Experience with a modified molded sorbent in the treatment of postpartum endometritis
Objective: To investigate the potential detoxifying effect of an application form of a polyvinylpyrrolidone-modified sorbent in the treatment of postpartum endometritis (PE).Barinov S.V., Lazareva O.V., Tirskaya Yu.I., Kadtsyna T.V., Chulovsky Yu.I., Orlitskaya A.D., Leont'eva N.N., Blauman E.S.
Materials and methods: This retrospective study included 124 post-cesarean section patients with PE. The study group (n=63) received combined treatment including antibiotic therapy in combination with intrauterine administration of an applicative form of a polyvinylpyrrolidone-modified sorbent (VNIITU-1(PVP)). The control group (n=61) received standard antibacterial treatment.
Results: In patients with PE, predominantly cocci were isolated from the uterine cavity, including Enterococcus faecalis (26.6%) and Staphylococcus spp. (21.0%), and Enterococcus faecium (14.5%). Antibiotic resistance of the pathogens reached 53.6–68.3%. Atomic force microscopy and electron microscopy of sorbent rods extracted from the uterine cavity confirmed the high sorption capacity of VNIITU-1(PVP) against microorganisms, regardless of their antibiotic resistance. IR spectroscopy showed the high sorption capacity of the molded sorbent VNIITU-1 (PVP) against proteins and microbial toxins. Following treatment, uterine microflora growth was significantly reduced in the treated group, and the concentrations of IL-1β and TNF-α in the uterine aspirate decreased. The risk of hysterectomy in the study group was 14.5 times lower than in the control group (relative risk 0.069 (95% CI 0.009–0.51)).
Conclusion: Intrauterine use of VNITU-1 (PVP) molded sorbent in the complex therapy of PE improves treatment results and reduces the risk of hysterectomy by 14.5 times.
Authors' contributions: Barinov S.V. – conception and design of the study; Lazareva O.V., Kadtsyna T.V., Orlitskaya A.D., Blauman E.S. – data collection and analysis; Lazareva O.V. – statistical analysis; Tirskaya Yu.I. – manuscript drafting; Leont'eva N.N. – IR-spectroscopy; Chulovsky Yu.I. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Omsk State Medical University, Ministry of Health of Russia (Ref. No. 81 of 26.09.2016).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Barinov S.V., Lazareva O.V., Tirskaya Yu.I., Kadtsyna T.V.,
Chulovsky Yu.I., Orlitskaya A.D., Leont'eva N.N., Blauman E.S.
Experience with a modified molded sorbent in the treatment of postpartum endometritis.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (6): 89-98 (in Russian)
https://dx.doi.org/10.18565/aig.2023.37
Keywords
In the context of the demographic crisis and decline in the reproductive health of the population, it is important to preserve the reproductive function of women. Despite the successes and achievements of modern science over the past 10-15 years, postpartum generalized septic complications remain one of the leading causes of maternal death in Russia and worldwide [1–3].
Among all postpartum infectious complications, postpartum endometritis (PE) is the most common; it also becomes the initial stage in the development of generalized forms of infection [3, 4]. The development of the inflammatory process in the closed space of the postpartum uterus has its own nuances owing to changes in hemodynamics and the presence of blood and lochia. Endotoxins secreted by rapidly multiplying microorganisms rapidly accumulate and end up in the circulating lymph and blood, with a subsequent impact on the immunological response, contributing to the generalization of the process. Currently, general extracorporeal detoxification methods for sepsis have been developed and successfully used, but the feasibility of removing toxins from the focus of inflammation is limited [3, 5].
Another important issue of our time is antibiotic resistance, which is becoming a global concern [6, 7]. Different types of microorganisms develop multiple mechanisms of resistance to different groups of antibacterial drugs and exchange this information. In this regard, the arsenal of therapeutic agents is rapidly diminishing; in fact, no new class of antibiotics has been discovered in the last 30 years [8].
An alternative or addition to antibiotic therapy is the intrauterine application of drugs with high sorption capacity and antibacterial action. The use of medical carbon sorbents makes it possible to influence not only the microorganisms themselves, reducing their number in the focus of inflammation due to mechanical sorption regardless of antibiotic resistance [9, 10], but also to sorb various types of toxins released by pathogens.
This study aimed to investigate the potential detoxifying effect of the application form of a sorbent modified with polyvinylpyrrolidone (VNIITU-1(PVP)) for the treatment of PE.
Materials and methods
This study was conducted at the Department of Gynecology of Omsk Regional Clinical Hospital from 2016 to 2021 and included 124 postpartum women with PE after caesarean section. Postpartum women included in the study were divided into two groups. Patients in the study group (n=63) underwent combined treatment with concomitant antibiotic therapy and the application of the sorbent, VNIITU-1 (PVP), injected into the uterine cavity. The exposure time of the sorbent was 24 h, after which the sorbent was removed from the uterine cavity and a new sorbent was inserted. Sorption therapy was performed for five days.
Postpartum women in the control group (n=61) were administered antibiotic therapy. On admission, broad-spectrum antibiotic therapy was initiated. On day 2, after receiving the culture results, therapy was adjusted according to the susceptibility of the pathogenic bacteria.
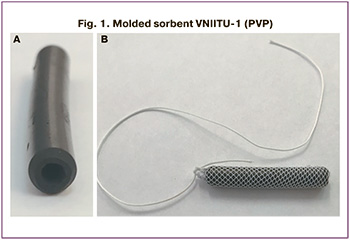
The molded sorbent VNIITU-1 (PVP) has registration certificate no. RZN 2015/2969 (08/14/2015) and was approved for use in the Russian Federation (RF patent No. 2646496). The absence of toxicity was confirmed in Report No. 2099.013P (August 14, 2013). This is nanostructured mesoporous carbon with antiseptic properties. The sorbent is a hollow 40 mm × 5 mm cylinder with rounded edges and an internal circular channel (Fig. 1A). VNIITU-1(PVP) is packed in a mesh nylon shell with a pore size greater than 1 mm. This shell does not prevent penetration of the sorbent. The thread attached to the sorbent is necessary for subsequent removal (Fig. 1B). The sorbent was produced by the Federal Research Center, Boreskov Institute of Catalysis of the Siberian Branch of the Russian Academy of Sciences.
The following instrumental and laboratory tests were used for the clinical evaluation of patients.
1. Pelvic ultrasound examination using a SonoScape SSI-8000 Pro (China) was performed on the 1st day of admission and on the 5th day of treatment. The assessment included anteroposterior size, length, body width, and thickness of the uterine cavity. The uterine volume was calculated using the following formula: V=1/6π×L×H×B, where L is the length of the uterine body, H is the anteroposterior size of the uterus, and B is the uterine body width.
2. Hysteroscopy was performed on all patients on the first day of admission by using an OLIMPUS A4760 hysteroscope (Japan).
3. Microbiological examination: on day 1, before the start of empirical antibiotic therapy, the contents of the uterine cavity were collected, avoiding contact with the vaginal and cervical flora. A contamination level of 102–9×103 CFU/ml was regarded as low, 104–9×104 CFU/ml as average, and a high degree corresponded to the growth of microorganisms in the amount of 105–9×105 CFU/ml. Sensitivity was determined using the standard disk diffusion test.
4. Immunological studies were performed at baseline and on day 5 of therapy and included measurements of the levels of the anti-inflammatory cytokines interleukin-10 (IL-10), tumor necrosis factor-alpha (TNF-α), and interleukin-1β (IL-1β) in uterine cavity aspirate (Vector-best, Novosibirsk).
5. Atomic force microscopy (AFM) of the sorbent rod (n=3) after its removal from the uterine cavity was performed to confirm its sorption capacity (Vektor, Novosibirsk).
6. Electron microscopy (EM) was used to study swabs from the sorbent (n=2) after removal from the uterine cavity (Vektor, Novosibirsk).
7. Infrared (IR) spectroscopy (IRPrestige-21 spectrometer from Shimadzu) was performed at a resolution of 4 cm-1 in the range of 350–7800 cm-1, with a spectrum accumulation number of 50. The sample was prepared by the sedimentation of fine particles deposited with a very thin layer on a BaF2 plate in a glass cylinder. Initially, for 2–3 min, sedimentation of large particles was performed by blowing small portions of carbon material through a hole in the upper part of the cylinder. The deposition of the fine particles took approximately 1 h. To obtain a layer of desired thickness, the entire procedure was repeated seven times. The spectra were processed (baseline correction and smoothing) using ORIGIN software package.
The effectiveness of PE treatment was assessed based on the number of hysterectomies performed in the study groups.
Statistical analysis
Statistical analysis was performed using STATISTICA 10.0. The normality of the distribution was tested using the Shapiro–Wilk test, which showed a non-normal distribution of the study data. Therefore, non-parametric the Mann–Whitney test was used to compare two independent groups; for small groups, Fisher's exact test was used (relative indicators). To calculate the differences between the groups, the χ2 test was used for categorical outcomes. Quantitative variables are presented as the median (Me) with interquartile range (Q1; Q3), therapy outcomes are expressed as binary values, and effect size is calculated using the risk difference with a 95% confidence interval (CI).
This study was conducted in accordance with the 1964 Declaration of Helsinki of the World Medical Association (amended in 2008). The study was reviewed and approved by the Research Ethics Committee of Omsk State Medical University (Ref. No. 81 of 26.09.2016).
Results
In the study patients, chronic iron-deficiency anemia 91/124 (73.4%) was the most common. During pregnancy, 7/124 (5.7%) patients had an acute respiratory infection complicated by pneumonia in 2/124 (1.6 %) women. Acute vaginitis was diagnosed in the of 42/124 (34%) pregnant women. The most common chronic inflammatory disease was chronic bronchitis (15/124 (12.1%)), followed by chronic inflammatory diseases of the urinary tract (8/124 (6.5%)); 3/124 (2.4%) pregnant women had chronic tonsillitis.
This study included patients with PE after caesarean section. The analysis of the indications for operative delivery showed that surgical intervention was most often performed for urgent indications. The most common (32/124 (25.8%)) were labor activity anomalies followed by clinically narrow pelvis (28/124 (22.6%)); the third (21/124 (16.9%)) was progressive fetal hypoxia during childbirth. Severe preeclampsia was an indication for caesarean section in of 11/124 (8.9%) pregnant women. The remaining 32/124 (25.8%) women underwent surgical delivery because of uterine scars after a previous caesarean section.
Endometritis was most frequently diagnosed 10 days after delivery (53/124 (42.7%)). On days 6–10, 39/124 (31.5%) women were diagnosed with the disease. On days 1–5 postpartum, 32/124 (25.8%) women were admitted to the hospital. The main complaint (94/124 (75.8%)) on admission was an increase in body temperature, with subfebrile in 26/124 (21.0%) and febrile in 68/124 (54.8%) patients.
Lower abdominal pain was reported by 105/124 (84.7%) patients. One-third (40/124 (32.3%)) complained of purulent vaginal discharge. Only 8/124 (6.5%) admitted patients complained of profuse, bloody discharge (Table 1).
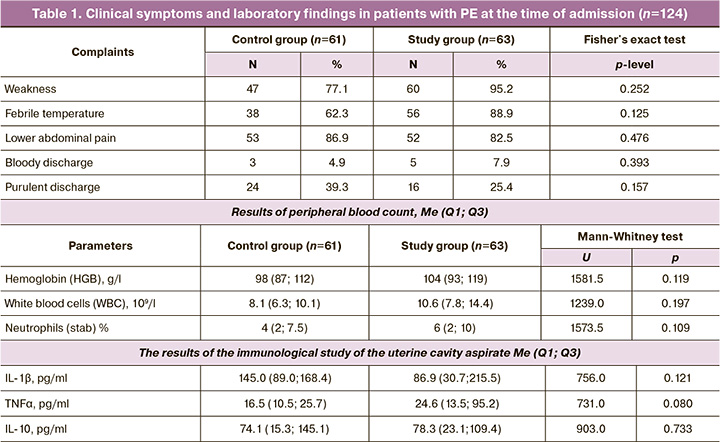
Laboratory findings on admission (general blood count and cytokine levels in the uterine cavity aspirate) did not differ between the study groups (Table 1).
The results of the culture study showed that Enterococcus faecalis dominated (33/124 (26.6%)) in uterine cavity cultures from patients with PE, followed by Staphylococcus spp. (26/124 (21.0%)), Enterococcus faecium (18/124 (14.5%)) ranked third in frequency, and Escherichia coli was isolated in 12/124 (9.7%) postpartum women. Corynebacterium spp. was detected in 6/124 (4.8%) postpartum women and Acinetobacter baumannii in 4/124 (3.2%). The remaining pathogens (Peptostreptococcus spp., Propionibacterium spp., Proteus vulgaris, Klebsiella pneumoniae, and Streptococcus spp.) were detected in less than 1% of the cases. Symbiosis of several pathogens was observed in 50/124 (40.3%) cultures. The most frequent associations of microorganisms were Enterococcus faecalis. In 7/33 (21.2%) patients they were combined with Staphylococcus spp., in 5/33 (15.2%) with Escherichia coli, and in 4/33 (12.1%) with Enterococcus faecium.
The results showed that Enterococcus faecalis was resistant to antibiotics in 18/33 (54.5%) cases, while in 4/33 (12.1%) cases, it was resistant to more than three antibiotics simultaneously. Enterococcus faecium was resistant in 10/18 (55.6%) cases; in 4/18 (22.2%) of the cultures, resistance to more than three antibiotics was detected. The Staphylococcus spp. group was resistant to antibiotics in 15/26 (57.7%) cases, with 9/26 (34.6%) cases resistant to three or more antibiotics from different pharmacological groups. E. coli showed resistance in 9/12 (75.0%) of the cultures, in 3/12 (25.0%) it was resistant to three antimicrobials. Acinetobacter baumannii was resistant to antibiotics in 2/4 (50%) cases and to four drugs in 3/4 (75%) cases.
On admission, all women underwent diagnostic hysteroscopy. Analysis of the results showed that the most frequent (43/124 (34.7%)) were blood clots in the placental site and suture edema in 32/124 (25.8%). Decidual tissue necrosis was visualized in 25/124 (20.2%) women; in 8/124 (6.6%), ligatures hanging freely in the uterine cavity and suture defects in the form of funnel-shaped retraction were diagnosed in 5/124 (4.0%) cases.
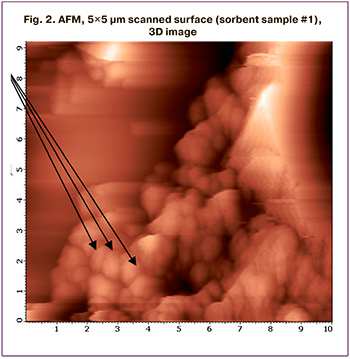
To assess the sorption capacity of VNIITU-1 (PVP), AFM analysis of the sorbent rod was performed after its 24-hour exposure in the uterine cavity (n=3). AFM was also used in parts of the sorbent that were previously destroyed. Examination of sample #1 showed that the entire surface of the sorbent was covered with a biomaterial in the form of an organic film consisting of round-shaped microorganisms. The presence of coccus microflora is shown in the images (Fig. 2). Preliminary culture of this sorbent revealed massive growth of Enterococcus faecalis. Microorganisms, mainly bacilliform, were detected on the surface of sorbent no. 2. The culture from sorbent sample #2 showed massive growth of Escherichia coli.
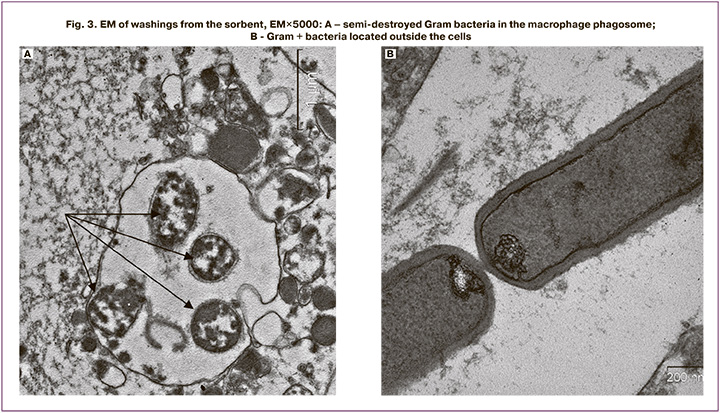
To clarify the composition of the cellular debris present on the surface of the sorbent, EM was performed on washes of VNIITU-1(PVP) after its extraction from the uterine cavity (n=2). Epithelial cells and neutrophils with varying degrees of maturity were mainly present on the slides. Granulocytes (eosinophils and basophils) were much less frequent. No lymphocytes were detected. Neutrophil phagosomes contained whole or half-destructed bacteria (Fig. 3A). A significant number of microorganisms were also found in the preparations, either individually or in groups, mainly Gram+ bacilli, without signs of destruction, and fission patterns were also observed (Fig. 3B).
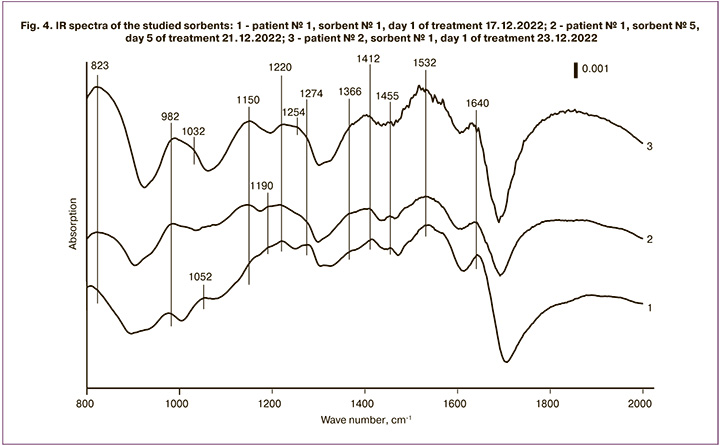
To determine the detoxification capacity of the VNIITU-1(PVP)-molded sorbent, IR spectroscopy was performed on the carbon material after extraction from the uterine cavity after 24 h of exposure (Fig. 4). When the samples were examined in the spectral region of 1500–1600 cm-1 at 1536 cm-1, an intense broad absorption band was observed, which corresponded to the valence vibrations of C=C bonds in condensed aromatic compounds. The appearance of an absorption band in the spectral region of 1000–1200 cm-1 indicated the presence of valent vibrations of the C=O bonds in the alcoholic and phenolic substrates. The absorption band corresponding to the vibrations of C=O bonds in phenol esters and lactones was detected in the 1200–1300 cm-1 spectral region. The presence of an absorption band at 1350–1480 cm-1 in the spectrum is characteristic of the C=H bonds in the-CH2- and -CH3- structures. The valence vibrations of the C=O bonds in amides (proteins and polypeptides) were recorded in the spectrum of 1610–1700 cm-1; these structures were conjugated to the aromatic ring in carboxylic acids, ketones, and esters. The results obtained indicate the high capacity of VNIITU-1(PVP) to sorb protein structures of high, medium, and low molecular weights.
The efficacy of the treatment in the study groups was assessed by studying laboratory blood values, cytokine levels in uterine cavity aspirates, determination of uterine cavity contamination, and postpartum uterine involution according to ultrasound examination (Table 2).
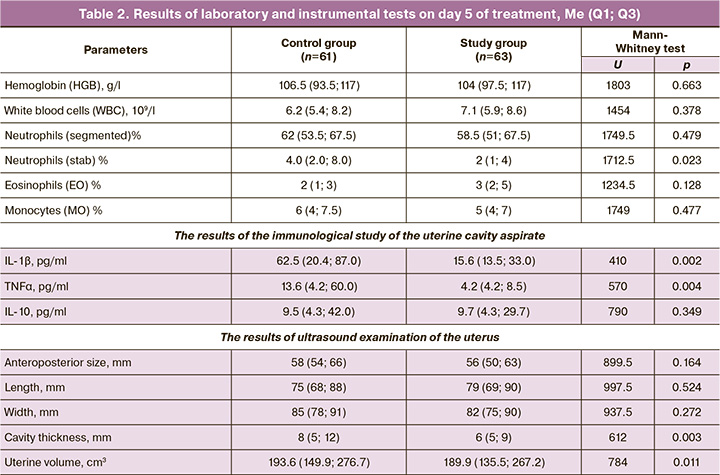
The control results of peripheral blood parameters in women with PE on the fifth day of therapy showed similar positive dynamics in both the groups. Significant differences were observed in the concentrations of pro-inflammatory cytokines in the aspirate from the uterine cavity. Thus, TNFα and IL-1β concentration were 3.2 and 4 times higher in the control group than in the study group. The ultrasound scan performed on day 5 showed positive uterine size involution in all groups. However, in the combined treatment group, total uterine volume and uterine cavity thickness decreased more rapidly (Table 2).
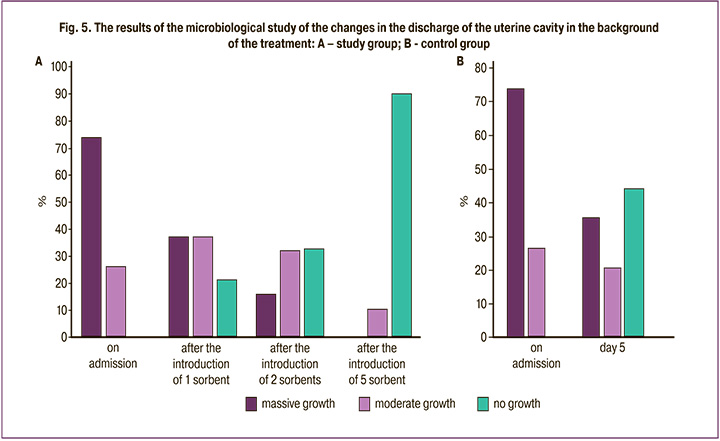
On day 5 of treatment, the results of uterine cavity culture on day 5 of treatment showed that in the treatment group 56/63 (88,9%) of cases had no microbial growth, while 7/63 (11,1%) showed moderate growth of microorganisms. In the control group, 22/61 (36.1%) postpartum women were found to be highly contaminated and 13/61 (21.3%) were moderately contaminated (Fig. 5).
Summing up the results of the treatment, we established that in the control group, 14/61 (22.9%) patients underwent hysterectomy because of treatment failure and progression of the inflammatory process, whereas in the study group, only one patient required hysterectomy (2=10.494, р0.05). Considering treatment outcomes, the clinical effect size was calculated using the risk difference. The relative risk was 0.069 (95% CI 0.009-0.51), that is, the risk of hysterectomy was 14.5 times lower in the study group than in the control group.
Discussion
Postpartum septic complications remain a pressing and unresolved problem in obstetrics. They are associated with increased resistance of pathogens to antibiotics, deterioration of the somatic health of pregnant and postpartum women, the risk of generalization of the infectious process, possible loss of the uterus, making childbirth impossible, and leading to abnormal anatomical and functional relationships between the pelvic organs, as well as neurovegetative and hormonal disorders, with a corresponding deterioration in the quality of life of patients. Therefore, preserving the uterus is one of the prerequisites for providing medical care to women of reproductive age [11–13].
According to the literature, Gram-positive anaerobic (enterococci, group B streptococci, staphylococci) and aerobic (Peptococcus and Peptostreptococcus species) cocci flora and aerobic Gram-negative bacilli (E. coli, Klebsiella pneumonia) dominate among the causative agents of PE [14, 15].
Our findings are consistent with those in the literature and suggest a predominance of cocci flora (Enterococcus faecalis (26.6%), Staphylococcus spp. (21.0%), Enterococcus faecium (14.5%), and Gram-negative E. coli (9.7%) in patients with PE. Associations of several microorganisms isolated from the uterine cavity occurred in 40.3% of the cultures. The antibiotic resistance of the identified flora reached 53.6–68.3%.
AFM and EM analyses of the sorbent rods extracted after 24 h from the uterine cavity of patients with PE confirmed the high sorption capacity of VNIITU-1 (PVP). All microorganisms, irrespective of their antibiotic resistance, and cellular detritus underwent sorption.
The surface of the molded sorbent was impregnated with a PVP monomer solution with subsequent polymerization (the rod surface contained at least 5% PVP). PVP contains a lactam ring in its composition and therefore has an antibacterial effect on pathogenic microflora, similar to that of (VNIITU-1(PVP))-lactam antibiotics. However, unlike β-lactam antibiotics, PVP contains a γ-lactam ring, which makes it impossible to enzymatically attack pathogens capable of producing β-lactamases.
Moreover, studies using physicochemical methods have shown that in contact with a biological medium, PVP migrates (desorbs) from the sorbent surface as polymer chains into the external environment and can independently interact with bacterial cells [16, 17].
Pathogenic microorganisms release biologically active substances, exotoxins, into the external environment. At the moment of death, when the cell wall is destroyed, endotoxins are released, the mechanism of action of which disrupts vital cellular processes (blocking protein synthesis, increasing membrane permeability, and transporting substances). This exacerbates the inflammatory process [18]. According to their chemical structure, bacterial toxins are proteins. IR spectroscopy demonstrated the high sorption capacity of the VNIITU-1 (PVP) molded sorbent with respect to protein structure.
Our study showed the high efficacy of combined treatment with VNIITU-1 (PVP) in the treatment of patients with PE in comparison with traditional treatment because of the sorbent's ability to eliminate pathogens, regardless of their antibiotic resistance, in addition to bactericidal properties of PVP, and the ability to absorb bacterial toxins. Thus, on day 5 of treatment, the concentration of stab neutrophils in peripheral blood was two times lower in the study group than in the control group (p<0,05). The concentration of the proinflammatory cytokines TNFα and IL-1β in uterine secretion was also 3.2 and 4 times lower in the study group (p<0.05). The results of the ultrasound examination suggested that uterine involution was faster in patients treated with combination therapy (p=0.011) during the first five days of treatment. The presence of a marked difference in the degree of uterine cavity contamination in the patients on day 5 of treatment also indicated greater efficacy of the combined PE treatment using the VNIITU-1 (PVP) molded sorbent.
The persistence of pathogenic microflora in the uterine cavity in the control group (massive growth in 36.1% of women and moderate growth in 21.3%) maintained the inflammatory process, which was manifested by a high concentration of pro-inflammatory cytokines (IL-1β and TNFα) and corresponding peripheral blood neutrophil leukocytosis on day 5 of conventional antibiotic therapy, creating a high risk of generalization of the infection process, which required hysterectomy in of 14/61 women (22.9%).
Calculation of the risk difference showed that the combined approach to the treatment of patients with PE reduced the risk of organ failure by 14.5-fold.
Conclusion
The combined approach to PE treatment using intrauterine administration of the VNIITU-1 (PVP) molded sorbent improved treatment results and reduced the risk of hysterectomies by 14.5-fold. VNIITU-1 (PVP) promotes the complete elimination of pathogenic microorganisms due to their sorption onto the sorbent surface, with simultaneous sorption of their life products and decay (exo- and endotoxins). All of these factors reduce the burden on the organism and immune defense factors, prevent the release of toxins to the periphery, and reduce the risk of generalization of the process.
References
- Pavoković D., Cerovac A., Ljuca D., Habek D. Post-cesarean peritonitis caused by hysterorrhaphy dehiscence with puerperal acute abdomen syndrome. Z. Geburtshilfe Neonatol. 2020; 224(6): 374-6.https://dx.doi.org/10.1055/a-1203-0983.
- Bonet M., Nogueira Pileggi V., J Rijken M., Coomarasamy A., Lissauer D., Paulo Souza J. et al. Towards a consensus definition of maternal sepsis: results of a systematic review and expert consultation. Reprod. Health. 2017; 14(1): 67. https://dx.doi.org/10.1186/s12978-017-0321-6.
- Faure K., Dessein R., Vanderstichele S., Subtil D. Postpartum endometritis: CNGOF and SPILF pelvic inflammatory diseases guidelines. Gynecol. Obstet. Fertil. Senol. 2019; 47(5): 442-50. (in French). https://dx.doi.org/10.1016/j.gofs.2019.03.013.
- Conroy K., Koenig A.F., Yu Y.H., Courtney A., Joong Lee H., Norwitz E.R. Infectious morbidity after cesarean delivery: 10 strategies to reduce risk. Rev. Obstet. Gynecol. 2012; 5(2): 69-77.
- Axelsson D., Brynhildsen J., Blomberg M. Postpartum infection in relation to maternal characteristics, obstetric interventions and complications. J. Perinat. Med. 2018; 46(3): 271-8. https://dx.doi.org/10.1515 / jpm-2016-0389.
- Versporten A., Bruyndonckx R., Adriaenssens N., Hens N., Monnet D.L., Molenberghs G. et al. Consumption of cephalosporins in the community, European Union/European economic area, 1997-2017. J. Antimicrob. Chemother. 2021; 76(12, Suppl. 2): ii22-ii29. https://dx.doi.org/10.1093/jac/dkab174.
- Martínez-Martínez L., Calvo J. The growing problem of antibiotic resistance in clinically relevant Gram-negative bacteria: current situation. Enferm. Infecc. Microbiol. Clin. 2010; 28(Suppl. 2): 25-31. (in Spanish).https://dx.doi.org/10.1016/S0213-005X(10)70027-6.
- Кузьмин В.Н. Антибиотикорезистентность как эпидемиологическая проблема инфекционно-воспалительных заболеваний в современных условиях. Медицинский оппонент. 2020; 3: 20-6. [Kuz'min V.N. Antibiotic resistance as an epidemiological problem of infectious and inflammatory diseases in modern conditions. Medical Opponent. 2020; (3): 20-6. (in Russian)].
- Barinov S.V., Tirskaya Y.I., Borisova A.B., Pyanova L.G., Di Renzo G.C. The effectiveness of using a molded sorbent: modified polyvinylpyrrolidone for the combined treatment of chronic endometritis. Int. J. Gynaecol. Obstet. 2021; 154(2): 277-84. https://dx.doi.org/10.1002/ijgo.13609.
- Баринов С.В., Блауман Е.С., Лазарева О.В., Долгих В.Т., Попова Л.Д., Новиков Д.Г., Пьянова Л.Г. Новый метод лечения больных с послеродовым эндометритом. Российский вестник акушера-гинеколога. 2019; 19(4): 65-71. [Barinov S.V., Blauman E.S., Lazareva O.V., Dolgikh V.T., Popova L.D., Novikov D.G., Pyanova L.G. A new method of treatment of patients with postpartum endometritis. Russian Bulletin of Obstetrician-Gynecologist. 2019; 19 (4): 65-71. (in Russian)]. https://dx.doi.org/10.17116/rosakush20191904165.
- Malmir M., Boroojerdi N.A., Masoumi S.Z., Parsa P. Factors affecting postpartum infection: a systematic review. Infect. Disord. Drug Targets. 2022; 22(3): e291121198367. https://dx.doi.org/10.2174/1871526521666211129100519.
- Woodd S.L., Montoya A., Barreix M., Pi L., Calvert C., Rehman A.M. et al. Incidence of maternal peripartum infection: a systematic review and meta-analysis. PLoS Med. 2019; 16(12): e1002984. https://dx.doi.org/10.1371/journal.pmed.1002984.
- Barinov S.V., Tirskaya Y.I., Kadsyna T.V., Lazareva O.V., Medyannikova I.V.,Tshulovski Yu.I. Pregnancy and delivery in women with a high risk of infection in pregnancy. J. Matern. Fetal Neonatal Med. 2022; 35(11): 2122-7.https://dx.doi.org/10.1080/14767058.2020.1781810.
- Кузнецова Д.Е., Макаренко Т.А., Аверчук Е.С. Особенности микробного пейзажа в очаге воспаления при послеродовых гнойно-воспалительных заболеваниях (обзор литературы). Проблемы репродукции. 2021; 27(2): 101-7. [Kuznetsova D.E., Makarenko T.A., Averchuk E.S. Features of the microbial landscape in the focus of inflammation in postpartum purulent-inflammatory diseases (literature review). Human Reproduction. 2021; 27(2): 101-7. (in Russian)]. https://dx.doi.org/10.17116/repro202127021101.
- Greer O., Shah N.M., Sriskandan S., Johnson M.R. Sepsis: precision-based medicine for pregnancy and the puerperium. Int. J. Mol. Sci. 2019; 20(21): 5388. https://dx.doi.org/10.3390/ijms20215388.
- Долгих В.Т., Долгих В.Т., Пьянова Л.Г. Антимикробная активность гранулированных углеродных сорбентов. Российский иммунологический журнал. 2014; 8(3): 788-91. [Dolgikh V.T., Dolgikh V.T., P'yanova L.G. Antimicrobial activity of granular carbon sorbents. Russian Journal of Immunology. 2014; 8(3): 788-91. (in Russian)].
- Бакланова О.Н., Пьянова Л.Г., Талзи В.П. Модифицирование поверхности углеродного сорбента поли-N-винилпирролидоном для аппликационной медицины. Физикохимия поверхности и защита материалов. 2012; 48(4): 363-9. [Baklanova O.N., P'yanova L.G., Talzi V.P. Surface modification of carbon sorbent with poly-N-vinylpyrrolidone for application medicine. Physical Сhemistry of the Surface and Protection of Materials. 2012; 48(4): 363-9.(in Russian)].
- Karsnitz D.B. Puerperal infections of the genital tract: a clinical review. J. Midwifery Womens Health. 2013; 58(6): 632-42. https://dx.doi.org/10.1111/jmwh.12119.
Received 08.02.2023
Accepted 19.04.2023
About the Authors
Sergey V. Barinov, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia, +7(913)633-80-48, barinov_omsk@mail.ru, https://orcid.org/0000-0002-0357-7097, 644099, Russia, Omsk, Lenin’s str., 12.Oksana V. Lazareva, PhD, Associate Professor, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia,
+7(905)484-66-99, lazow@mail.ru, https://orcid.org/0000-0002-0895-4066, 644099, Russia, Omsk, Lenin’s str., 12.
Yuliya I. Tirskaya, Dr. Med. Sci., Associate Professor, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia, +7(913)145-28-17, yulia.tirskaya@yandex.ru, https://orcid.org/0000-0001-5365-7119, 644099, Russia, Omsk, Lenin’s str., 12.
Tat’yana V. Kadtsyna, PhD, Associate Professor, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia,
+7(929)368-08-15, tatianavlad@list.ru, https://orcid.org/0000-0002-0348-5985, 644099, Russia, Omsk, Lenin’s str., 12.
Yuriy I. Chulovsky, PhD, Associate Professor, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia,
+7(913)637-18-11, akusheromsk@rambler.ru, 644099, Russia, Omsk, Lenin’s str., 12.
Anastasiya D. Orlitskaya, Assistant, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia, +7(962)050-64-60, orlitskayaad@mail.ru, https://orcid.org/0000-0002-1641-0720, 644099, Russia, Omsk, Lenin’s str., 12.
Natal’ya N. Leont’eva, PhD (Chemistry), Deputy Director for Science, Center of New Chemical Technologies BIC, +7(3812)67-26-16, science@ihcp.ru,
https://orcid.org/0000-0001-5887-5860, 644040, Russia, Omsk, Neftezavodskaya str., 54.
Ekaterina S. Blauman, graduate student, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia, +7(908)809-68-78, blauman-es@yandex.ru, https://orcid.org/0000-0002-1498-0578, 644099, Russia, Omsk, Lenin’s str., 12.
Corresponding author: Yuliya I. Tirskaya, yulia.tirskaya@yandex.ru