Пролапс тазовых органов является распространенной патологией у женщин [1, 2]. По данной проблеме было проведено множество исследований, в том числе влияния ассоциаций известных факторов риска, таких как многократные вагинальные роды и старение. Активно проводятся биохимические исследования: выявление перспективных конечных продуктов гликирования, концентрация, экспрессия рецепторов и уровень эстрогенов в крови и в тканях влагалища в зависимости от возраста [3, 4]. Неоспоримым фактом остается то, что с увеличением продолжительности жизни частота пролапса половых органов растет [5]. С учетом роста продолжительности жизни наиболее актуальным является изучение взаимосвязи генитального пролапса с экстрагенитальной патологией. В нескольких исследованиях изучается ассоциация между минеральной плотностью кости (МПК), гипертонической болезнью (ГБ), сахарным диабетом (СД) и генитальным пролапсом [6, 7]. Согласно данным Bohoussou E. et.al., СД обнаружен у 11,6%, а артериальная гипертензия – у 32,5% из 414 пациентов с генитальным пролапсом, но при этом авторы не сообщили о повышении риска развития опущения органов малого таза [8]. Особый интерес вызывают результаты исследования Isik H. et.al., согласно которому ГБ в комбинации с СД значительно увеличивает риск генитального пролапса (р<0,05) [9], что также подтверждается данными, полученными в исследовании Weli H. et.al [10].
Целью нашего исследования является анализ генитального пролапса у пациентов с коморбидной патологией.
Материалы и методы
Исследование проводилось с 2017 по 2019 гг. на базе Клиники БГМУ и ГКБ № 18 г. Уфы. Всего прооперировано 718 пациенток с генитальным пролапсом с оценкой по POP-Q I–IV степени. 62 пациенткам была проведена оценка МПК путем двухэнергетической рентгеновской абсорбциометрии (DXA, Dual Energy X-ray Absorptiometry) с определением T-критерия согласно критериям ВОЗ [11].
Обработка полученных данных проводилась с помощью программного обеспечения STATISTICA 10.0 от компании StatSoft и SPSS17 Statistics 17.0. Для описания центральной тенденции данных предпочтение было отдано медиане (Ме), которая позволяет исключить статистические ошибки, связанные с отсутствием нормального (Гауссова) распределения в выборке, а для выражения меры вариабельности по той же причине использовались квартили (25 и 75). С целью выявления наиболее значимых факторов в развитии пролапса гениталий был применен метод бинарной логистической регрессии.
Результаты
В данной статье была проведена оценка экстрагенитальной патологии и оперативных вмешательств в анамнезе оперируемых женщин.
Пациентки, включенные в исследование, имели в анамнезе преимущественно нарушения со стороны сердечно-сосудистой системы: гипертоническую болезнь (ГБ) I степени – 30 женщин (4,2%), ГБ II степени – 194 пациентки (27,0%), ГБ III степени – 40 пациенток (5,6%), варикозное расширение вен нижних конечностей – 40 пациенток (8,4%). С клинической точки зрения имеющиеся нарушения могут оказывать влияние на кровоток в стенках влагалища, что может усугублять состояние тазового дна. Также 38 (5,3%) пациенток имели в анамнезе СД; так как в предоперационном и послеоперационном периоде не требовались дополнительные методы исследования и лечения, нами отдельно не рассматривались СД I типа (СД I) и СД II типа (СД II).
С помощью метода бинарной логистической регрессии был выделен наиболее значимый фактор в развитии пролапса гениталий. В качестве зависимой переменной выступило наличие генитального пролапса. В качестве независимых (предикторных) переменных в анализ включались наличие ГБ (I, II, III степени), СД, варикозного расширения вен (статистический анализ представлен в табл. 1).
Уравнение регрессии:
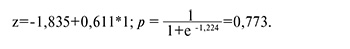
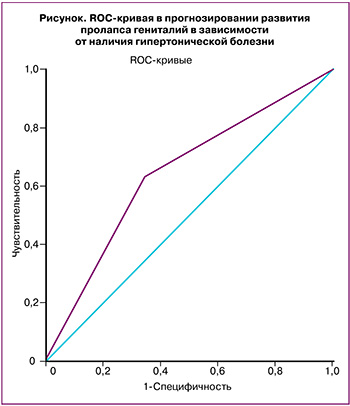 Самым значимым фактором в развитии данной патологии (по данным многофакторного анализа) было признано наличие ГБ, площадь под ROC-кривой составила 0,643±0,05; р=0,012; 95% ДИ 0,535–0,750 (рисунок). СД, ожирение и метаболический синдром в анамнезе имели немного более низкие значения, что не позволило включить их в ряд факторов, достоверно влияющих на развитие данной патологии, это, возможно, требует большего количества наблюдений. Модель не была валидизирована, исследование в данном направлении продолжается.
Самым значимым фактором в развитии данной патологии (по данным многофакторного анализа) было признано наличие ГБ, площадь под ROC-кривой составила 0,643±0,05; р=0,012; 95% ДИ 0,535–0,750 (рисунок). СД, ожирение и метаболический синдром в анамнезе имели немного более низкие значения, что не позволило включить их в ряд факторов, достоверно влияющих на развитие данной патологии, это, возможно, требует большего количества наблюдений. Модель не была валидизирована, исследование в данном направлении продолжается.
Также был проведен анализ анестезиологического пособия. С учетом экстрагенитальной патологии и объема операции были выбраны следующие виды наркоза: тотальная внутривенная анестезия+искусственная вентиляция легких (ИВЛ), спинномозговая анестезия и внутривенная анестезия.
При проведении оперативных вмешательств, как правило, использовалась спинномозговая анестезия, которая не требует дополнительных наркотических препаратов. В 70 (9,7%) случаях проведена тотальная внутривенная анестезия+ИВЛ. С целью снижения повышенной тревожности у 41 пациентки (5,7%) проводилась комбинированная спинномозговая и внутривенная анестезия. Осложнения после наркоза ни в одном случае зарегистрированы не были. Продолжительность операции составила 50,0 (35,0;60,0) минут. Средняя кровопотеря составила 60,0 (56,0;91,0) мл. Послеоперационный период у всех пациентов протекал без особенностей.
Оперативному лечению преимущественно подвергались пациентки старше 49 лет (80,1%). Продолжительность постменопаузы у женщин, участвующих в исследовании, составила 5,0 (3,0;10,0) года, а продолжительность заболевания – 6,0 (4,0; 10,0) года. Таким образом, с учетом этих показателей можно предположить, что пролапс органов малого таза прогрессирует у женщин в постменопаузе.

У 62 пациенток с пролапсом органов малого таза диагностировано нарушение МПК со стороны позвоночника: T-критерий -1,3 в отличие от T-критерия правой бедренной кости -0,44 и T-критерия левой бедренной кости -0,44, что также характерно для женщин в постменопаузе.
Пациентки, включенные в данное исследование, были прооперированы тремя бригадами с целью исключения нарушения техники; проведенные операции представлены в табл. 2.
При постгистерэктомическом пролапсе были выполнены следующие операции: «упрощенная» промонтофиксация, сакроспинальная фиксация, использование сетчатого эндопротеза для реконструкции переднего и апикального отделов тазового дна. Одним из вариантов реконструкции тазового дна предлагалась «упрощенная» промонтофиксация; отличием является то, что при данном оперативном вмешательстве не проводится глубокое рассечение тканей до пуборектальной мышцы и мочевого пузыря. При упрощенной фиксации дистальный конец протеза фиксируется в области купола влагалища U-образно к передней и задней стенкам влагалища, а проксимальный конец – к промонториуму. При предварительной диагностике и исключении нарушения МПК проксимальный отдел протеза фиксируется анкером, который позволяет при несостоятельности связочного аппарата фиксировать протез более плотно к позвонку. Сакроспинальная фиксация использовалась при постгистерэктомическом пролапсе, если длина влагалища была менее 9 см. Сетчатый эндопротез для реконструкции переднего и апикального отделов тазового дна использовался при симптоматическом цистоцеле и при наличии длины влагалища более 9 см, а также в случае отсутствия условий для проведения «упрощенной» промонтофиксации. При наличии шейки матки выполнялась унилатеральная крестцово-остистая фиксация с помощью сетчатого протеза.
Анализ послеоперационного периода выявил наличие одного осложнения через 3 месяца после операции в виде эрозии сетчатого протеза в просвет прямой кишки с последующим удалением импланта трансанально; на 4-е сутки пациентка была выписана в удовлетворительном состоянии.
Обсуждение
В литературе неоднократно освещались такие факторы риска развития пролапса гениталий, как роды, беременность, аборты. Согласно данным McLennan et al., гистерэктомия в анамнезе повышает риск развития генитального пролапса в 1,5 раза [12]. На сегодняшний день нет алгоритма, который мог бы рутинно использоваться в практике для прогнозирования развития генитального пролапса, в том числе у женщин репродуктивного возраста после родов или во время беременности. Одной из нерешенных проблем остается хирургическая коррекция постгистерэктомического пролапса, так как, несмотря на большое количество проводимых операций, многие авторы получают противоречивые результаты при проведении оперативной коррекции данного состояния. Одним из методов коррекции является «упрощенная» промонтофиксация с фиксацией анкером с предварительной диагностикой МПК. Согласно нашему клиническому опыту, при некорригируемой артериальной гипертензии предпочтителен вагинальный доступ в связи с высоким риском осложнений при лапаротомии и лапароскопии с учетом длины влагалища.
Многие авторы оценивали взаимосвязь коморбидных состояний и генитального пролапса. В нашем исследовании ROC-анализ позволил подтвердить гипотезу о влиянии ГБ на увеличение частоты пролапса гениталий (AUC=0,643±0,05, р=0,012); при этом ГБ и СД в совокупности могут увеличивать риски генитального пролапса, что подтверждается данными Weli H., согласно которому именно эти заболевания в совокупности увеличивают риск генитального пролапса в 1,9 раза [10].
Стоит отметить, что наличие в анамнезе СД, ожирения и метаболического синдрома имело немного более низкое значение в прогнозировании пролапса гениталий. Это не позволило включить их в ряд факторов, достоверно влияющих на развитие данной патологии, что, возможно, требует большего количества наблюдений.
Заключение
Возрастное сочетание артериальной гипертензии, СД, метаболического синдрома, снижения МПК и пролапса органов малого таза является актуальной проблемой. Это обусловлено высокой распространенностью данных коморбидных патологий в постменопаузе, а также снижением качества жизни в данной группе пациенток. Требуются дополнительные исследования данной группы заболеваний для определения факторов, влияющих на ухудшение течения этих взаимосвязанных состояний, критериев включения в группы риска, совершенствования методов диагностики и лечения данной коморбидной патологии.