Innovative minimally invasive surgical treatment for partial hemivaginal aplasia with uterine and vaginal duplication. First Russian experience
Objective: To develop a minimally invasive surgical treatment for partial vaginal aplasia, including uterine duplication. Materials and methods: The study included 35 patients with partial vaginal aplasia of one of the duplicated uteruses who were treated at the Department of Pediatric and Adolescent Gynecology, V.I. Kulakov NMRC from June to December 2021. Of them, 20 patients underwent vaginorectoscopic opening of the hematocolposis and vaginoplasty using an improved technique. Results: The operation time with the developed technique averaged 43 (5) minutes versus 116 (3) minutes in the comparison group. Mean blood loss during vaginorectoscopic plasty was 14 (2) ml compared with 73 (18) ml during the classical method (p<0.05). No vaginal strictures were observed after surgery with the vaginorectoscopic technique. Conclusion: In patients with partial hemivaginal aplasia and uterine duplication, vaginorectoscopic vaginoplasty is a safe and effective surgical treatment.Batyrova Z.K., Uvarova E.V., Chuprynin V.D., Kumykova Z.Kh., Kruglyak D.A., Filippova E.A., Mamedova F.Sh., Kostyukov K.V., Asaturova A.V.
Keywords
Partial aplasia of one of the vaginas in patients with complete uterine and vaginal duplication and ipsilateral renal agenesis, known as Herlyn–Werner–Wunderlich Syndrome or Obstructed HemiVagina and Ipsilateral Renal Agenesis (OHVIRA) syndrome, is a rare congenital anomaly first reported by Purslow in 1922 [1]. Patients usually present after menarche with progressive dysmenorrhea and lower abdominal pain [2, 3]. Diagnosis may be difficult in most cases due to preserved menstrual function, and forms of this malformation accompanied by high aplasia of one of the vaginas usually end with removal of the uterus on the closed vaginal side due to the inability to form a complete vaginal artery.
Most researchers agree that early detection of genital malformations in girls and their timely treatment increase the chances of maintaining fertility in the future, so the need for surgical correction of internal genital malformations with outflow of menstrual blood disorders is without a doubt [1–5].
The traditional method of surgical correction is characterized by a high risk of traumatization of the bladder or rectum with subsequent bleeding and scarring. Drainage of the hematocolpos and excision of the closed vaginal wall with a scalpel and/or scissors followed by mucosal anastomosis are often difficult to perform due to the small size of the vagina, the location of a high colpos, and is always accompanied by instrumental defloration. sexual
Tsai et al (1998) reported the first case of endoscopic resection of the closed vaginal wall for uterine and vaginal duplication in an adolescent girl with no experience in sexual activity. The author used hysteroscopic resection of the vaginal septum to open the blocked hemivagina [6].
Later, Amagai and Cicinelli et al. (1999) described cases of endoscopic septotomy of the imperforate hemivagina in a newborn girl and an adolescent girl with uterine and vaginal duplication [7, 8].
In recent years, several studies have been published reporting successful vaginorectoscopy in girls with obstructive vaginal anomalies, including those with no experience in sexual activity [9, 10].
The disadvantage of the described approaches was the lack of control of incoming fluid loss and the impossibility to maintain optimal pressure in the working cavity, its uneven distribution in the hymenal margins, which reduced visualization quality and increased the risk of postoperative complications. In addition, preservation of the free edges of the mucosa of the dissected closed vagina, artificially created coagulation necrosis, and the presence of blind pockets increased the risk of strictures and infectious complications.
No techniques describing the possibility of surgical treatment of partial aplasia of one of the vaginas in uterine duplication using vaginorectoscopy could be found in the Russian literature.
This study aimed to develop a minimally invasive surgical treatment for partial vaginal aplasia, including uterine duplication.
Materials and methods
All stages of the presented study complied with the Russian Federation’s legislation, the international ethical norms and regulations of research organizations, and were approved by the Research Ethics Committee. Data analysis was performed after obtaining informed consent of the parent or legal representative and the patient for inclusion in the study.
From June to December 2021, 35 patients with partial aplasia of one of the vaginas in uterine and vaginal duplications were treated in the Department of Pediatric and Adolescent Gynecology of the V.I. Kulakov NMRC for OG&P. Complaints, physical (height, body weight, body mass index), and sexual development (sexual formula, gynecological and recto-abdominal examination data with assessment of the anomaly variant) were evaluated. After clinical and medical history and standard preoperative laboratory examination, 20 patients underwent vaginorectoscopic dissection of the closed hemivaginal wall with the creation of a combined vagina according to the developed technique, and 15 patients had vaginal opening and emptying of the hematocolpos with the formation of an oval window-type artery following the classical technique. After surgery, we assessed the total blood loss volume, operating time, and postoperative complaints of the patients.
Results
A clinical observation presents the technique developed for minimally invasive surgical treatment on the example of patient M., 11 y. o., with the diagnosis: genitourinary malformation. Duplication of the uterus and vagina. Distal aplasia of the right vagina. Hematocolpos. Hematocervix. Hematometra. The girl complained of periodic lower abdominal pain on days of menstruation with a tendency to increase.
Gynecological examination at admission: the external genitalia are formed according to age and sex, the hymen fimbriatus during rectal examination at a height of 2.0 cm from the anus, the lower pole of a tight elastic oval formation measuring 10×6 cm is palpated – hematocolpos.
On pelvic ultrasound examination, the uterus was duplicated (Fig. 1A), the right uterine body 49×28×54 mm, the right cervix 21×31 mm, myometrial echo structure was unchanged. The ureteral cavity was dilated to 10 mm (Fig. 1C), the cervical canal was dilated to 5 mm, the upper and middle third of the vagina was dilated to 104×51×68 mm (Fig. 1D). Contents heterogeneous; left uterine body 39×20 mm, left uterine cervix 26×18 mm, unchanged myometrial echostructure, non-dilated uterine cavity (Fig. 1B).
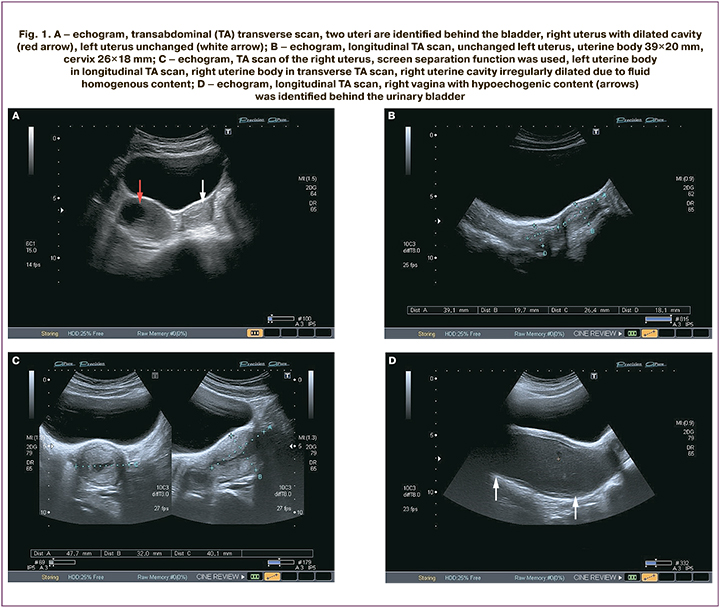
According to liquid vaginoscopy: pale pink vaginal mucosa, pronounced folding, pronounced swelling of the right vaginal wall mucosa – hematocolpos, cervix sharply deviated to the left, conic shape.
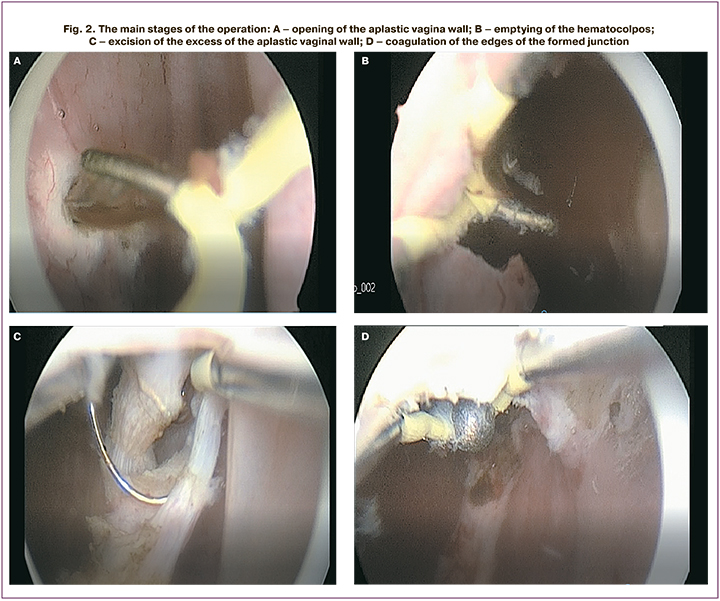
Treatment. A 26 Fr hysteroresectoscope was introduced into the vagina under constant dynamic ultrasound monitoring throughout the operation using aseptic techniques. To seal the vaginal cavity, we used a silicone bowl with an opening for the resectoscope on top. A natural latex medical device in the form of a small thin-walled elastic tube was placed in the bowel cavity and its distal part was fixed to the resectoscope tube using two vicryl sutures. The wide part of the cup in the folded state was conducted behind the hymenal ring, spread out, and created the effect of sealing the vagina during the examination to reduce the losses of the working solution and preserve the cavity of the overstretched vagina with low pressure. Using an L-shaped electrode, the walls of the closed vagina were dissected and flushed, followed by a cavity review (Fig. 2A, B). The location of the cervix and its position relative to the cervix of the second uterus with a functioning vagina were determined. The excess medial wall of the aplastic vagina was dissected using a curved resectoscope loop (Fig. 2С). Dissection was performed until the blind pockets of the united vagina were completely reduced. Additionally, hemostasis of the cut wall area was performed using the resectoscope balloon electrode (Fig. 2D). Hemostasis control was performed after reducing intravaginal pressure in the working medium. Additionally, at the end of the operation, a pad was placed in the combined vaginal cavity without tight tamponade with a solution of incomplete silver salt of polyacrylic acid. The total blood loss was less than 5 ml. The operation time was 45 minutes. The postoperative period was uneventful, no complications were observed. The results of control clinical and laboratory parameters and instrumental data (fluid vaginoscopy, ultrasound examination of the pelvic organs) did not deviate from the normal values. She was discharged from the hospital on the 7th day after surgical intervention without any complaints.
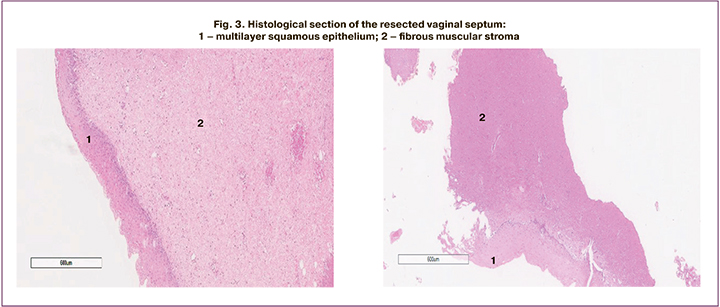
The 35 girls included in the study were comparable in age, anthropometric parameters, and pubertal development. The duration of vaginal resectoscopic repair averaged 43 (5) minutes versus 116 (3) minutes in the comparison group with the classic variant of surgery (p<0.05); the average blood loss during vaginorectoscopic repair was 14 (2) ml and 73 (18) ml during classical vaginal shaping (p<0.05). The resected septum was most often represented by fibrous tissue, lined in some places with mature multilayered squamous epithelium without signs of circulatory disorders and coagulation necrosis (Fig. 3).
All patients in the study group noted the absence of painful sensations on the 1st day after surgery according to the results of the postoperative pain assessment using the visual analogue scale.
To date, according to the results of face-to-face outpatient and remote (by telephone) counseling of all patients (100%), no signs of stricture of the created vagina have been noted.
Conclusion
The proposed method allows minimally invasive surgical treatment using endoscopic techniques, thus providing a complete restoration of menstrual outflow in girls with genital malformations. Furthermore, this method minimizes the risk of blood loss, preserves the integrity of the hymen, reduces the operating time and duration of the postoperative hospital stay, and improves the quality of medical care for this category of patients. The presented method of surgical treatment is extremely promising and requires further optimization and introduction into practice.
References
- Адамян Л.В., Фархат К.Н., Макиян З.Н. Комплексный подход к диагностике, хирургической коррекции и реабилитации больных при сочетании аномалий развития матки и влагалища с эндометриозом. Проблемы репродукции. 2016; 22(3): 84-90. [Adamyan L.V., Farkhat K.N., Makiyan Z.N. An integrated approach to the diagnosis, surgical correction and treatment of diseases during exacerbation of anomalies in the development of the uterus and vagina with endometriosis. Problems of Reproduction. 2016; 22(3): 84-90. (in Russian)].
- Крутова В.А., Наумова Н.В., Котлова Т.А., Тулендинова А.И., Асланян И.Э. Алгоритм диагностики и лечения девочек с врожденными пороками развития органов репродуктивной системы. Репродуктивное здоровье детей и подростков. 2015; 1: 30-6. [Krutova V.A., Naumova N.V., Kotlova T.A., Tulendinova A.I., Aslanyan I.E. Algorithm for the diagnosis and treatment of girls with congenital malformations of the organs of the reproductive system. Reproductive health of children and adolescents. 2015; 1: 30-6. (in Russian)].
- Albulescu D.M., Ceauşescu A.E., Sas L.M., Comănescu M.C., Constantin C., Tudorache Ş. The Herlyn-Werner-Wunderlich triad (OHVIRA syndrome) with good pregnancy outcome - two cases and literature review. Rom. J. Morphol. Embryol. 2018; 59(4): 1253-62.
- Беженарь В.Ф., Ярнова Е.А., Трофимова Т.Н. МРТ-диагностика аномалии мюллерова протока. Лучевая диагностика и терапия. 2012; 1(3): 99-103. [Bezhenar V.F., Yarnova E.A., Trofimova T.N. MRI diagnostics of the anomaly of the Mullerian duct. Radiation diagnostics and therapy. 2012; 1(3): 99-103. (in Russian)].
- Ипатова М.В., Маланова Т.Б., Серов В.Н. Преформированные физические факторы в раннем послеоперационном периоде в гинекологии детского и юношеского возраста. Репродуктивное здоровье детей и подростков. 2009; 6: 48-55. [Ipatova M.V., Malanova T.B., Serov V.N. Preformed physical factors in the early postoperative period in pediatric and adolescent gynecology. Reproductive health of children and adolescents. 2009; 6: 48-55. (in Russian)].
- Tsai E.M., Chiang P.H., Hsu S.C., Su J.H., Lee J.N. Hysteroscopic resection of vaginal septum in an adolescent virgin with obstructed hemivagina. Hum. Reprod. 1998; 13(6): 1500-1. https://dx.doi.org/10.1093/HUMREP/13.6.1500.
- Amagai T., Ohkawa H., Kaneko M. Endoscopic septotomy: a new surgical approach to infantile hydrometrocolpos with imperforate hemivagina and ipsilateral renal agenesis. J. Pediatr. Surg. 1999; 34(4): 628-31.https://dx.doi.org/10.1016/s0022-3468(99)90091-x.
- Cicinelli E., Romano F., Didonna T., Schonauer L.M., Galantino P., Di Naro E. Resectoscopic treatment of uterus didelphys with unilateral imperforate vagina complicated by hematocolpos and hematometra: case report. Fertil. Steril. 1999; 72(3): 553-5. https://dx.doi.org/10.1016/s0015-0282(99)00270-8.
- Ludwin A., Ludwin I., Bhagavath B., Martins W.P., Lindheim S.R. Virginity-sparing management of blind hemivagina in obstructed hemivagina and ipsilateral renal anomaly syndrome. Fertil. Steril. 2018; 110(5): 976-8.https://dx.doi.org/10.1016/j.fertnstert.2018.07.007.
- Cheng C., Subedi J., Zhang A., Johnson G., Zhao X., Xu D., Guan X. Vaginoscopic incision of oblique vaginal septum in adolescents with OHVIRA syndrome. Sci. Rep. 2019; 9(1): 20042. https://dx.doi.org/10.1038/s41598-019-56471-2.
Received 06.06.2022
Accepted 24.06.2022
About the Authors
Zalina K. Batyrova, PhD, Senior Researcher at the Department of Pediatric and Adolescent Gynecology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-85-42, linadoctor@mail.ru, https://orcid.org/0000-0003-4997-6090, 4, Oparina str., 117997, Moscow, Russia.Elena V. Uvarovа, Corresponding member of the RAS, Dr. Med. Sci., Professor, Head of the Department of Pediatric and Adolescent Gynecology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia; President of Interregional Public Organization "Association of Pediatric and Adolescent Gynecologists"; Professor at the Department of Obstetrics, Gynecology, Perinatology and Reproductology, Institute of Professional Education, +7(495)438-85-42, elena-uvarova@yandex.ru,
https://orcid.org/0000-0002-3105-5640, 4, Oparina str., 117997, Moscow, Russia.
Vladimir D. Chuprynin, PhD, Head of the Surgical Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-85-42,
v_chuprynin@oparina4.ru, 4, Oparina str., 117997, Moscow, Russia.
Zaira Kh. Kumykova, PhD, Senior Researcher at the Department of Pediatric and Adolescent Gynecology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health
of Russia, +7(495)438-85-42, zai-kumykova@yandex.ru, https://orcid.org/0000-0001-7511-1432, 4, Oparina str., 117997, Moscow, Russia.
Diana A. Kruglyak, doctor at the Department of Pediatric and Adolescent Gynecology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
+7(495)438-85-42, diana.kruglyak@yandex.ru, 4, Oparina str., 117997, Moscow, Russia.
Elena A. Filippova, PhD, Head of the Department of Ultrasound Diagnostics in Neonatology and Pediatrics, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health
of Russia, +7(495)438-85-42, fla77@mail.ru, 4, Oparina str., 117997, Moscow, Russia.
Fatima Sh. Mamedova, PhD, doctor at the Department of Ultrasound Diagnostics in Neonatology and Pediatrics, Academician V.I. Kulakov NMRC for OG&P, Ministry
of Health of Russia; Аssistant at the Department of Radiation Diagnostics of Children, Russian Medical Academy of Continuing Professional Education, Ministry of Healthcare of Russia, +7(495)438-85-42, fmamedova@yandex.ru, ttps://orcid.org/0000-0003-1136-7222, 4, Oparina str., 117997, Moscow, Russia.
Kirill V. Kostukov, Dr. Med. Sci., Head of the Department of Functional and Ultrasound Diagnostics, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-85-42, kostyukov_k@yahoo.com, 4, Oparina str., 117997, Moscow, Russia.
Aleksandra V. Asaturova, PhD, Head of the Department of Anatomic Pathology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-23-11, a.asaturova@gmail.com, https://orcid.org/0000-0001-8739-5209, 4, Oparina str., 117997, Moscow, Russia.
Authors' contributions: Batyrova Z.K., Chuprynin V.D., Uvarova E.V., Kumykova Z.Kh. – conception and design of the study; Batyrova Z.K., Uvarova E.V., Chuprynin V.D., Kumykova Z.Kh., Kruglyak D.A., Filipova E.A., Mamedova F.S., Kostyukov K.V., Asaturova A.V. – data collection and analysis; Batyrova Z.K. – manuscript drafting; Kumykova Z.Kh. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P.
Patient Consent for Publication: All patients provided informed consent for the publication of their data and associated images.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Batyrova Z.K., Uvarova E.V., Chuprynin V.D., Kumykova Z.Kh., Kruglyak D.A., Filippova E.A., Mamedova F.Sh., Kostyukov K.V., Asaturova A.V. Innovative minimally invasive surgical treatment for partial hemivaginal aplasia with uterine and vaginal duplication.
First Russian experience.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 7: 75-80 (in Russian)
https://dx.doi.org/10.18565/aig.2022.7.75-80