Cardiovascular risk assessment tools for optimizing pregravid preparation: the results of the study on working women of reproductive age
Salov I.A., Malinova L.I., Tolstov S.N., Zhuk A.A., Denisova T.P.
Objective: To assess the possibilities of cardiovascular risk assessment tools for optimizing pregravid preparation of working women of reproductive age.
Materials and methods: A comprehensive analysis of employees at three commercial and manufacturing enterprises was conducted. The study included women with normal menstrual function planning pregnancy or who did not exclude the probability of getting pregnant within the next year. Age group classification adjusted for the study sample was used: Group 1 (peak fertility), Group 2 (reduced fertility), and Group 3 (perimenopause). The 10-year risk of fatal cardiovascular events (CVEs), total cardiovascular risk (TCR), and the parameters of cardiovascular health were assessed.
Results: The highest scores of total cardiovascular risk and the risk of fatal cardiovascular events were in perimenopause group – 1/20 (0/87; 2.01)% and 0.30 (0.22; 0.50)%, respectively, p=0.000. The highest cardiovascular health score was in the group of peak fertility – 575 (525; 600) (р=0.025, and had an inverse correlation with gestational hypertension in history (τ=-0.352; p=0.011), which, in turn, was distinguished by the highest population attributable risk of arterial hypertension (23.55%, p=0.002).
Conclusion: In the sample of working women of reproductive age, who were planning pregnancy or did not exclude the probability of getting pregnant, routine use of traditional cardiovascular risk assessment tools is not advisable. Integral assessment of cardiovascular health is associated with age-related fertility and can be used for risk stratification of hypertensive disorders at the stage of pregravid preparation.
Authors' contributions: Salov I.A., Malinova L.I., Tolstov S.N., Denisova T.P. – the concept and design of the study; Zhuk A.A., Malinova L.I. – material collection and processing; Malinova L.I., Denisova T.P. – statistical data processing, Malinova L.I., Tolstov S.N., Denisova T.P. – analysis and interpretation of the results. Malinova L.I., Zhuk A.A. – article writing; Salov I.A., Malinova L.I., Tolstov S.N., Denisova T.P. – article editing.
Conflicts of interest: The authors confirm that they have no conflicts of interest to declare.
Funding: The study was conducted in the frames of research initiative.
Ethical Approval: The study was approved by the local Ethics Committee of Saratov State Medical University named
after V.I. Razumovsky, Ministry of Health of Russia.
Patient Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Salov I.A., Malinova L.I., Tolstov S.N., Zhuk A.A., Denisova T.P. Cardiovascular risk assessment tools for optimizing pregravid preparation: the results of the study on working women of reproductive age.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2024; 11: 155-161 (in Russian)
https://dx.doi.org/10.18565/aig.2024.230
Keywords
Given the current medical and demographic situation in the Russian Federation, the issue of optimizing pregravid preparation is of exceptional importance. Extragenital pathology has the highest share in the structure of the causes of maternal mortality, including in our country [1]. Among this group of conditions, cardiovascular diseases (CVDs) rank first. This dramatic alliance served as the basis to create a new subspecialty – cardio-obstetrics [2], the clinical significance of which is yet to be understood. However, at the current stage it is becoming obvious that the existing pregravid preparation protocols [3] are far from perfect, primarily in terms of risk stratification of cardiovascular events.
At present, special attention is paid to the development and clinical implementation of quantitative risk assessment of adverse cardiovascular events or construction of individual nosologies, based on comprehensive analysis of clinical, genetic, anthropological, social and other factors, taking into account their predictive value, the so-called riskometry. However, the vast majority of predictive scales and indices (risk assessment tools) were developed regardless of specific characteristics of women’s health [4].
All of the above served as the basis to conduct the study, the purpose of which was to assess the possibilities of cardiovascular risk assessment tools for optimizing pregravid preparation of working women of reproductive age.
Material and methods
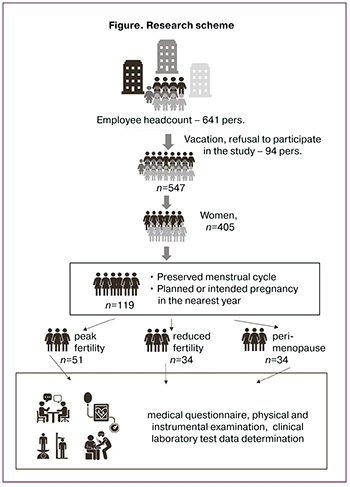
A comprehensive analysis of employees at three commercial and manufacturing enterprises was conducted. The study included 547 employees aged 21–79 years, and 405/547 (74.0%) of them were female employees. The main group consisted of 119 women, who at the time of medical examination had regular menstrual cycles and were planning for pregnancy or had intention to become pregnant within the next year (Figure). Age group classification adjusted for the study sample was used for comparative analysis [5]: group 1 (peak fertility, n=51) aged 20–35 years, group 2 (reduced fertility, n=34) aged 36–45 years, and group 3 (perimenopause, n=34) aged over 45 years (before menopause).
The study included medical questionnaire, physical and instrumental examination, clinical laboratory test data determination. The questionnaire included: 1) medical and demographic data; 2) formalized obstetric and gynecological history; 3) sleep quality; 4) seeking medical care over the past year; 5) the results of self-assessment of health status. All research procedures were standardized in accordance with epidemiological methods for identification of major chronic non-communicable diseases and risk factors [6].
Physical examination included ausculatory blood pressure (BP) measurement on the right and left arms, heart rate calculation and anthropometric measurements (height, weight, waist and hip circumference). In the “centralized” laboratory, total serum cholesterol levels, triglycerides, high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol, glucose, creatinine, and uric acid (UA) levels were determined using photocolorimetric method, Clima device (Spain) and test kits produced by LLC “Diacon DS”). Glomerular filtration rate was calculated using the CKD-EPI Creatinine Equation (2021 update) [7].
Assessment of 10-year risk of fatal cardiovascular events and total cardiovascular risk was performed for all patients, as described in our previous studies [8]. The integrated assessment of cardiovascular health in women of reproductive age was performed according to [9]; 7 modules were used: duration of night sleep, duration of habitual physical activity per day, smoking status, body mass index, blood pressure, lipid metabolism, and fasting blood glucose level.
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and National Standard of the Russian Federation “Good Clinical Practice” (GCP) (GOST R52379-2005). The protocol of the study was approved at the meeting of the local Ethics Committee. All participants have signed informed consent to participate in the study.
Statistical analysis
Individual data of patients in the study were blinded and recorded in accordance with the study protocol. Statistical analysis was performed using software packages SPSS (version 26.0.0.1); Excel Microsoft Office Professional plus 2010 (version 14.0.6112.5000). The quantitative characteristics were described using median (Me) and interquartile range (the lower quartile Q1; the upper quartile Q3). The ranked variables were described using absolute value (N) and frequency (%).
When planning the study, the necessary sample size was based on the power of the study (1-β) – 80% and the level of significance (α) – 5%. The minimal clinically important difference (d) for the basic biochemical parameters was 15%. The Kruskal–Wallis one-way analysis-of-variance-by-ranks test with subsequent pairwise comparison (when necessary), and the Jonckheere–Terpstra test for ordered differences for independent samples and the chi-square test of independence were used.
For the selected risk factors, the odds ratio with confidence interval (CI), attributable risk, the percentage of attributable risk, and population attributable risk were calculated. Correlation analysis was performed using Spearman and Kendall correlation coefficients. The level of significance (p) of 0.05 for two-tailed tests was used for testing statistical hypothesis.
Results
The clinical characteristics of women participating in the study is represented in Table 1. As can be seen from the presented data, younger female employees had higher education and lower body weight more often. All identified differences in the values of basic hemodynamic parameters were within normal range, and reflected age-related changes in the cardiovascular system (in the context of female age-related fertility decline; see the results of the Jonckheere–Terpstra test for ordered differences, Table 1).
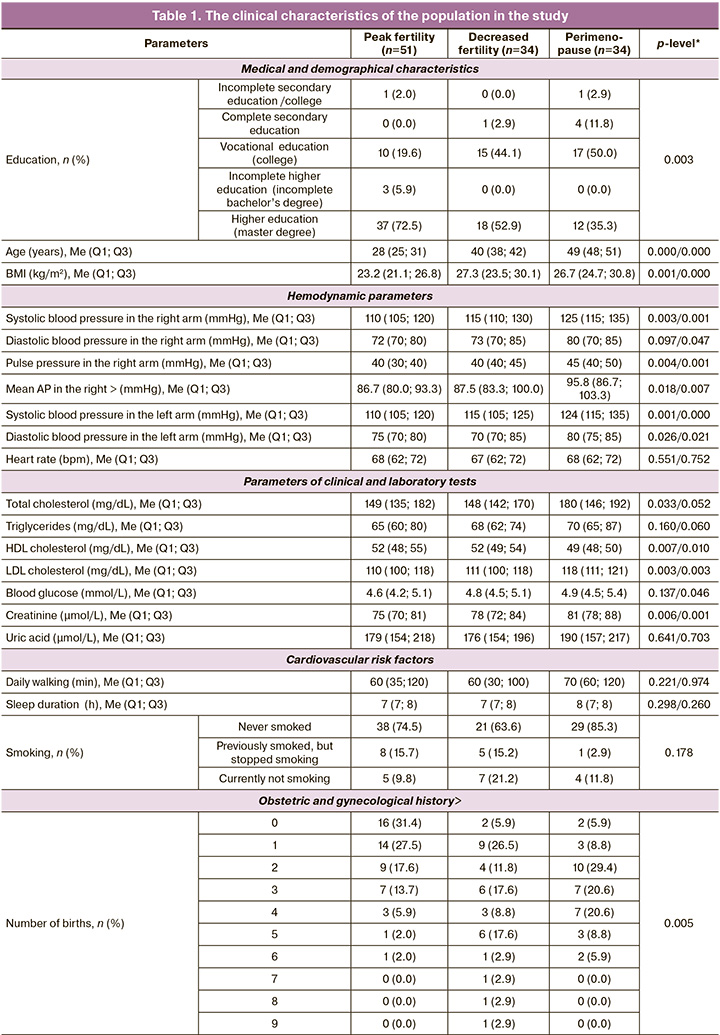
The similar situation refers to the parameters of lipid metabolism and creatinine levels.
In the examined population, no congenital defects or minor defects in cardiac development, as well as no pathological processes associated with atherosclerotic lesions of coronary arteries were detected. Arterial hypertension (AH) was found most frequently in group 3, but this difference was not statistically significant. In the same way as in large epidemiological studies, the frequency of antihypertensive therapy was lower compared to the prevalence of arterial hypertension in the examined population. Analysis of drug therapy showed that antihypertensive drug therapy with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers was predominant. At the time of examination, 11/119 women (9.2%) continued using hormonal contraceptives.
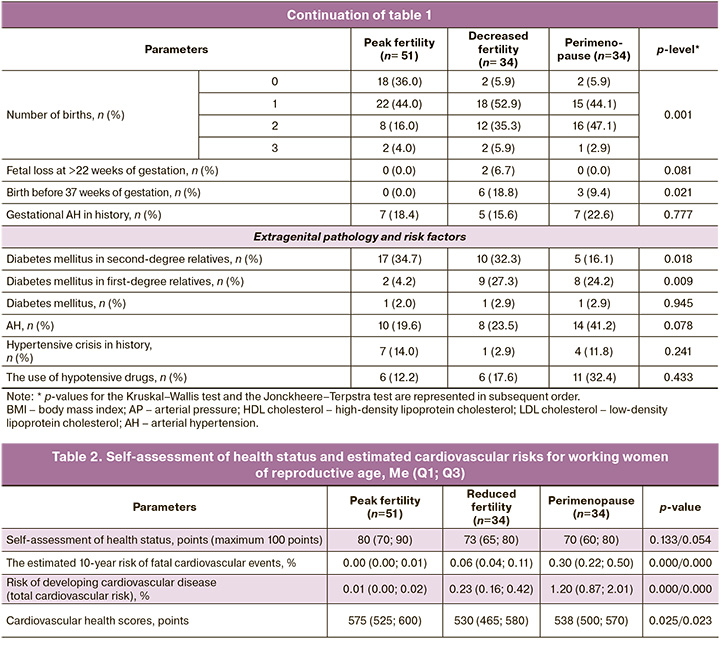
Based on the clinical characteristics of the sample, the modified WHO classification of maternal cardiovascular risk, as well as the CARPREG [10] and the ZAHARA [11] risk scores could not be applicable in our study. In this connection, we used the estimated 10-year risk of fatal cardiovascular events, total cardiovascular risk, as well as cardiovascular health scores. In our study, the healthy eating index was not included in cardiovascular health assessment. So, the optimal cardiovascular health score was 700 points.
As can be seen from the data represented in Table 2, according to cardiologists, the traditional risks in this sample are negligible, and the reliable differences are due to age difference in the compared groups. More interesting is comparison of cardiovascular health scores. However, the clinical significance of the differences, for example, 530 (465; 580) points versus 575 (525; 600) needs to be clarified.
Based on the structure of cardiovascular pathology in the sample, we assessed the clinical significance of cardiovascular health in relation to AH. Inverse correlations were found between the parameter "heart health" and the number of pregnancies (τ=-0.459, p=0.000), as well as the parameter “gestational hypertension (GH) in history” (τ=-0.352; p=0.011). Risk analysis is represented in Table 3.
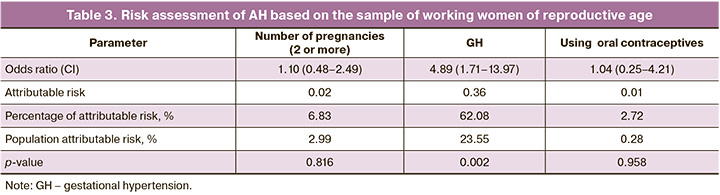
As can be seen from the results represented in Table 3, among the analyzed factors, only GH in history was significant for occurrence of AH. In other words, 23.55% of cases of AH in working women of reproductive age were associated with GH.
Discussion
Despite a great deal of studies devoted to pregravid preparation, we could find only a few number of studies on the optimizing assessment of total cardiovascular risk in terms of preparing for pregnancy. Usually, study subjects were the patients with known cardiovascular pathology or diseases closely intertwined in athogenetic sense with AH and atherosclerosis (obesity, diabetes mellitus). One of the largest research projects on the similar topic was the Norwegian cohort study [12], that analyzed the data on 13 217 pregnancies (1.59 births per 8321 women). The most interesting aspect of our study was the focus on hereditary burden of diabetes mellitus and arterial hypertension in terms of the risk of hypertensive disorders associated with pregnancy. Extensive data have been accumulated on the influence of several cardiovascular risk factors, that made it possible to recommend assessment of cardiovascular health in preparing women for pregnancy [13]. However, clinical validation of this approach has not yet been finalized.
The use of most known risk assessment tools is either limited by pre-existing cardiovascular pathology (the limitations of the modified WHO classification of maternal cardiovascular risk, the CARPREG and ZAHARA risk scores) or is devoid of practical meaning (the SCORE and SCORE-2 scales which are limited by the age of patients (≥40 years)).
Following the logic of the SCORE project (risk estimation based on the Weibull hazard function) in this study, once again proved the influence of age-related involution on the status of cardiovascular system. However, the practical use of these risk assessment tools seems questionable due to the negligible risk values. Whereas it was found that the parameter of cardiovascular health was less associated with the age, at the same time it maintains associative links with the parameters of obstetric and gynecological anamnesis and the presence of cardiovascular system pathology, in particular, arterial hypertension.
The major limiting factor of our study was sampling bias. The study subjects were predominantly clinically healthy women and had a fairly high socioeconomic status and level of education. In this category of women, where risk assessment was rather complicated, we obtained the results that seemed to us to be promising in terms of optimizing pregravid preparation, namely, introduction of cardiovascular health assessment into health screening program for women planning for pregnancy.
From the practical point of view, detection of the fact of using teratogenic antihypertensive drugs (angiotensin-converting enzyme inhibitors and angiotensin receptor blockers) by women of reproductive age, who were planning for pregnancy or had intention to become pregnant, including those who were not satisfied with the use of contraceptive method, is undoubtedly important. Despite the apparency of this issue, it is necessary to emphasize the exceptional importance of reconsidering antihypertensive therapy in patients, who are planning for pregnancy or have intention to become pregnant.
Conclusion
In the study sample of working women of reproductive age, who were planning for pregnancy or had intention to become pregnant, routine use of traditional cardiovascular risk assessment tools is not advisable. Integral assessment of cardiovascular health is associated with age-related fertility and can be used for risk stratification of hypertensive disorders at the stage of pregravid preparation.
References
- Филиппов О.С., Гусева Е.В. Материнская смертность в Российской Федерации в 2019 г. Проблемы репродукции. 2020; 26(6): 8-26.. [Filippov O.S., Guseva E.V. Maternal mortality in the Russian Federation in 2019. Russian Journal of Human Reproduction. 2020; 26(6‑2): 8‑26.(in Russian)]. https://dx.doi.org/10.17116/repro2020260628.
- Davis M.B., Arendt K., Bello N.A., Brown H., Briller J., Epps K. et al. Team-Based Care of Women With Cardiovascular Disease From Pre-Conception Through Pregnancy and Postpartum: JACC Focus Seminar 1/5. J. Am. Coll. Cardiol. 2021; 77(14): 1763-77. https://dx.doi.org/10.1016/j.jacc.2021.02.033.
- Междисциплинарная ассоциация специалистов репродуктивной медицины (МАРС). Прегравидарная подготовка. Клинический протокол. Версия 3.1. М.: Редакция журнала StatusPraesens; 2024. 124 с. [Interdisciplinary Association of Reproductive Medicine Specialists (MARS). Pregravid preparation. Clinical protocol. Version 3.1. Moscow: Editorial office of the StatusPraesens Journal; 2024. 124 p. (in Russian)].
- American College of Gynecologists Committee on Gynecologic Practice. Female age-related fertility decline. Committee Opinion No. 589. Fertil. Steril. 2014; 101(3): 633-4. Epub 2014/02/25. https://dx.doi.org/10.1016/j.fertnstert.2013.12.032.
- Badawy M.A.E.M.D., Naing L., Johar S., Ong S., Rahman H.A., Tengah D.S.N.A.P. et al. Evaluation of cardiovascular diseases risk calculators for CVDs prevention and management: scoping review. BMC Public Health. 2022; 22(1): 1742. https://dx.doi.org/10.1186/s12889-022-13944-w.
- Калинина А.М., Шальнова С.А., Гамбарян М.Г., Еганян Р.А., Муромцева Г.А., Бочкарева Е.В., Ким И.В. Эпидемиологические методы выявления основных хронических неинфекционных заболеваний и факторов риска при массовых обследованиях населения. Методическое пособие. Бойцов С.А., ред. М.; 2015. 96 c. [Kalinina A.M., Shalnova S.A., Gambaryan M.G., Eganyan R.A., , Muromtseva G.A., Bochkareva E.V., Kim I.V. Epidemiological methods for identifying major chronic non-communicable diseases and risk factors during mass population surveys. Boytsov S.A, ed. Moscow; 2015. 96 p. (in Russian)].
- Miller W.G., Kaufman H.W., Levey A.S., Straseski J.A., Wilhelms K.W., Yu H.E. et al. National Kidney Foundation Laboratory Engagement Working Group Recommendations for Implementing the CKD-EPI 2021 Race-Free Equations for Estimated Glomerular Filtration Rate: Practical Guidance for Clinical Laboratories. Clin Chem. 2022 ;68(4): 511-20. https://dx.doi.org/10.1093/clinchem/hvab278.
- Малинова Л.И., Долотовская П.В., Фурман Н.В., Толстов С.Н., Клочков В.А., Денисова Т.П. Оценка метаболического бремени в свете концепции сосудистого старения при артериальной гипертензии (исследование трудоспособного населения крупного промышленного центра). Артериальная гипертензия. 2023; 29(1): 24-37. [Malinova L.I., Dolotovskaya P.V., Furman N.V., Tolstov S.N., Klochkov V.A., Denisova T.P. Estimation of metabolic burden within the concept of vascular ageing in hypertension(a study of the able-bodied population of a large industrial center). "Arterial’naya Gipertenziya" ("Arterial Hypertension"). 2023; 29(1): 24-37. (in Russian)]. https://dx.doi.org/10.18705/1607-419X-2023-29-1-24-37.
- Lloyd-Jones D.M., Allen N.B., Anderson C.A.M., Black T., Brewer L.C., Foraker R.E. et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation. 2022; 146(5): e18-e43. https://dx.doi.org/10.1161/CIR.0000000000001078.
- Silversides C.K., Grewal J., Mason J., Sermer M., Kiess M., Rychel V. et al. Pregnancy outcomes in women with heart disease: The CARPREG II Study. J. Am. Coll. Cardiol. 2018; 71(21): 2419-30. https://dx.doi.org/10.1016/j.jacc.2018.02.076.
- Lu C.W., Shih J.C., Chen S.Y., Chiu H.H., Wang J.K., Chen C.A. et al. Comparison of 3 risk estimation methods for predicting cardiac outcomes in pregnant women with congenital heart disease. Circ. J. 2015; 79(7): 1609-17. https://dx.doi.org/10.1253/circj.CJ-14-1368.
- Egeland G.M., Klungsoyr K., Oyen N., Tell G.S., Naess O., Skjaerven R. Preconception cardiovascular risk factor differences between gestational hypertension and preeclampsia: cohort norway study. Hypertension. 2016; 67(6): 1173-80. https://dx.doi.org/10.1161/HYPERTENSIONAHA.116.07099.
- Khan S.S., Brewer L.C., Canobbio M.M., Cipolla M.J., Grobman W.A., Lewey J. et al. Optimizing prepregnancy cardiovascular health to improve outcomes in pregnant and postpartum individuals and offspring: A Scientific Statement from the American Heart Association. Circulation. 2023;147(7): e76-e91. https://dx.doi.org/10.1161/CIR.0000000000001124.
Received 13.09.2024
Accepted 28.10.2024
About the Authors
Igor A. Salov, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia, https://orcid.org/0000-0002-1926-5418Lidia I. Malinova, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia, lidia.malinova@yandex.ru, https://orcid.org/0000-0002-0951-9314
Sergey N. Tolstov, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia, https://orcid.org/0000-0002-4546-9449
Alena A. Zhuk, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia, https://orcid.org/0000-0002-5236-0871
Tatyana P. Denisova, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia; https://orcid.org/0000-0003-4931-0969
Corresponding author: Lidia I. Malinova, lidia.malinova@yandex.ru