Clinical practice of using T. Vejmovich technique for suture of the uterus after cesarean section
Objective. To improve the outcomes of cesarean section using T. Vejnovic technique for suturing of the uterus after caesarean section.Kabatin N.A., Kalinin V.V., Sorokina A.L.
Materials and methods. The study included 220 women who underwent caesarean section to deliver their babies. They were divided into 3 groups: group 1 – the patients who had ceasarean section with the Pfannenstiel–Kerr technique; group 2 – the patients who had ceasarean section with M.Stark modified technique based on the Joel–Cohen incision; group 3 – the patients who had ceasarean section with M.Stark technique based on the Joel–Cohen incision, using T. Vejnovic modified uterine suture technique. Intraoperative blood loss, operative duration, early postoperaive complications, the presence of an isthmocele 6 months after surgery and residual myometrial thickness were assessed.
Results. The lowest rate of isthmocele formation was 9% (n=5) in group 3, where T.Vejnovic technique was used to restore the uterine wall integrity. The myometrium thickness of 7.9 (0.25) mm in the area of postoperative scar after previous cesarean section was significantly larger compared to group 1 5.6 (1.94) mm (p=0,01), and group 2: 4.7 (2.37) mm (p=0.005).
Conclusion. To preserve the normal thickness of uterine walls during cesarean section, T. Vejnovic modified uterine suture technique proved to be more effective compared to single-row and double-row suturing with no statistically significant differences in reduction in the incidence of isthmocele (niche).
Keywords
The constantly growing number of deliveries by caesarean section in the world leads to the emergence of new pathological conditions and issues to be addressed [1]. One of them is the formation of isthmocele, or niche. An isthmocele, a cesarean section scar defect, or uterine niche, is a triangular defect in the uterine wall with a basis adjacent to the uterine cavity at the site of the previous cesarean section [2]. Isthmocele is diagnosed not earlier than 6 months after surgery by transvaginal echography; however, echohysterography with sterile 0.9% sodium chloride solution is a more sensitive method [3–5]. It is believed that a defect of more than 50% of the thickness of the myometrium is of clinical importance. It is also significant to determine the thickness of the residual myometrium in the area of the previous cesarean section; the critical thickness of less than 2.2 mm may require surgical correction [6–8]. Isthmocele may be associated with an increased risk of obstetric complications: scar insufficiency, placenta praevia, placental ingrowth, uterine rupture, pregnancy in the scar, and also increases the probability of some gynecological complications, such as abnormal uterine bleeding, dysmenorrhea and chronic pelvic pain, secondary infertility [9–15].
The incidence of isthmocele varies within different limits. Finnish researchers report the incidence of isthmocele in 45.6% of cases, and also cite risk factors for the formation of isthmocele, such as repeated prolonged cesarean section, increased body mass index, gestational diabetes mellitus, duration of labor [4]. A recent study by Korean scientists revealed the incidence of isthmocele in 73.8% of cases, as well as factors affecting the risk of ismocele formation: repeated caesarean section, premature rupture of the fetal membranes, shorter operation time, opening of the cervix more than 4 cm. The authors also note that suturing with a single-row or double-row suture did not result in any differences in the frequency of isthmocele formation [16].
One of the main questions is the influence of the suturing method of the uterus wall on the frequency of isthmocele formation. The most common methods of suturing the uterine wall are single-row and double-row technique. A 2017 systematic review and meta-analysis describing 9 randomized controlled trials involving 3969 women showed that one- and two-row sutures are associated with the same frequency of a defect detection in the scar area after cesarean section by ultrasound examination (US), as well as the frequency of scar dehiscence and uterine rupture during subsequent pregnancy. The only difference between a single-layer suture and a two-layer suture is thinner residual myometrium detected on US with a singlerow technique [17]. Many publications in recent years provide evidence that it is not the number of the suture rows that matters, but non-inclusion of the endometrium decidua [18, 19].
In addition to the standard methods of the uterine wall suturing, the technique based on intraoperative shortening of the incision length have been described and used during cesarean section: 1) suture according to Cem Turan; 2) suture according to T. Vejnovic. When using the latter, the reparation of the uterus is based on the natural processes of involution of the uterus after childbirth. Sutures and knots are organized in such a way that the length of the incision on the uterus intraoperatively becomes twice shorter, and the centripetal forces inside the scar contribute to further involution of the uterus and preservation of the thickness of the uterine wall [20, 21]. The peculiarities of the suture technique make it possible to reduce blood loss and reduce the frequency of additional hemostatic sutures due to the effect of myotamponade [21]. There are publications on the successful use of this technique in clinical practice and positive long-term outcomes [22–24]. It is assumed that the use of these techniques, in comparison with conventional methods, will reduce the frequency of isthmocele formation and associated obstetric and gynecological complications.
Thus, the relationship between various methods of suturing the uterus and the prevalence of isthmocele is still unclear.
The aim of this study was to improve the outcomes of caesarean section by using the method of suturing the uterus wall according to T. Vejnovic.
Materials and methods
The study was conducted on the basis of the Perinatal Center of the State Budgetary Healthcare Institution “Borsky Central Regional Hospital” from June 2018 to December 2019. The study included 220 women who gave birth by caesarean section. The key inclusion criterion was the first delivery by cesarean section, the exclusion criterion was pathological intraoperative blood loss ≥1000 ml. The following methods were used to examine the women: 1) physical examination; 2) the history analysis; 3) the volume of blood loss was assessed using the formula according to D. Malcolm intraoperatively: V = P * (Hto-Htk), where: V – blood volume, P – patient's weight, Hto – initial hematocrit before surgery, Htk – hematocrit after surgery; 4) Ultrasound using a Medison Accuvix V10 scanner (South Korea) with a transabdominal probe with a frequency of 3.5 Hz and a transvaginal probe with a frequency of 5 Hz. Ultrasound examination was carried out on the 4–5th day of the postoperative period and repeated not earlier than 6 months after the operation by echohysterography with sterile 0.9% sodium chloride solution.
Caesarean section was performed using various techniques. The choice of the method of caesarean section was carried out randomly. Based on this choice, 3 groups were formed: group 1 included 110 women who were operated using the technique of caesarean section by laparotomy according to Pfannenstiel: the abdominal wall was incised according to Pfannenstiel, the uterus was dissected with a transverse incision in the lower segment with preliminary opening of the plica vesicouterina, the incision on the uterus was sutured with two rows of continuous sutures, uterine serosa and parietal peritoneum were sutured with continuous sutures, the aponeurosis was sutured with a continuous suture, and a continuous intradermal suture was applied to the skin.
Group 2: 55 women were operated using the modified M. Stark technique: the abdominal wall was cut according to Joel–Cohen, the uterus was dissected with a transverse incision in the lower segment without opening the plica vesicouterina, the incision on the uterus was sutured with one raw of a continuous suture, uterine serosa and parietal peritoneum were not sutured, the muscles were not sutured, the aponeurosis was sutured with a continuous suture, and a continuous intradermal suture was applied to the skin.
Group 3 included 55 women operated using a modified M.Stark technique with suturing on the uterine wall using the T. Vejnovic technique.
The groups were comparable in terms of age, clinical and anamnestic data, and the incidence of pregnancy complications. All operations were performed using modern synthetic polymer absorbable suture material.
Description of the method of suturing the uterus according to T. Vejnovic
The T.Vejnovic suture technique includes 4 steps. The first step is suturing the right corner of the wound with a Z-shaped suture with further application of 3-4 Reverden stitches to the middle of the incision. After that, the free ends of the threads are tied causiong the first reduction in the length of the incision. The second step – suturing of the left corner of the wound – is performed similarly to the first step. The third step is Reverden suturing the central part of the incision with further tying together the needles ends. The fourth step – the final reduction in the length of the insicion – the free ends of the threads are tied together (every two ends of each side). A prerequisite for the technique is non-inclusion of absence of the endometrium (decidua) into the suture.
Statistical analysis
All the results of the studies were processed by statistical methods by the Microsoft Excel 2013, STATISTICA v.11, Biostat 2009 Professional version 5.8.4 application package. At the first stage of statistical analysis, the distribution normality was determined using the generalized D'Agostino–Pearson test. Normally distributed data is presented as mean and standard deviation M (SD). Data where the hypothesis of normality is rejected is presented as a median with an interquartile range Me (Q1; Q3). Qualitative data is presented as absolute (n) and relative (%) values. To assess the differences between the compared groups in quantitative variables with normal distribution, the Student's t-test was used, to compare nonparametric data, the Mann–Whitney U-test was used. Fisher's exact test was used to assess differences between groups in terms of qualitative characteristics. Differences between the compared values were considered statistically significant with a probability of error p <0.05, and these statements were regarded as significant.
Results and discussion
The age of women ranged from 18 to 42 years. The average age of the operated patients was 29 (5.2) years. The groups and subgroups were comparable in terms of age, clinical and anamnestic data and complications of pregnancy. In the structure of indications for operative delivery prevailed: fetal hypoxia – 25% (n=55), abnormal labor, including premature rupture of the fetal membranes – 23% (n=51), breech presentation – 15% (n=33). In a smaller percentage of cases, operations were performed for somatic diseases – 7.5% (n=16), preeclampsia – 7.5% (n=16), obstructed labor – 7.5% (n=16), high viral load in HIV infection – 4.5% (n=10). Elective CS was performed in 28.5% (n=63); emergent CS in 71.5% (n=157). All elective SCs (n=63) were performed under regional spinal anesthesia. In emergent CS, total intravenous anesthesia with mechanical ventilation was used in 12% (n=26) of cases.
The average blood loss during operative delivery was 404 (298; 629) ml. In group 1, blood loss was on average 470 (342; 758) ml, which is significantly higher than in group 2 – 333 (292; 426) ml (p=0.018); and in group 3: 320 (255; 387) ml (p=0.028). The smallest average blood loss was noted in the subgroup of women where the uterine suturing was done according to the T. Vejnovic technique, but there was no statistically significant difference with the modified M. Stark technique. However, it should be noted that additional hemostatic sutures when using the T. Vejnovic technique were statistically less often: these were applied in 5.5% (n=3) cases, compared to 21% (n=23) (p=0.04) in a group with two rows sutures and 23.5% (n=13) (p=0.03) in a group with single-row suture with the modified M. Stark method. This observation shows that the suture according to T. Vejnovic is effective in reducing the volume of intraoperative blood loss and use of additional hemostatic sutures due to the implementation of the myotamponade effect described by the author.
The average duration of surgical intervention in group 1 was 39 (6) minutes, which turned out to be statistically significantly higher than in groups 2 and 3, where it amounted to 27 (3.5) minutes (p=0.02). Thus, the use of the M. Stark technique reduces the duration of surgery, and the use of the suture according to the T. Vejnovic technique does not increase this parameter [25].
Laparotomy according to Joel–Cohen, in comparison with laparotomy according to Pffanenstiel, has a number of advantages [25]. This was also confirmed in our study: the duration of the use of anesthesia in the postoperative period in women of groups 2 and 3 was 55 (5) hours, which is statistically significantly less than in group 1: 72 (1.5) hours (p <0.001); was less frequent for over 24 hours after surgery in groups 2 and 3: 5.5% (n=3) and 3.6% (n=2), respectively, compared to group 1: 11% (n=12). Postoperative wounds in women of groups 2 and 3: skin hematomas and seromas were observed in only two cases, that was significantly less (p=0.03) than in the group of women where the skin incision was performed according to Pfannenstiel; skin hematomas in the latter group occurred in 10% (n=11) cases, seromas – 5.5% (n=6) cases.
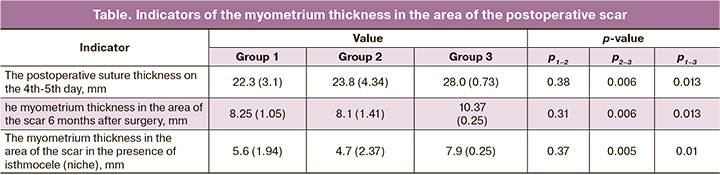
Ultrasound of the thickness of the postoperative uterine scar on the 4–5th day of the postoperative period showed that it was significantly more in the group of women where the T. Vejnovic suturing was used, and amounted to 28 (0.73) mm, compared with the group with double-row suture – 22.3 (3.1) mm (p=0.006); and with the group with a single-row suture – 23.8 (4.34) mm (p=0.01) (Table). The thickness of the area of the postoperative suture did not differ significantly when single-row and double-row sutures were applied. Most important is the ultrasound of the uterine scar, carried out 6 months after surgery, when the main reparative processes in this area were completed [26]. When performing transvaginal echohysterography using sterile 0.9% sodium chloride solution in women who underwent caesarean section, the thickness of the myometrium in the area of the postoperative scar, the presence of an isthmocele (niche) and the thickness of the residual layer of the myometrium were assessed.
The overall incidence of isthmocele in the postoperative scar in the examined women was 18.6% (n=41). In most cases – 95% (n=39) niches had a typical inverted triangle shape. In women with double-row and single-row sutures, the uterine niches were visualized with similar incidence – 21% (n= 23) and 23% (n=13) cases, respectively. The detection of isthmocele (niche) was found in the group of patients with T. Vejnovic technique – 9% (n=5), although this difference was not statistically important. Also noteworthy is the fact that within this group there were no niches with a depth of more than 50% of the thickness of myometrium; in the group of examined patients with a double-row suture, niches more than 50% of the myometrium thickness were visualized in 13% (n=3) cases, in women after single-row suture – in 15% (n=2) cases. These 5 patients were selected for a close follow-up, since such a niche may have clinical significance in the future and require surgical correction before planning the next pregnancy.
The average thickness of the myometrium in the area of the postoperative scar with a two-row suture was 8.25 (1.05) mm, with a single-row suture – 8.1 (1.41) mm, and these data did not have statistically significant differences. In group 3, where T. Vejnovic technique was used, the average value of the thickness of the myometrium in the area of the postoperative scar was 10.37 (0.25) mm, which was statistically higher than in the group of women with a double-row (p=0.01) and a single-row suture (p=0.006) (table). In the presence of a niche in group 1, the thickness of the myometrium in the area of the postoperative scar was 5.6 (1.94) mm in average; in group 2, this value turned out to be minimal, it amounted to 4.7 (2.37) mm, although no statistically significant differences were obtained. Our results confirm the data obtained in a systematic review and meta-analysis by Di Spiezio Sardo (2017) [17] that the only difference between a single-row suture and a two-row suture is the thinner residual myometrium on sonography. We obtained statistically significant thickness of the myometrium in the area of the postoperative scar in the presence of isthmocele in group 3, which amounted to 7.9 (0.25) mm, which was higher than in group 1 – 5.6 (1.94) mm (p=0.01) and in group 2 – 4.7 (2.37) mm (p=0.005), respectively (Table).
Conclusion
Our study demonstrated higher effectiveness of T. Vehnovic technique for preservation of the thickness of the uterine wall after cesarean section in comparison to a single-row or double-row suture without statistically significant differences in reducing the incidence of isthmocele (niche). Despite this, the question of choosing optimal technique for caesarean section remains open.
Our study showed only certain quantitative characteristics of the outcomes of the operation, while the clinical outcomes can be assessed only during the prospective follow-up.
References
- Betrán A.P., Ye J., Moller A.B., Zhang J., Gülmezoglu A.M., Torloni M.R. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016; 11(2): e0148343. https://dx.doi.org/10.1371/journal.pone.0148343.
- Bij de Vaate A.J., Van der Voet L.F., Naji O., Witmer M., Veersema S., Brölmann H.A. et al. Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following cesarean section: systematic review. Ultrasound Obstet. Gynecol. 2014; 43(4): 372-82. https://dx.doi.org/10.1002/uog.13199.
- Regnard C., Nosbusch M., Fellmans C., Benali N., van Rysselberghe M., Barlow P. et al. Cesarean section scar evaluation by saline contrast sonohysterography. Ultrasound Obstet. Gynecol. 2004; 23(3): 289-92. https://dx.doi.org/10.1007/s00404-018-4702-z.
- Antila-Långsjö R., Mäenpää J.U., Huhtala H., Tomás E., Staff S. Comparison of transvaginal ultrasound and saline contrast sonohysterography in evaluation of cesarean scar defect: a prospective cohort study. Acta Obstet. Gynecol. Scand. 2018; 97(9): 1130-6. https://dx.doi.org/10.1111/aogs.13367.
- Приходько А.М., Баев О.Р., Луньков С.С., Еремина О.В., Гус А.И. Возможности методов оценки состояния стенки матки после операции кесарева сечения. Акушерство и гинекология. 2013; 10: 12-6. [Prikhodko A.M.,Bayev O.R., Lunkov S.S., Eremina O.V., Gus A.I. Possibilities of methods for evaluating the uterine wall after cesarean section. Obstetrics and Gynecology. 2013; 10: 12-6. (in Russian)].
- Ofili-Yebovi D., Ben-Nagi J., Sawyer E., Yazbek J., Lee C., Gonzalez J. et al. Deficient lower-segment cesarean section scars: prevalence and risk factors. Ultrasound Obstet. Gynecol. 2008; 31(1): 72-7. https://dx.doi.org/10.1002/uog.5200.
- Osser O.V., Jokubkiene L., Valentin L. High prevalence of defects in cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet. Gynecol. 2009; 34(1): 90-1. https://dx.doi.org/10.1002/uog.6395.
- Marotta M.L., Donnez J., Squifflet J., Jadoul P., Darii N., Donnez O. Laparoscopic repair of post-cesarean section uterine scar defects diagnosed in nonpregnant women. J. Minim. Invasive Gynecol. 2013; 20(3): 386-91.https://dx.doi.org/10.1016/j.jmig.2012.12.006.
- Futyma K., Gałczyński K., Romanek K., Filipczak A., Rechberger T. When and how should we treat cesarean scar defect – isthmocoele? Ginekol. Pol. 2016; 87(9): 664. https://dx.doi.org/10.5603/GP.2016.0063.
- Tulandi T., Cohen A. Emerging manifestations of cesarean scar defect in reproductive-aged women. J. Minim. Invasive Gynecol. 2016; 23(6): 893-902. https://dx.doi.org/10.1016/j.jmig.2016.06.020.
- Van der Voet L.F., Bij de Vaate A.M., Veersema S., Brölmann H.A., Huirne J.A. Long-term complications of caesarean section. The niche in the scar: a prospective cohort study on niche prevalence and its relation to abnormal uterine bleeding. BJOG. 2014; 121(2): 236-44. https://dx.doi.org/10.1111/1471-0528.12542.
- Bij de Vaate A.J., Brölmann H.A., van der Voet L.F., van der Slikke J.W., Veersema S., Huirne J.A. Ultrasound evaluation of the cesarean scar: relation between a niche and postmenstrual spotting. Ultrasound Obstet. Gynecol. 2011; 37(1): 93-9. https://dx.doi.org/10.1002/uog.8864.
- Wang C.B., Chiu W.W., Lee C.Y., Sun Y.L., Lin Y.H., Tseng C.J. Cesarean scar defect: correlation between cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet. Gynecol. 2009; 34(1): 85-9. https://dx.doi.org/10.1002/uog.6405.
- Florio P., Filippeschi M., Moncini I., Marra E., Franchini M., Gubbini G. Hysteroscopic treatment of the cesarean-induced isthmocele in restoring infertility. Curr. Opin. Obstet. Gynecol. 2012; 24(3): 180-6. https://dx.doi.org/10.1097/GCO.0b013e3283521202.
- Gubbini G., Centini G., Nascetti D., Marra E., Moncini I., Bruni L. et al. Surgical hysteroscopic treatment of cesarean-induced isthmocele in restoring fertility: prospective study. J. Minim. Invasive Gynecol. 2011; 18(2): 234-7. https://dx.doi.org/10.1016/j.jmig.2010.10.011.
- Park I., Kim M., Lee H., Gen Y., Kim M. Risk factors for Korean women to develop an isthmocele after a cesarean section. BMC Pregnancy Childbirth. 2018; 18(1): 162. https://dx.doi.org/10.1186/s12884-018-1821-2.
- Di Spiezio Sardo A., Saccone G., McCurdy R., Bujold E., Bifulco G., Berghella V. Risk of Cesarean scar defect following single- vs double-layer uterine closure: systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet. Gynecol. 2017; 50(5): 578-83. https://dx.doi.org/10.1002/uog.17401.
- Yazicioglu F., Gökdogan A., Kelekci S., Aygün M., Savan K. Incomplete healing of the uterine incision after caesarean section: Is it preventable? Eur. J. Obstet. Gynecol. Reprod. Biol. 2006; 124(1): 32-6. https://dx.doi.org/10.1016/j.ejogrb.2005.03.023.
- Roberge S., Bujold E. Closure of uterus and the risk of uterine rupture. BJOG. 2014; 122(11): 1542. https://dx.doi.org/10.1111/1471-0528.13095.
- Turan C., Büyükbayrak E.E., Yilmaz A.O., Karsidag Y.K., Pirimoglu M. Purse-string double-layer closure: A novel technique for repairing the uterine incision during cesarean section. J. Obstet. Gynaecol. Res. 2014; 41(4): 565-74. https://dx.doi.org/10.1111/jog.12593.
- Vejnovic T.R. Cesarean delivery – Vejnovic modification. Srp. Arh. Celok. Lek. 2008; 136(Suppl. 2): 109-15. https://dx.doi.org/10.2298/sarh08s2109v.
- Furau C., Furau G., Dascau V., Ciobanu G., Onel C., Stanescu C. Improvements in cesarean section techniques: Arad's obstetrics department experience on adapting the Vejnovic cesarean section technique. Maedica (Buchar). 2013; 8(3): 256-60.
- Vejnovic T.R., Costa S.D., Ignatov A. New technique for caesarean section. Geburtshilfe Frauenheilkd. 2012; 72(9): 840-5. https://dx.doi.org/10.1055/s-0032-1315347.
- Vejnoviс T., Vejnoviс A. New technique in obstetrics: Vejnovic modification of caesarean section. Is there an impact on the frequency of placenta increta/percreta? Jatros. Medizin fur die Frau. 2016; 3/16: 26-9. Available at: http://ch.universimed.com/files/grafik/Zeitungen_2016/Frau_1603/e-papers/index.html#26/z52
- Dahlke J.D., Mendez-Figueroa H., Rouse D.J., Berghella V., Baxter J.K., Chauhan S.P. Evidence-based surgery for cesarean delivery: an updated systematic review. Am. J. Obstet. Gynecol. 2013; 209(4): 294-306. https://dx.doi.org/10.1016/j.ajog.2005.12.063.
- Naji O., Wynants L., Smith A., Abdallah Y., Stalder C., Sayasneh A. et al. Predicting successful vaginal birth after Cesarean section using a model based on Cesarean scar features examined by transvaginal sonography. Ultrasound Obstet. Gynecol. 2013; 41(6): 672-8. https://dx.doi.org/10.1002/uog.12423.
Received 29.05.2020
Accepted 04.12.2020
About the Authors
Nikolay A. Kabatin, Ph.D., obstetrician-gynecologist of the Department of Obstetrics, Perinatal Center, Borsky Central Regional hospital.Tel.: +7(915)939-22-65. E-mail: onlybones@yandex.ru. ORCID: 0000-0003-4759-9420. 606440, Russia, Bor, Babushkina str., 8.
Vitalii V. Kalinin, Ph.D., Head of the Department of Obstetrics, Perinatal Center, Borsky Central Regional hospital. Tel.: +7(904)784-19-00. E-mail: vikalinin77@mail.ru.
ORCID: 0000-0002-3481-0138. 606440, Russia, Bor, Babushkina str., 8.
Anna L. Sorokina, Head of Perinatal Center, Borsky Central Regional hospital. Tel.: +7(906)354-42-66. E-mail: perenat@crb-bor.ru. ORCID: 0000-0003-3316-1559.
606440, Russia, Bor, Babushkina str., 8.
For citation: Kabatin N.A., Kalinin V.V., Sorokina A.L. Clinical practice of using T. Vejmovich technique for suture of the uterus after cesarean section.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 1: 88-93 (in Russian)
https://dx.doi.org/10.18565/aig.2021.1.88-93