вы выделение сгустков крови во время менструаций? – 11/34 (32,4%).
- Приходится ли Вам вставать ночью для замены гигиенического средства в дни менструаций? – 30/34 (88,2%).
- Вынуждены ли Вы планировать свою повседневную, социальную или иную активность в зависимости от дней наиболее интенсивного кровотечения? – 17/34 (50%).
При сборе анамнестических данных большая часть пациенток (21/34 (61,8%)) сообщили, что ранее никогда не обследовались на предмет диагностики дефицита железа. Среди пациенток, которые обследовались, 13/34 (38,2%) имели в анамнезе ЖДА или ЛДЖ, при этом только 6/13 (46,2%) получали терапию препаратами железа.
Средний уровень гемоглобина в 1-й группе составил 110 (100–119) г/л, ферритина – 12,5 (8,0–17,0) мкг/л.
Средний уровень гемоглобина во 2-й группе составил 124 (120–127) г/л, ферритина – 21 (16,0–26,0) мкг/л.
Пациенткам обеих групп назначали препарат, содержащий в одной капсуле для перорального приема 163,56 мг железа (II) фумарата (эквивалентно 50 мг железа) и фолиевую кислоту 500 мкг («Ферретаб комп.»).
Пациенткам 1-й группы для лечения анемии назначали «Ферретаб комп.» по 1 капсуле 2 раза в день за 40 минут до еды. Первая оценка результатов эффективности терапии осуществлялась на 30-й день приема препарата (уровень гемоглобина, количество эритроцитов, цветовой показатель, уровень ферритина). Длительность терапии была индивидуальной, но не более 2 месяцев. При нормальных показателях гемоглобина, эритроцитов и гематокрита назначалась терапия насыщения (восстановление запасов железа в организме) приемом «Ферретаб комп.» по 1 капсуле 1 раз в сутки, под контролем оценки уровня сывороточного ферритина. Длительность этой терапии была также индивидуальной, но не более 2 месяцев.
Пациенткам 2-й группы с ЛДЖ назначали «Ферретаб комп.» по 1 капсуле 1 раз в день за 40 минут до еды. Первая оценка результатов эффективности терапии осуществлялась на 30-й день приема препарата (общий анализ крови, сывороточный ферритин). Длительность лечения была индивидуальной, но не более 2 месяцев.
Мы отметили повышение концентрации гемоглобина с 110 г/л до 122 г/л в 1-й группе, с 124 г/л до 132 г/л – во 2-й группе и повышение ферритина с 12,5 мкг/л до 27,2 мкг/л – в 1-й группе и с 21 мкг/л до 32,6 мкг/л – во 2-й группе (табл. 1).
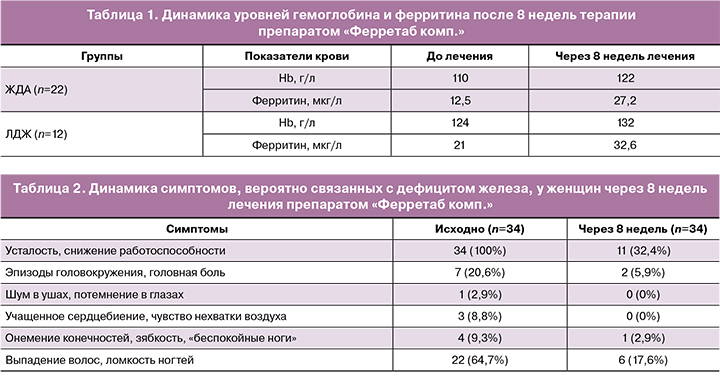
По прошествии 8 недель терапии мы оценили динамику симптомов, потенциально связанных с дефицитом железа, у женщин, получавших «Ферретаб комп.» Результаты анализа приведены в таблице 2.
Таким образом, следует отметить уменьшение доли пациенток с жалобами, активно выявляемыми при первоначальном опросе. Это косвенно подтверждает связь перечисленных неспецифических симптомов с дефицитом железа и демонстрирует клиническую эффективность применения препарата «Ферретаб комп.».
Обсуждение
Результаты нашего исследования подтвердили роль ОМК как фактора риска ЖДА и железодефицитных состояний вследствие недостаточной выявляемости гиперменореи и дефицита железа [8].
Исследование показало, что обычный клинический опрос позволяет диагностировать ОМК, особенно у тех женщин, которые, считая свои менструации нормальными, сообщают о вынужденном изменении обычной активности в дни наиболее интенсивных выделений. ОМК тесно ассоциированы с железодефицитными состояниями [17], а дополнительные факторы риска дефицита железа усугубляют ситуацию. Нельзя игнорировать высокую распространенность ЖДА среди женщин, не предъявляющих активных жалоб и обращающихся к врачу только по вопросам диспансеризации или консультирования в связи с планированием беременности или контрацепции. Выявление железодефицитных состояний и их своевременная коррекция являются важной составной частью прегравидарной подготовки. Учитывая эти данные, представляется целесообразным рекомендовать препараты железа в суточной дозе 40–60 мг всем женщинам с ОМК [14].
Для обеспечения приверженности к терапии оральными препаратами железа следует ориентироваться на выбор препарата с хорошей переносимостью, которая, в свою очередь, обеспечивается несколькими компонентами: технология изготовления, определяющая возможность пролонгированного высвобождения активных веществ, особенности солей, связывающих железо, и других ингредиентов лекарственного средства, вводимых в состав препарата для улучшения усвоения железа. Одним из таких препаратов является «Ферретаб комп.», в состав которого входят органическая соль (фумарат) железа и фолиевая кислота. Совместное применение железа и фолиевой кислоты оправдано не только улучшением всасывания железа, но и самостоятельной ролью фолатов в обеспечении гомеостаза. Состав и структура препарата «Ферретаб комп.» (мини-таблетки внутри капсулы) обеспечивают его пролонгированное действие, что позволяет применять препарат 1–2 раза в день.
Существенными требованиями к препаратам железа для приема внутрь являются удобство их применения и хорошая переносимость, что позволяет обеспечить высокий уровень приверженности пациентки назначенному лечению. Ни в одном случае нами не было зафиксировано непереносимости данного препарата, что обеспечивает высокий комплаенс к проводимой терапии.
Режим приема и титрация доз препаратов железа могут варьировать в зависимости от тяжести железодефицитного состояния, наличия сопутствующих заболеваний и индивидуальной переносимости (от 50 мг до 150 мг элементарного железа в сутки) [18].
Заключение
По нашему мнению, учитывая высокую распространенность железодефицитных состояний при ОМК, необходимость консультирования женщин врачами амбулаторного приема не вызывает сомнений. При выявлении ОМК целесообразными представляются назначение общего анализа крови, исследование ферритина и своевременный прием препаратов железа.