Отсутствие универсальных критериев оценки эффективности лечения глубокого инфильтративного эндометриоза (ГИЭ) затрудняет анализ исходов при различных объемах проведенного оперативного вмешательства.
При оценке тяжести ГИЭ традиционно проводится анализ выраженности болевого синдрома. Однако такой подход не позволяет полноценно оценить тяжесть бремени заболевания для каждого отдельного пациента, т.к. не учитывает влияние бесплодия на жизнь пациента. При лечении больных с ГИЭ рационально использовать показатель оценки качества жизни (КЖ) как критерий, характеризующий заболевание.
КЖ, связанное со здоровьем (health related quality of life, HRQL), – это интегральная характеристика физического, психологического, социального и эмоционального состояния пациента, оцениваемая исходя из его субъективного восприятия, позволяющая дать оценку параметров, ассоциированных и не ассоциированных заболеванием, и дифференцированно определить влияние болезни и лечения на состояние пациента.
Основные инструменты для изучения КЖ – это стандартизированные опросники (индексы и профили), составленные с помощью психометрических методов. Опросники для изучения КЖ можно разделить на две большие группы – общие и специфические.
Наиболее распространенным из общих опросников является SF-36 [1]. Этот опросник наиболее часто применяется в странах Европы, Азии и США для оценки качества жизни, валидирован в РФ [2] и является эффективным инструментом для оценки КЖ женщин с ГИЭ [3].
Исследованию КЖ женщин с ГИЭ посвящено большое количество исследований. Доказано, что женщины с ГИЭ имеют более низкие показатели как физического, так и психического компонентов КЖ по сравнению со здоровой популяцией, и чаще испытывают тревогу и симптомы депрессии, то есть более подвержены психологическому стрессу [4–7].
При этом наиболее значимым фактором снижения КЖ является наличие болевого синдрома. При этом наличие дисменореи оказывает значительное влияние только на физический компонент КЖ, в то время как хроническая тазовая боль влияет на все компоненты [8, 9].
Женщины с более высоким уровнем болевых ощущений закономерно демонстрируют более низкие показатели КЖ [10]. Данные о восприятии хронической тазовой боли (ХТБ) женщинами с эндометриозом и другими заболеваниями противоречивы. Одни авторы утверждают, что женщины с болевой формой эндометриоза демонстрируют более низкие показатели КЖ, чем женщины с ХТБ той же интенсивности при ряде других нозологий [11, 12], другие авторы не находят различий в показателях КЖ женщин с ХТБ различной этиологии [13–15].
Для пациенток с эндометриозом характерно модифицированное восприятие боли, которое независимо от ее интенсивности приводит к более выраженным психологическим изменениям (психологическому стрессу) и потенцирует снижение как физического, так и психического компонента КЖ [16, 17].
Было доказано, что боль, кроме прямого влияния на физический компонент КЖ [18], опосредованно через потенцируемый модифицированным восприятием боли психологический стресс оказывает опосредованное отрицательное действие на психологический компонент КЖ [10], т.е. потенциирует психологический стресс. Таким образом, боль и стресс взаимопотенциируют друг друга, приводя к стойким нарушениям иммунного ответа, нервной и эндокринной регуляции и образованию порочного круга [19].
Известно, что уровень психологического стресса во многом определяется способностью к регуляции эмоций [20–22]. Низкая способность к регуляции эмоций может потенцировать психологический стресс, который, в свою очередь, модифицирует и усиливает болевое восприятие [22, 23]. Хроническое болевое раздражение как основа для хронического стресса истощает нервную систему, приводя к поведенческим изменением и аффективным расстройствам [24]. Таким образом, образуется второй порочный круг.
Психологический стресс дополняется бесплодием как значимым и порой недооцененным социальным аспектом жизни женщины. Бесплодие, приводя к фрустрации, которая в свою очередь приводит к депрессии, снижению самооценки, чувству вины и тревоги, изменению поведенческих реакций и эмоционального фона, еще больше усугубляет психологический стресс [25], увеличивающийся с длительностью бесплодия и по мере применения лечебных процедур [26], что в равной степени касается обоих супругов [27, 28]
С другой стороны, психологический стресс потенцирует бесплодие, таким образом создает дополнительный порочный круг, хоть и не является единственным достаточным фактором [29].
Хирургическое иссечение очагов ГИЭ в значительной степени улучшает КЖ [30] вне зависимости от наличия осложнений течения послеоперационного периода [30, 31] и выведения колостомы [32], однако не приводит к значимому результату при малых формах эндометриоза [33]. У пациенток c более низкими показателями качества жизни наблюдается наиболее значительное улучшение КЖ в послеоперационном периоде [2], что может служить индикатором для отбора пациенток для хирургического лечения и прогнозирования результатов лечения [33].
С целью выработки оптимальной клинической тактики значительный интерес вызывает изучение взаимосвязи КЖ с клиническими проявлениями, локализацией очагов ГИЭ и объемом оперативного лечения, возрастом пациентки, противорецидивной терапией, наличием бесплодия и другими важными аспектами заболевания. Однако опубликовано ограниченное количество научных работ, оценивающих весь спектр. Положительное влияние оперативного лечения колоректального эндометриоза на качество жизни сохраняется даже при длительном (до 4-х лет) послеоперационном наблюдении [34].
Таким образом, именно оценка КЖ является полноценным отражением всех проявлений и особенностей течения заболевания, выявляет изменения состояния пациентки под воздействием различных методов лечения и позволяет сравнить результаты, полученные при применении различных методов. Кроме того, оценка КЖ может служить инструментом для выявления пациенток, которым необходимо хирургическое лечение, и прогнозирования результатов лечения.
Цель исследования – провести анализ показателей КЖ женщин с ГИЭ до и после оперативного лечения.
Материалы и методы
В исследование включены 93 женщины (основная группа) с глубоким инфильтративным эндометриозом, прошедших оперативное лечение в хирургическом отделении НМИЦ АГП им.В.И. Кулакова МЗ РФ в период с 2017 по 2019 гг., из которых 47 полностью завершили исследование к декабрю 2019 г., и 31 женщина без эндометриоза (группа контроля). Оценку КЖ проводили с использованием опросника SF-36 при поступлении в стационар и через 6–8 месяцев после оперативного лечения. Полученные результаты сравнивали по десяти шкалам, вычисляемым согласно методологии анализа результатов, полученных при помощи данного опросника. В ходе исследования, в зависимости от степени распространения ГИЭ, пациентки основной группы были разделены на четыре подгруппы в зависимости от локализации очага на основе классификации ENZIAN: группа А (n=12) – глубокий инфильтративный ретроцервикальный эндометриоз, эндометриоз ректовагинальной перегородки; группа В (n=16) – глубокий инфильтративный эндометриоз крестцово-маточных, кардинальных связок, боковых стенок малого таза; группа С (n=49) – глубокий инфильтративный эндометриоз ректосигмоидного отдела толстой кишки; группа F (n=16) – глубокий инфильтративный эндометриоз мочевого пузыря. Дополнительно проведен сравнительный анализ показателей КЖ у женщин с различным размером наибольшего очага ГИЭ вне зависимости от локализации: в 1-ю группу были включены женщины с размерами наибольшего очага до 1 см, во 2-ю – с размерами очага от 1 до 3 см, в 3-ю – с размерами очага более 3 см. Для более углубленного изучения КЖ женщин с ГИЭ проведен сравнительный анализ показателей в зависимости от наличия бесплодия и оперативного лечения по поводу эндометриоза в анамнезе.
Статистическую обработку данных проводили с использованием программы SPSS 23. Учитывая ненормальное распределение данных в исследуемых совокупностях, описательные данные представлены в виде медианы (Median) и межквартильного интервала (IQR). Для оценки статистической значимости различий использовали непараметрические критерии. Для оценки значимости различий между двумя совокупностями применяли тест Вилкоксона–Манна–Уитни, при сравнении более двух групп – тест Краскела–Уоллиса. Для качественных признаков данные представлены в виде абсолютного числа и доли в процентах (n (%)). Для оценки статистической значимости различий долей применялся тест хи-квадрат Пирсона либо, при малом количестве наблюдений, – точный тест Фишера. Данные о вероятности ошибки первого рода приводятся в столбце p-value (р). Критическим значением для отклонения нулевой гипотезы принималось значение p>0,05.
Результаты и обсуждение
Возраст пациенток в основной группе и группе контроля варьировал от 22 до 47 лет. В основной группе медиана возраста составила 34 года (Q1–Q3: 29,5–39,0 лет), в группе контроля 31 год (Q1–Q3: 28,0–37,0 лет). Статистически значимых различий по возрасту в исследуемых группах выявлено не было (р=0,116).
Сопутствующая соматическая патология была выявлена у 67/93 (72,0%) пациенток основной группы и у 27/31 (87,1%) пациенток группы контроля. Статистически значимых различий в частоте встречаемости сопутствующей патологии в исследуемых группах выявлено не было (р=0,75).
При анализе анамнестических данных обращало внимание то, что у пациенток основной группы в анамнезе было до 9 оперативных вмешательств, в то время как у пациенток группы контроля этот показатель не превышал 3. При анализе средних показателей количества операций в анамнезе у пациенток исследуемых групп была выявлена закономерность – у пациенток основной группы медиана общего количества оперативных вмешательств составила 3 (Q1–Q3:1–3), в то время как в группе контроля медиана составила 1 (Q1–Q3:0–2), данные различия были статистически значимы (р<0,001). Такие различия были обусловлены статистически значимо большей медианой гинекологических операций в анамнезе у пациенток основной группы (р<0,001)
При сравнительном анализе нарушений менструального цикла в исследуемых группах отмечается статистически значимо большее число пациенток, испытывающих болезненные ощущения при менструации – 71/93 (76,3%) в основной группе против 6/31 (19,4%) в группе контроля (р<0,001). Пациентки основной группы в 51,6% случаев испытывали обильные менструации, в группе контроля этот показатель был статистически значимо ниже и составлял 19,4%. Примечательно то, что в основной группе пациентки также сообщали о скудных менструациях в 7/93 (7,5%) и о «мажущих» сукровичных выделениях в межменструальный период в 8/93 (8,6%) наблюдений, в то время как в группе контроля таких нарушений менструального цикла не наблюдалось. Однако эти различия не были статистически значимыми.
При анализе репродуктивной функции не было выявлено статистически значимых различий в частоте беременности, родов, способе родоразрешения, частоте естественных и искусственных прерываний беременности, несостоявшихся выкидышей и внематочных беременностей (р>0.05).
Общее количество оперативных вмешательств по поводу эндометриоза в основной группе пациенток составило 83/182 (45,6%) от общего количества перенесенных оперативных вмешательств, и 83/146 (56,8%) от количества гинекологических операций в данной группе. Количество оперативных вмешательств по поводу эндометриоза в анамнезе у пациенток в основной группе достигало 5, при этом медиана составила 1 (Q1–Q3:0–1).
При анализе перенесенных оперативных вмешательств по поводу эндометриоза в основной группе было выявлено, что 42/93 (45%) женщин не имели оперативных вмешательств в анамнезе, 34/93 (36,5%) имели одно оперативное вмешательство в анамнезе, 12/93 (13%) пациенток – 2 оперативных вмешательства, а оставшиеся 5/93 (5,5%) пациенток имели 3 и более оперативных вмешательств в анамнезе.
При анализе структуры перенесенных оперативных вмешательств по поводу эндометриоза в основной группе выявлено, что в большинстве случаев – 72/83 (86,7%), оперативные вмешательства были выполнены лапароскопическим доступом в плановом порядке – 77/83 (92,6%). Чаще всего при оперативном вмешательстве была выполнена резекция одного яичника в связи с эндометриоидной кистой (28/83 (34%)), коагуляция очагов эндометриоза (12/83 (15%)), адгезиолизис (11/83 (14%)) и иссечение очагов эндометриоза (9/83 (11%)) (рисунок). Примечательным является то, что у 3/83 (3,6%) пациентов в анамнезе уже была резекция толстой кишки в связи с колоректальным эндометриозом. Ни одна пациентка не сообщала об осложнениях в послеоперационном периоде.
Рецидивы заболевания у пациенток основной группы, имеющих в анамнезе оперативное лечение по поводу эндометриоза, в форме глубокого инфильтративного эндометриоза к моменту исследования можно объяснить не только возможностью нерадикальностью первичного оперативного вмешательства, но и агрессивным течением заболевания или неэффективностью/неадекватностью противорецидивной терапии. Ретроспективный характер исследования, длительное течение заболевания, отсутствие выписных эпикризов и выписок из амбулаторных карт, в полной мере отражающих характер течения заболевания и методы лечения, ограничивают возможности анализа факторов риска рецидива. Необходимо изучение и более углубленный и масштабный анализ этих аспектов течения заболевания для определения наиболее значимого фактора, способствующего рецидиву.
При сравнительной оценке КЖ пациенток с ГИЭ и практически здоровых женщин по всем шкалам выявлены меньшие показатели медианы КЖ у женщин основной группы по сравнению с группой контроля. При этом статистически значимые различия (р≤0,05) выявлены по всем шкалам (табл.1).

Результаты исследования подтверждают, что ГИЭ оказывает значительное негативное влияние на большую часть сфер жизни женщин: ограничивает физическую активность, в том числе из-за более выраженного болевого синдрома, что обуславливает снижение ролевого функционирования, т.е. негативно влияет на объем и скорость выполняемой работы и повседневных обязанностей. Женщины с ГИЭ проявляют меньше жизненной и социальной активности, обладают меньшей способностью к регуляции своих эмоций, ниже оценивают свое здоровье по сравнению с женщинами группы контроля. Все эти аспекты обуславливают более низкие результирующие показатели КЖ – физическое и психическое здоровье. Полученные результаты согласуются с данными опубликованных отечественных и зарубежных научных исследований [4–7].
При сравнительной оценке показателей КЖ пациенток с ГИЭ различной локализации статистически значимых различий выявлено не было (p>0,05) (табл. 2). В литературе опубликовано ограниченное количество данных, оценивающих корреляцию между локализацией очага поражения на основе классификации ENZIAN и проявлениями заболевания. Авторы демонстрируют статистически значимые различия в частоте встречаемости и выраженности таких симптомов, как дисхезия, диспареуния, дизурия и дисменоррея при различной локализации очагов ГИЭ [35–37].
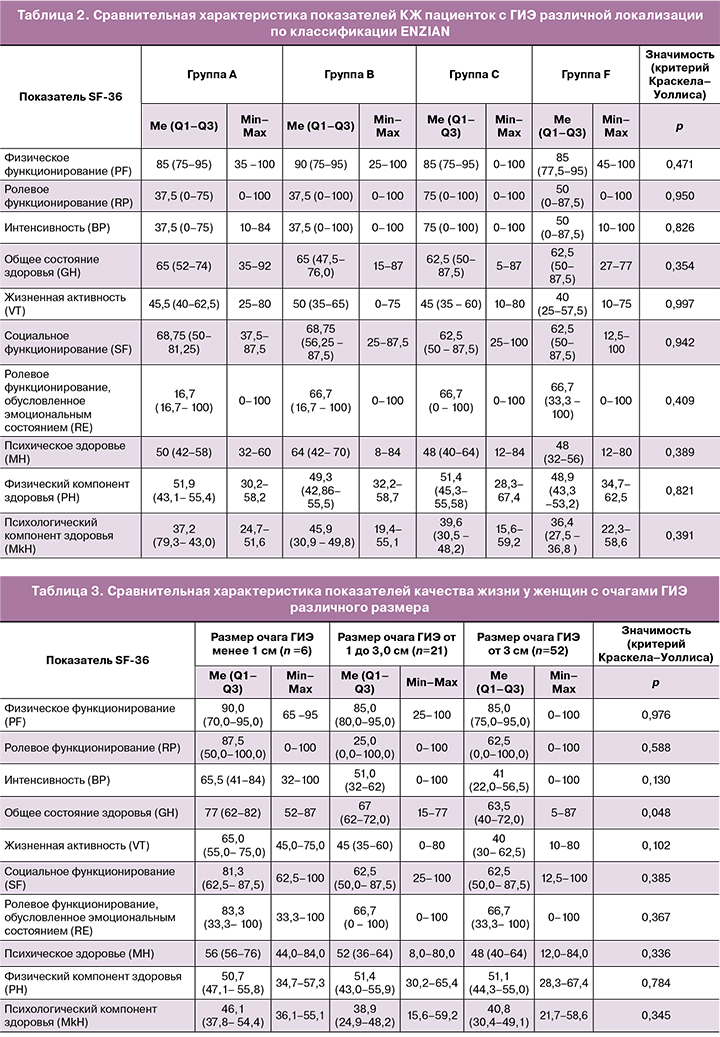
Однако, исследований, сравнивающих КЖ пациенток в данных группах среди опубликованных научных работах не найдено. В этом свете представляется перспективным углубленное изучение корреляции между наличием и выраженностью симптомов ГИЭ и КЖ для выработки персонифицированного подхода в лечении.
Также проведен анализ показателей КЖ пациенток в зависимости от размера наибольшего очага. В 1-ю группу вошли женщины с размерами большего очага до 1,0 см, 2-ю группу – от 1,0 до 3,0 см, 3-ю группу – более 3,0 см. При сравнительной оценке показателей КЖ пациенток с очагами ГИЭ различного размера статистически значимые различия (p<0,05) были выявлены только по шкале «общая оценка своего здоровья». По остальным шкалам статистически значимых различий выявлено не было (табл. 3). Полученные данные подтверждают результаты других исследований. Так, при анализе показателей качества жизни в зависимости от стадии заболевания на основании классификации американского общества фертильности (ASRM) так же не было выявлено статистически значимых различий [38–40].
Также проведен анализ КЖ пациенток с ГИЭ в зависимости от наличия бесплодия и наличия оперативного лечения эндометриоза в анамнезе.
При сравнительной характеристике женщин, предъявляющих жалобы на бесплодие (n=39), и женщин без бесплодия (n=54) были выявлены более высокие показатели КЖ по всем шкалам опросника SF-36 у женщин с бесплодием. При этом статистически значимые различия (p<0,05) в показателях качества жизни были выявлены по шкалам «Социальное функционирование» (SF), «Жизненная активность» (VT), «Интенсивность боли» (BP) и «Физическое функционирование» (PF) (табл. 4).

Данные исследований, изучающих влияние бесплодия на КЖ женщин с ГИЭ противоречивы. Несмотря на то, что многие авторы утверждают, что наличие бесплодия в значительной степени усугубляет психологическое состояние пациентки, в нашем исследовании это не нашло подтверждения [27, 41, 42].
Имеющиеся различия, возможно, объясняются тем, что у женщин с бесплодием, включенных в данное исследование, нет ярко выраженной клинической симптоматики, вызванной течением ГИЭ, а доминирующим симптомом заболевания и поводом для обращения к врачу являлось именно отсутствие наступления беременности. Таким образом, пациентки с бесплодием не испытывали большого спектра симптомов, связанных с ГИЭ, что обусловливало более высокие показатели КЖ по всем шкалам, свидетельствующими о более высокой жизненной и социальной активности, и менее значительном ограничении физического функционирования у этих пациенток. Это подтверждает выводы, полученные другими авторами, утверждающими, что более значимым фактором, негативно влияющим на КЖ, является наличие болевого синдрома [8, 10].
При сравнительном анализе показателей КЖ женщин, оперированных по поводу эндометриоза впервые (n=42), и женщин с оперативным лечением эндометриоза в анамнезе (n=51) были отмечены более высокие показатели КЖ по всем шкалам опросника SF-36 у женщин оперированных повторно. Статистически значимыми различия (р<0,05) были выявлены по шкалам «Интенсивность боли» (BP), «Физическое функционирование» (PF) и «Физический компонент здоровья» (PH) (табл. 5). Аналогичные исследования демонстрируют, что оперативное лечение ГИЭ может сохранять эффективность с позиции улучшения КЖ до 4-х лет послеоперационного наблюдения [34], однако в случае возникновения рецидива заболевания оперативное лечение приводит к менее значимому улучшению показателей КЖ [33]. В данном свете необходимо еще раз подчеркнуть важность выполнения оптимального объема оперативного вмешательства для достижения максимально возможной циторедукции при первичном оперативном вмешательстве по поводу эндометриоза.
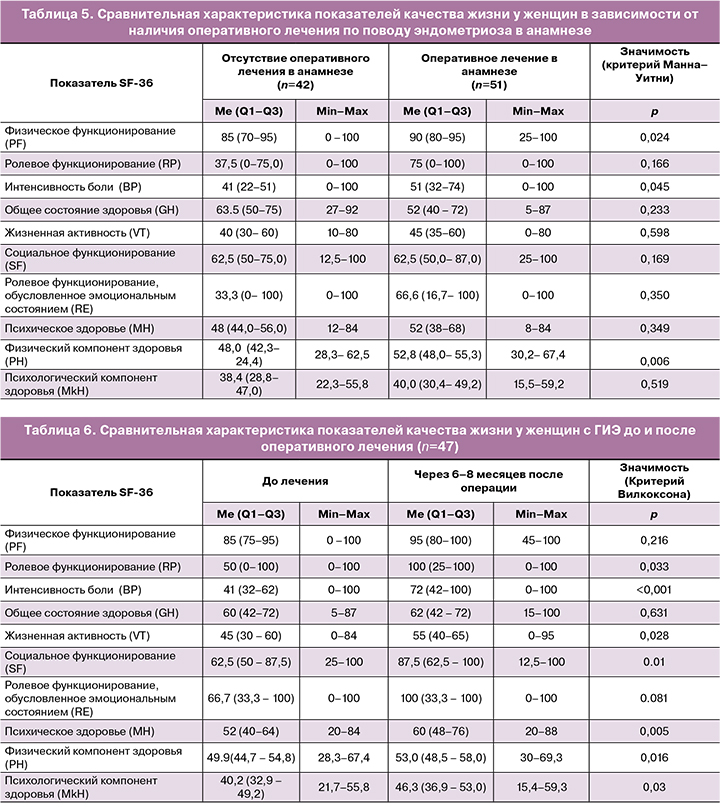
При сравнительной характеристике показателей КЖ пациенток с ГИЭ до и после оперативного лечения было отмечено улучшение по всем шкалам опросника SF-36. Интенсивность болевых ощущений статистически значимо снизилась, что выражается в увеличении значения по шкале «телесная боль» с 41 (Q1–Q3; 32–62) до 72 (Q1–Q3; 42–100) (р<0,001), однако увеличение медианы показателя «физическое функционирование» с 85 (Q1–Q3;75–95) до 95 (Q1–Q3; 80–100) не было статистически значимым. В то же время показатель «Ролевое функционирование, обусловленное физическим состоянием» статистически значимо увеличился с 50 (Q1–Q3;0–100) до 100 (Q1–Q3; 25–100) (р<0,033). Таким образом, несмотря на снижение болевых ощущениq, физическая активность женщин с ГИЭ после операции оставалась ограниченной (самообслуживание, ходьба, подъем тяжестей, ходьба по лестнице и т.п.), в то время как уменьшилось ограничивающее влияние физических ощущений, связанных с ГИЭ на повседневную деятельность (работа, выполнение повседневных обязанностей). Показатели «Жизненная активность» и «Социальное функционирование» через 6–8 месяцев после операции статистически значимо увеличились с 45 (Q1–Q3; 30– 60) до 55 (Q1–Q3; 40–65) и с 62,5 (Q1–Q3; 50–87,5) до 87,5 (Q1–Q3; 62,5–100) соответственно (р<0,05), что говорит об улучшении психического здоровья пациенток, снижении количества негативных эмоций. Также через 6–8 месяцев после операции показатель «Психическое здоровье» статистически значимо увеличился с 52 (Q1–Q3; 40–64) до 60 (Q1–Q3;48–76) (р=0,005). Однако, увеличение показателя «Ролевое функционирование, обусловленное эмоциональным состоянием» с 66,7 (Q1–Q3; 33,3–100) до 100 (Q1–Q3; 33,3–100) не было статистически значимым (р=0,081). Таким образом, влияние психического состояния, обусловленного ГИЭ, на повседневную деятельность через 6–8 месяцев после операции статистически значимо не изменилось и остается низким. Результирующие показатели опросника SF-36 – «физическое здоровье» и «психическое здоровье» статистически значимо увеличились через 6–8 месяцев после операции с 49,9(Q1–Q3;44,7–54,8) до 53,0 (Q1–Q3;48,5–58,0) и с 40,2 (Q1–Q3;32,9–49,2) до 46,3 (Q1–Q3;36,9–53,0) соответственно (р=0,016 и р=0,03 соответственно). Несмотря на это, показатель «Общая оценка своего здоровья» оставалась на прежнем низком уровне (табл. 6). Изменение данного показателя в большей степени зависит от восприятия пациенткой своего заболевания. Возможно, включение психотерапевтической поддержки пациенткам в послеоперационном периоде позволит улучшить этот показатель.

Полученные результаты подтверждают выводы других авторов – оперативное лечение значительно улучшает показатели качества жизни пациенток с ГИЭ [30–33]. Считается, что хирургическое удаление очагов приводит к улучшению преимущественно физического компонента КЖ [42], однако в нашем исследовании продемонстрировано значительное улучшение и психологического компонента. Вероятнее всего, это обусловлено снижением выраженности болевого синдрома, что еще раз подчеркивает его доминирующую роль в снижении показателей КЖ [10]. Однако для более точных выводов необходим более углубленный анализ корреляции симптоматики с показателями КЖ.
Заключение
Глубокий инфильтративный эндометриоз приводит к значительному снижению всех показателей КЖ женщин вне зависимости от локализации очага и его размеров. КЖ женщин с ГИЭ, основной жалобой которых является бесплодие, выше, чем у женщин, имеющих развернутую клиническую симптоматику заболевания, но не страдающих бесплодием. Хирургическое удаление очагов является эффективным методом с длительным частичным эффектом, однако вероятно должно быть дополнено психотерапевтическим лечением. Исходя из данных, полученных при сравнительном анализе показателей КЖ у пациенток с наличием оперативного лечения эндометриоза в анамнезе и без такового, можно сделать вывод, что оперативное лечение эндометриоза даже в отдаленном периоде приводит к статистически значимому снижению болевого синдрома, улучшению физического функционирования и физического компонента КЖ в целом. Однако не наблюдается статистически значимого улучшения психического здоровья пациенток, их жизненной и социальной активности, общей оценки своего здоровья и облегчения в выполнении повседневных обязанностей.