Несмотря на серьезные достижения в диагностике и лечении гинекологических заболеваний, аномалии развития матки остаются одной из актуальных проблем. Диагностика врожденных аномалий развития матки и влагалища представляет значительные трудности, несмотря на широкий спектр современных методов визуализации (лапароскопия, гистероскопия, гистеросальпингография, ультразвуковое исследование (УЗИ), магнитно-резонансная томография (МРТ)), и приводит к ошибкам в распознавании характера порока. У 24–34% больных с врожденными аномалиями репродуктивной системы диагноз неясен или некорректно сформулирован, что в дальнейшем влияет на эффективность лечения и сохранения репродуктивной функции пациенток [1]. Несмотря на то что аномалии развития матки являются сравнительно редкой патологией, диагностика и коррекция ее представляют чрезвычайно сложную задачу в плане восстановления репродуктивной функции и благоприятного исхода беременности и родов [2, 3].
Описание клинического наблюдения
На кафедру акушерства и гинекологии Волгоградского государственного медицинского университета за консультативной помощью обратилась пациентка 31 года с жалобами на отсутствие беременности в течение 5 лет. Из анамнеза выяснено, что женщина состоит в первом браке 6 лет. За этот период времени наблюдалась врачом женской консультации, обследовалась на инфекции, передающиеся половым путем, неоднократно проводилось УЗИ органов малого таза, оценка гормонального профиля. В результате лабораторных и инструментальных исследований патологии со стороны женской половой сферы не выявлено. Проведено комплексное обследование супруга пациентки андрологом, мужской фактор бесплодия не диагностирован.
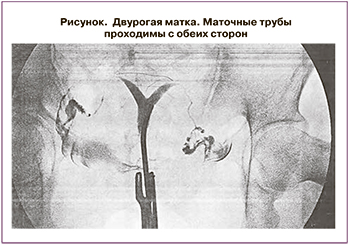 В условиях университетской клиники №1 ВолгГМУ выполнено общеклиническое, гинекологическое исследование и УЗИ органов малого таза. При выполнении УЗИ выявлена аномалия развития матки в виде двурогой матки. Ультразвуковым признаком данной аномалии явилось 2 М-эхо в средней и верхней третях матки. УЗ-мониторинг овуляции и состояния эндометрия выявил хроническую ановуляцию. С целью уточнения вида аномалии развития матки и проходимости маточных труб пациентке рекомендована метросальпингография. При выполнении рентгенологического исследования выявлено следующее: двурогая матка, маточные трубы проходимы с обеих сторон (рисунок).
В условиях университетской клиники №1 ВолгГМУ выполнено общеклиническое, гинекологическое исследование и УЗИ органов малого таза. При выполнении УЗИ выявлена аномалия развития матки в виде двурогой матки. Ультразвуковым признаком данной аномалии явилось 2 М-эхо в средней и верхней третях матки. УЗ-мониторинг овуляции и состояния эндометрия выявил хроническую ановуляцию. С целью уточнения вида аномалии развития матки и проходимости маточных труб пациентке рекомендована метросальпингография. При выполнении рентгенологического исследования выявлено следующее: двурогая матка, маточные трубы проходимы с обеих сторон (рисунок).
В результате проведенного обследования выставлен окончательный диагноз: первичное бесплодие, двурогая матка, хроническая ановуляция.
В данной клинической ситуации пациентке рекомендовано дополнительное обследование (УЗИ почек) и лечение (дидрогестерон 10 мг + эстрадиол 2 мг по 1 таблетке 1 раз в день в течение 6 месяцев; аппликации лечебной грязи озера Эльтон на низ живота №10; консультация в одном из московских НИИ акушерства и гинекологии для решения дальнейшей тактики ведения больной).
Пациентка начала курс назначенного лечения и по собственной инициативе обратилась за дополнительными консультациями в отделения вспомогательных репродуктивных технологий г. Волгограда и г. Казани, где ей было предложено суррогатное материнство, от которого она категорически отказалась.
В дальнейшем при консультации в отделении гинекологической эндокринологии ГБУЗ МО МОНИИАГ и выполнении 3D-УЗИ подтвержден диагноз: первичное бесплодие, двурогая матка, хроническая ановуляция. Выполнения МРТ, гистероскопии, лапароскопии с целью дообследования и хирургической коррекции порока не потребовалось.
Рекомендовано продолжить прием вышеуказанного препарата (дидрогестерон 10 мг + эстрадиол 2 мг по 1 таблетке 1 раз в день в течение года), контрольное УЗИ органов малого таза через 3 и 6 месяцев, биохимический анализ крови (печеночные пробы, коагулограмма и др.). После окончания лечения пациентке рекомендовано выполнить контроль уровней лютеинизирующего, фолликулостимулирующего, антимюллерова гормонов, пролактина, и ингибина В, УЗИ органов малого таза и решить вопрос о возможности стимуляции овуляции.
Через 12 месяцев при контрольном УЗИ органов малого таза после проведенного курса лечения отмечена положительная динамика: 2М-эхо только в верхней половине полости матки. Затем проведена стимуляция овуляции кломифена цитратом в дозировке 100 мг с 3-го по 7-й день менструального цикла и фоллитропином альфа 75 МЕ подкожно на 9-й, 10-й, 11-й день менструального цикла. Дополнительно применялись эстрадиол гель 1 г на низ живота (при достижении фолликула 15 мм в диаметре) и фолиевая кислота по 400 мкг в сутки. Поддержка 2-й фазы менструального цикла осуществлялась прогестагенами (дидрогестерон в таблетках по 10 мг 2 раза в день). На фоне проводимой терапии у пациентки наступила беременность в правом маточном роге, что было подтверждено данными УЗИ от 23.10.2018.
На диспансерный учет по беременности пациентка встала в сроке 8 недель. Обследована в соответствии с приказом Министерства здравоохранения РФ от 01 ноября 2012 г. N 572н «Об утверждении Порядка оказания медицинской помощи по профилю “акушерство и гинекология (за исключением использования вспомогательных репродуктивных технологий)”». У пациентки выявлена экстрагенитальная патология в виде хронического гайморита в стадии ремиссии и нейродермита. Течение данной беременности осложнилось умеренной рвотой в 9–10 недель гестации. В связи с угрозой преждевременных родов в 22–23 и 26–27 недель беременности пациентка дважды госпитализировалась в отделение патологии беременности ГУЗ КБ родильный дом №5, где проводилась токолитическая терапия гексопреналина сульфатом и микронизированным прогестероном в суточной дозе 200 мг вагинально (до 34 недель беременности). В плановом порядке беременная была родоразрешена путем операции кесарева сечения в Волгоградском областном клиническом перинатальном центре №1 им. Л.И. Ушаковой при сроке беременности 39 недель. На 5-й минуте извлечен мальчик массой 3670 г, по шкале Апгар 8–9 баллов. Операция прошла без технических трудностей. Кровопотеря составила 560 мл. Послеоперационный период протекал без осложнений. Пациентка выписана домой на 6-е сутки с ребенком.
Обсуждение
Комплексное обследование женщин с подозрением на аномалии развития матки включает одномоментное проведение гистероскопии и лапароскопии. Однако это инвазивные методы, связанные с рисками проведения анестезиологического пособия [4–6].
Прогноз репродуктивных исходов зависит от анатомической формы порока, а также от сопутствующих эндокринных и функциональных нарушений. Гиперандрогения встречается у 20% больных, гипофункция яичников – у 15%, ановуляция различного генеза – у 34%, нарушение проходимости маточных труб – у 22%, спаечный процесс в малом тазу – у 17%; хронический эндометрит, внутриматочные синехии, гиперплазия эндометрия – у 7% больных [7].
Показатели восстановления репродуктивной функции после проведения реконструктивных операций остаются недостаточно высокими: частота наступления беременности – 54,5%, а потери беременности у них достигают 20–29% [8].
Также аномалии развития женских половых органов являются причинами различных осложнений, возникающих во время беременности (самопроизвольное ее прерывание – 23%, преэклампсия – 41%, кровотечения вследствие предлежания плаценты и преждевременной отслойки нормально расположенной плаценты – 5%) и в родах (слабость родовой деятельности – 15%, преждевременные роды – 18%, послеродовые кровотечения – 35%, разрыв матки – 5%). Бесплодие, ассоциированное с данной патологией, отмечается в 13% случаев [9].
В представленном клиническом наблюдении диагноз аномалии развития матки был установлен в результате выполнения экспертного УЗИ. Трехмерное трансвагинальное УЗИ органов малого таза (3D-УЗИ) является неинвазивным методом визуализации, который позволяет оценить как внешние, так и внутренние контуры матки, состояние эндометрия, яичников и маточных труб, что делает его сравнимым с МРТ [10–15]. Комплексное лечение, персонифицированный подход к пациентке позволили реализовать детородную функцию.
Заключение
Необходимость достоверной диагностики каждого подтипа аномалий матки коррелирует с вероятностью благоприятного исхода родов при каждой патологии, частотой осложнений беременности. Лечение пациенток с аномалиями развития матки представляет значительные сложности в связи с необходимостью использования комплексных методов лечения, терапии сопутствующих эндокринных нарушений, наблюдения, прогнозирования и коррекции осложнений беременности.