Пролапс тазовых органов является одним из наиболее распространенных заболеваний у женщин во всем мире. Сведения о распространенности пролапса органов малого таза по данным разных авторов варьируют, считается, что риск подвергнуться оперативному лечению по поводу пролапса гениталий имеют 11,8% женщин [1]. Поэтому в настоящее время существует множество хирургических методик лечения пролапса гениталий. Сакроспинальная фиксация стенки влагалища или шейки матки является одним из эффективных методов оперативного лечения пролапса гениталий у женщин в любом возрасте [2–6]. Частота послеоперационных геморрагических осложнений по разным данным варьирует от 0,2 до 2,2% [7–9], как правило, они проявляются образованием забрюшинных гематом малого таза.
В настоящее время не существует протоколов и четких рекомендаций по ведению пациентов с послеоперационными забрюшинными гематомами. Проведенный анализ литературы показал, что доказательных исследований по поводу тактики ведения пациентов с забрюшинными гематомами не проводилось, рекомендации основаны чаще всего на описаниях единичных клинических случаев или небольших когортных исследованиях [10]. Как правило, послеоперационные гематомы расположены в зоне оперативного вмешательства, по ходу выделения тазовых структур, возникают в результате ранения кровеносных сосудов. В образовании гематом играет роль метод оперативного вмешательства, ненадлежащий гемостаз, исходное состояние свертывающей системы крови. В зависимости от величины поврежденного сосуда, длительности кровотечения, времени обнаружения, размеры гематом могут варьировать в широком диапазоне. При значительном забрюшинном кровотечении гематома может распространиться вплоть до околопочечной клетчатки.
Диагностика забрюшинных гематом малого таза чаще всего не представляет трудностей: при бимануальном осмотре пальпируется как опухолевидное образование без четких контуров, малоподвижное, эластичной консистенции. Гематомы хорошо визуализируются при ультразвуковом исследовании, компьютерной томографии и магнитно-резонансной томографии. Дополнительное выполнение ангиографии является достаточно важным исследованием в определении тактики лечения [8, 10].
Выбор метода лечения зависит от размеров гематомы, наличия клиники синдрома сдавления соседних органов, выраженности геморрагического синдрома, болевого синдрома, появления признаков инфицирования гематомы. Многие исследователи считают наиболее целесообразной консервативную тактику ведения таких пациентов, особенно на начальном этапе. Таким пациентам проводится инфузионно-трансфузионная, гемостатическая терапия, коррекция коагулопатических нарушений. При выборе оперативного метода лечения предпочтение отдается малоинвазивным способам дренирования. В настоящее время все чаще используется метод селективной эмболизации сосудов таза под рентгенологическим контролем [8–11].
Описание клинического наблюдения
Пациентка 34 лет поступила в плановом порядке на оперативное лечение по поводу пролапса гениталий POP-Q 2-й ст., цистоцеле 2-й ст., ректоцеле 2-й ст., опущение матки 2-й ст. (Aa +1, Ba +1 , C 0, D – 2, Ap 0 , Bp 0 , gh – 4,5, pb – 1, tvl – 9). Из анамнеза: самопроизвольные срочные роды – 2, в 2006 г. – эпизиотомия, в 2012 г. – разрыв промежности 2-й степени. Длительно наблюдалась у врача акушера-гинеколога по месту жительства по поводу рецидивирующих кольпитов, бактериального вагиноза, лечение местными и системными антибактериальными, противовоспалительными препаратами было с кратковременным эффектом, при обследовании на инфекции, передающиеся половым путем обнаружен ВПЧ 16-го типа. Пролапс гениталий диагностирован в 2012 г., проводились попытки консервативной терапии, положительный эффект достигнут не был. Пациентку беспокоила неудовлетворенность в сексуальной жизни, вагинальные звуки во время полового акта, чувство инородного тела, постоянный дискомфорт в области промежности. В связи с этим пациентка была направлена на оперативное лечение. Учитывая репродуктивный возраст, возможное планирование беременности, показаний к использованию сетчатых имплантов не было. Проведенное предоперационное обследование каких-либо отклонений, в том числе со стороны системы гемостаза, не выявило. Выполнено: передняя кольпоррафия, кольпоперинеоррафия, леваторопластика, сакроспинальная цервикопексия слева. Интраоперационно гемостаз достигнут удовлетворительный, устойчивый, осложнений не было. Время операции составило 115 минут, общая кровопотеря – 100 мл.
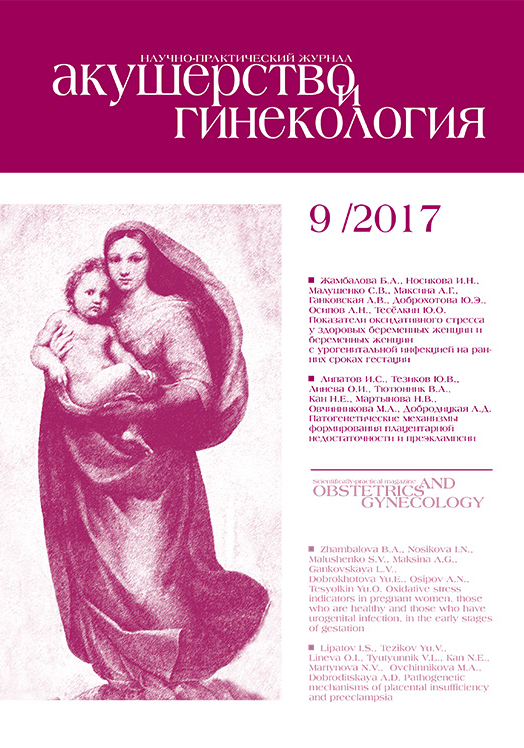
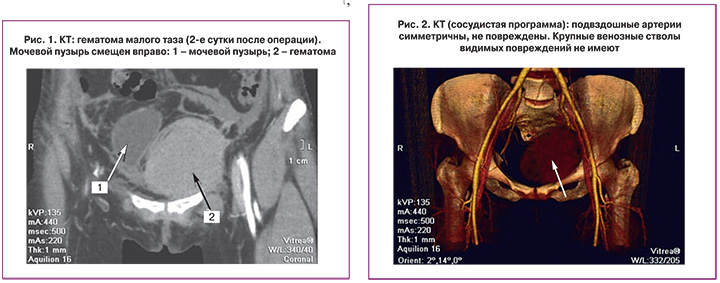
В послеоперационном периоде на 2-е сутки после активизации пациентки внезапно появилась тахикардия до 120 уд./мин, гипотония до 80/50 мм рт. ст., слабость, боль внизу живота. Лабораторные показатели – гемоглобин снизился до 65 г/л, количество эритроцитов до 2,15×1012/л. Срочно было выполнено ультразвуковое исследование, обнаружена забрюшинная гематома: в проекции малого таза неправильной четырехугольной формы неоднородное образование (ан-, гипо-, гиперэхогенное), с четким неровным наружным контуром, отграниченное от окружающих органов и тканей, объемом около 200–233 см3. При ЦДК и ЭДК образование аваскулярно. Пациентка переведена в палату интенсивной терапии, начата инфузионная, гемостатическая терапия. После стабилизации гемодинамических показателей проведена компьютерная томография органов малого таза с трехфазным болюсным контрастированием и ангиографией для определения источника кровотечения. В переднем отделе левой половины малого таза, над m. levator ani, под париетальным листком брюшины определяется образование неправильно-округлой формы с четкими, ровными контурами, изоденсивное крови (63HU-гематома). Размеры образования 65,6×74,9×90,1 мм, приблизительный объем 192,0 см3. Образование имеет недостаточно однородную, слоистую структуру. Передний отдел гематомы расположен над верхней ветвью левой лонной кости, непосредственно под левой прямой мышцей живота. Левый боковой отдел расположен на 7,0 мм медиальнее наружных подвздошных артерии и вены. Верхний и латеральный отделы гематомы оттесняют париетальный листок брюшины, смещают органы таза вправо (рис. 1). В полости малого таза внутрибрюшинных образований не выявлено. Подвздошные артерии симметричны, не повреждены. Крупные венозные стволы видимых повреждений не имеют (рис. 2). Несмотря на смещение мочевого пузыря гематомой вправо, жалоб на нарушение мочеиспускания у пациентки не было.
Принимая во внимание отсутствие признаков нарастания гематомы, а также признаков повреждения крупных сосудистых структур, пациентке продолжена консервативная терапия: гемостатическая (транексамовая кислота 2 г/сут.), инфузионно-трансфузионная терапия (стерофундин 1000 мл, свежезамороженная плазма 440 мл, эритроцитарная взвесь 380 мл). Учитывая эффективность проводимой терапии и стабилизацию гемодинамики у пациентки (АД 109/68 мм рт. ст., частота сердечных сокращений 115 в мин, шоковый индекс Альговера не более 1, стабильные показатели гемоглобина, количество эритроцитов в динамике), отсутствие признаков продолжающегося кровотечения, ненапряженную, ограниченную, без признаков прогрессирования гематому малого таза по данным обследований, было принято решение о продолжении консервативной терапии.
Пациентка находилась в палате интенсивной терапии в течение 2 суток, к лечению дополнительно была назначена антибактериальная терапия (цефтриаксон 2 г/сут. 7 дней, метронидазол 1,5 г/сут. 7 дней), физиотерапия: 2 сеанса криотерапии, 5 сеансов магнитотерапии, 7 сеансов лазеротерапии. Переведена в профильное отделение в стабильном состоянии, лабораторные показатели: гемоглобин – 93 г/л, эритроциты – 3,15×1012/л, лейкоциты – 9,04×109/л, тромбоциты – 236×1012/л.
Пациентка выписана на 10-е сутки после оперативного лечения в удовлетворительном состоянии, размеры гематомы при бимануальном осмотре и по данным ультразвукового исследования оставались прежними.
При контрольном осмотре через 1 и 3 месяца жалоб пациентка не предъявляла, при бимануальном осмотре размеры гематомы уменьшились.
Обсуждение
Данное клиническое наблюдение показывает возможность консервативного лечения послеоперационной забрюшинной гематомы. Тактика лечения изначально была выбрана консервативная в связи с отсутствием признаков повреждения крупных сосудистых структур по данным компьютерной томографии органов малого таза с трехфазным болюсным контрастированием. Следует отметить, что данный метод позволяет достоверно определить локализацию, размеры гематомы, целостность сосудистых структур. Поэтому можно рекомендовать проведение компьютерной томографии с контрастированием пациентам при развитии подобных осложнений.
Стабилизация состояния пациентки на фоне гемостатической, инфузионной терапии, переливания компонентов крови (свежезамороженной плазмы, эритроцитарной взвеси) позволила отказаться от проведения хирургического дренирования гематомы.
Можно предположить, что при отсутствии повреждения крупных сосудов гематома вызывает тампонаду и гемостаз мелких сосудистых структур, а ее раннее открытое опорожнение может привести к нарушению этого тампонирующего эффекта и, как следствие, к повторному кровотечению. Также дренирование гематомы может привести к инфицированию раны через дренажное отверстие. Поэтому выжидательная тактика у пациентов с забрюшинными гематомами при стабилизации гемодинамических показателей и отсутствии признаков продолжающегося кровотечения, на наш взгляд, является наиболее приемлемой.
Заключение
Дальнейшее накопление и обобщение клинического материала будет способствовать разработке практических рекомендаций (лечебно-диагностического алгоритма) по оптимизации тактики ведения пациентов с забрюшинными гематомами таза в послеоперационном периоде.