Giant follicular cyst in a teenage girl
Background. According to different authors, in the pattern of gynecological morbidity in children and adolescents, the proportion of ovarian tumors and tumor-like masses varies widely from 1 to 19.2%, and the overwhelming majority of these are benign. Tumor-like masses (50–60%) are rather more common than ovarian tumors (40–49.5%), whereas giant ovarian neoplasms are rare. There are found publications that the giant ovarian mass is inherently cystadenoma that sometimes reaches the size of the uterus with a full-term fetus. A giant ovarian follicular cyst is very rarely mentioned.Kyurdzidi S.O., Khashchenko E.P., Uvarova E.V., Chuprynin V.D., Asaturova V.A., Tregubova A.V.
Case report. The paper describes a rare clinical case of a giant follicular ovarian cyst in a 14-year-old girl. A mass of 35 cm in diameter was found due to the increased abdominal size in the teenager; a follicular ovarian cyst was confirmed histologically. Clinical features and management tactics are analyzed in comparison to the data currently available in the literature on giant ovarian masses in childhood.
Conclusion. The described clinical case proves the importance of regular preventive examinations, including complex ultrasound examination in teenage girls, in order to early diagnose ovarian mass and to timely perform organ-sparing surgery.
Keywords
Ovarian neoplasms in children are most often diagnosed during puberty. This is due to the increase in gonadal activity and the formation of full menstrual cycles at this time of a girl’s life [1]. Benign ovarian tumors of large size tend to stretch the ovarian tissue from the inside or compress and deform it from the outside, which undoubtedly poses an additional risk to the ovarian reserve as it is limited and cannot be restored.
According to different studies, the incidence of ovarian tumors and tumor-like masses varies widely from 1–4.6% [2, 3] and 7.5–19.2% [1] among other gynecological pathologies in children and adolescents. The proportion of ovarian neoplasms in adolescent girls does not exceed 2%, which means that most of them are benign. Moreover, tumor-like masses are more common (50–60%) than ovarian tumors (40–49.5%) [2].
Tumor-like masses, unlike ovarian tumors, do not result from the proliferation of cellular elements and the growth of the tissue of the masses, but they form due to the accumulation of fluid in a particular cavity. If fluid accumulates in the follicle, a follicular cyst is formed; a luteal cyst is formed in the cavity of the corpus luteum; and a paramesonephric cyst is formed in the remaining cells of the paramesonephric ducts [1]. Follicular cysts are lined with granulose, often flattened, cells or have lining containing theca cells [4]. Such masses, in comparison with ovarian tumors, may undergo regression during the menstrual cycle or drug therapy [1].
Torsion of the uterine adnexa, which is often associated with the mass formation, causes acute abdominal pain in children in about 15% of cases [1]. The presence or suspicion of torsion of the uterine adnexa requires urgent differential diagnostic and therapeutic measures [2]. The developed algorithm for diagnosing cysts in the abdominal cavity, including ultrasound examination of the pelvic organs, Doppler blood flow mapping, analysis of the concentration of cancer markers, computer tomography and magnetic resonance imaging (CT and MRI), allows us to identify the character of masses and choose appropriate surgical tactics [4]. The most common method for treating ovarian tumors is an organ-sparing surgery, which makes it possible to maintain the ovarian reserve to the maximum.
Due to the improved imaging techniques, pelvic neoplasms are now diagnosed and treated more often at an early stage. However, adolescent girls with benign cysts of giant size in the abdominal cavity are also found among those who live in large cities with hospitals having sufficient diagnostic capabilities.
Many questions concerning the tactics of examination and treatment of girls with giant tumors and tumor-like masses in the abdominal cavity are still debated. Massive formations of the ovaries can imitate ascites. Therefore, it is necessary to determine clearly the sonographic signs of cystic masses, or, in case of doubts, MRI should be done for verification of the diagnosis. Performing paracentesis in ascites with transabdominal aspiration in case of undiagnosed ovarian cyst can lead to serious life-threatening complications. In order to preserve fertility, the most proper surgical treatment is cystectomy with the maximum preservation of ovarian tissue. However, it is necessary for the patient to undergo regular follow-up by a gynecologist due to the risk of recurrence after conservative surgery.
We present a unique clinical observation of a 14-year-old girl with chronic pelvic pain associated with a giant mass of the right ovary, which turned out to be a follicular ovarian cyst.
Clinical observation
A 14-year-old patient presented to pediatric and adolescent gynecologist at the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Moscow, Russia (hereinafter referred to as the Center) in February 2020. She complained of acute pain in the lower abdomen when moving, painful urination in small portions, dizziness and nausea. According to the ultrasound examination of the pelvic organs performed at her local clinic, the girl was diagnosed with an ovarian mass with a diameter of 15 cm, and this was the reason for referring her to the Center for consultation. Taking into account the data of the ultrasound examination and clinical manifestations, the girl was urgently hospitalized in the 2nd Gynecological Department (Pediatric and Adolescent) with a suspicion of torsion of the uterine adnexa.
When analyzing the medical information, it was found out that a cystic mass with fluid in the right ovary measuring 40x30 mm was first detected in May, 2019 during the ultrasound examination of the pelvic organs. In order to clarify the examination and treatment, hospitalization was recommended, which was refused by the patient’s family. In June 2019, the patient repeatedly visited the gynecologist at the local clinic with complaints of irregular menstrual cycle and bleeding from the genital tract. According to the ultrasound examination of the pelvic organs, a cystic mass with fluid in the right ovary of the previous size was again detected. The patient was prescribed a microdose combined oral contraceptive containing 20 mcg of ethinylestradiol and 3 mg of drospirenone, which was taken by the patient until the end of December, 2019. It was in this month that the girl first noticed an increased abdomen size, but the family did not pay attention to this. Nine days before being admitted to the Center, the girl had a pain in the lower abdomen, which caused her family to visit a doctor at their local clinic. An ultrasound examination of the pelvic organs revealed a cystic mass with fluid in the right ovary measuring 150x98x100 mm. The doctor from the local clinic prescribed her dydrogesterone (duphaston) at the dose of 20 mg/day for 10 days and rectal suppositories with indomethacin at the dose of 50 mg/day. The control ultrasound examination the day before hospitalization revealed an increase in the mass up to size 216x145x146 mm.
Surgical and family histories were not remarkable, according to the girl’s mother. Among the past diseases, there were frequent acute respiratory viral infections, rotavirus infection, chickenpox, furunculosis, bronchial asthma, and atopic dermatitis. An allergic reaction occurred in contact with animals, iodine containing drugs and in season of spring and autumn pollinosis, and could have different manifestations including Quincke’s edema. The patient was not performed any hemotransfusions. She denied any bad habits. Menarche was at the age of 12 years, the menstrual cycle was not regulated, with menstruation delays for up to several months. Menstrual bleeding was moderate, and it was painful in the first days. She was admitted to hospital on the 44th day of the menstrual cycle. According to her words, she was not sexually active.
On admission to the hospital, the girl’s condition was assessed as satisfactory. She had normal consciousness. The girl complained of pain in the lower abdomen and difficult urination. The skin and visible mucous membranes were clean, they had a normal color and moistness. Body temperature was 36.6°C. Her height was 174 cm, and her weight was 67 kg. Body mass index was 22 kg/m2. The tongue was clean and moist. Physical and sexual maturity was consistent with her age, and the formula for sexual development was B (Breast) 4, P (Pubis) 5 using the Tanner scale. The thyroid gland was not palpated, and there were no symptoms of its disorder. Submandibular and cervical lymph nodes were not changed. The mammary glands were soft, the nipples were clean and normal, and there were no discharges from the nipples. Vital signs were stable: regular breathing, vesicular breathing, no wheezing, respiratory rate was 14 per minute; heart tones were sonorous and rhythmic, heart rate was 78 beats per minute; pulse rate was satisfactory; blood pressure on the left arm was 110/75 mmHg; on the right arm it was 110/70 mmHg.
The abdomen was enlarged, its circumference was 90 cm, which corresponds to 32 weeks of pregnancy; the abdomen was tense and tender in the lower parts. On palpation, the abdomen was rounded, its upper border was 3 cm below the xiphoid process. On percussion of the abdomen, a dull sound was detected in all areas of the abdominal cavity. There were no symptoms of peritoneal irritation. Pasternatsky symptom was negative on both sides. The stool was formed.
External genitals were formed according to the age and gender. The clitoris was not enlarged. The urethra had a typical location. The hymen was fimbriated and intact. Rectal examination was complicated by the presence of a large mass in the abdominal cavity.
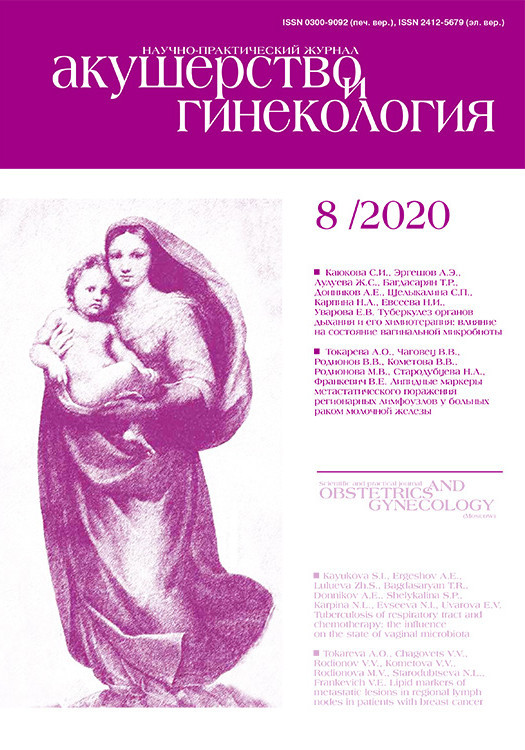
The ultrasound examination of the pelvic organs revealed a cystic mass with fluid over the bladder; it had thick layered walls, an uneven internal contour, measuring 17x9x23 cm, and a volume of about 1840 cm3. Behind the cystic mass, there was the uterus with smooth, clear contours, measuring 48x32x40 mm (body) and 32x20 mm (cervix), without any structural changes in the myometrium and endometrium; the uterus was displaced to the right from the midline. The left ovary was located in the corner of the uterus, measuring 27x14x22 mm and a volume of 4.4 cm with small 4-5 follicles in the section. The right ovary was not separately identified. Free fluid in the abdominal cavity was not detected. According to the Doppler examination, single pixels of blood flow along the periphery of the neoplasm were visualized (Fig. 1). The echographic diagnosis was a giant neoplasm of the right ovary. Torsion of the right adnexa of the uterus was suspected.
Clinical and biochemical blood tests and urinalysis were within physiological range: leucocytes = 6.38х109/L; erythrocytes = 4.78х1012/L; hemoglobin = 132 g/L; hematocrit = 37.7%; thrombocytes = 304х109/L; total protein = 77 g/L; glucose (in serum) = 4.9 mmol/L; urea = 3.1 mmol/L; creatinine = 66.9 mmol/L; total bilirubin = 5.5 mmol/L; direct bilirubin = 2.4 mmol/L; lactate dehydrogenase = 369.2 units/L; C-reactive protein = 1.66 mg/L.
Small changes were detected in the coagulogram: Clauss fibrinogen level increased to 4.24 g/L; prothrombin time – 12 sec; international normalized ratio – 1.0; activated partial thromboplastin time – 26.5 sec; thrombin time – 21.3 sec.
Cancer markers: cancer antigen CA-125 was 30.49, normal values are 0–35 U/ml; cancer antigen CA 19-9 was 9.09, normal values are 0–37 U/ml; cancer-embryonic antigen was 0.6, normal values are 0–5 ng/ml; neuron-specific enolase was 14.01, normal values are 0–20 ng/ml; alpha-fetoprotein was 2.9, normal values are 0–10 IU/ml; human chorionic gonadotropin was <0.500 with normal values of 0-10 IU/ml.
The hormonal status corresponded to the age-appropriate normal value, except for the level of anti-Muller hormone, which exceeded the age values by three times, namely 23.8 ng/L.
According to the results of patient’s history, examination, clinical and laboratory-instrumental studies, a clinical diagnosis was made: a giant neoplasm of the right ovary. Torsion of the right ovary was suspected. The patient was administered emergency surgical treatment. The patient and her parents were explained the diagnosis and the chosen tactics, they were warned about possible laparotomic access and increased extent of surgery and possible risk of ovariectomy. Informed written consent was obtained from the girl’s legal representative.
The surgery was performed under endotracheal anesthesia. The abdominal puncture and subsequent incision for the insertion of the laparoscope tube were performed 3 cm below the xiphoid process. However, it was not possible to insert a central trocar with a laparoscope into the abdominal cavity due to the direct proximity of the wall of the neoplasm to the wound. It was decided to perform an access through a lower midline incision. When opening the abdominal cavity, it was found that the cystic mass of an ellipsoid shape had a size of about 30x25 cm, a smooth surface, a tight elastic consistency and occupied the abdominal cavity by more than 2/3 of its volume. On the anterior surface of the mass, there were spots of dark grey and bluish color, which were signs of impaired blood circulation in the ovary.
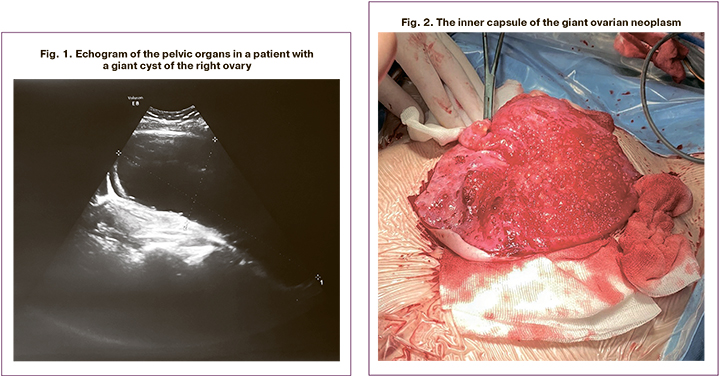
The abdominal cavity was insulated with gauze along the side channels on both sides, the neoplasm was pulled up to the edges of the surgical incision. A purse-string suture was used to sew the capsule of the neoplasm superficially without penetrating into the cavity. An incision of the capsule was made inside the purse-string suture. The contents of the neoplasm were aspirated gradually, with intervals of two minutes, which provided a slow restoration of blood flow in the aorta and large vessels of mesenterium. A total of 2,800 ml of light yellow fluid with an admixture of mucin was evacuated. During the inspection of the abdominal cavity, it was found that the cystic mass originated from the right ovary. The decreased neoplasm was turned out on the anterior abdominal wall covered with a protective film. Additionally, the abdominal cavity was insulated with gauze and a diaper. The cyst capsule was opened again and the remaining fluid was evacuated. The inner wall of the neoplasm with injected vessels over the entire surface was covered with a variety of vesicular masses ranging in size from 0.2 to 1.0 cm with transparent contents (Fig. 2).
The neoplasm was totally excised and separated from the surrounding ovarian tissue. The bed was coagulated, and a separate vicryl suture was applied to the bleeding vessel in the area of the ovarian hilus. When examining the right ovary, it was found that most of its tissue does not contain tertiary follicles and its thickness does not exceed 2 mm. Small tertiary follicles were detected only at the ovarian hilus. It was decided to perform a resection of the ovary preserving the ovarian tissue for 4 cm from the ovarian hilus. The edges of the ovary were connected with vicryl sutures.
During the control inspection of the abdominal cavity, it was found that the uterus was located along the middle line, it had a normal color and shape, measuring 3.8x2.8x4.3 cm. On the left and right, the inside of the fallopian tubes was visible throughout, the ampullary sections were free, and the fimbriae were expressed. The right resected ovary had normal color; its blood vessels were not bleeding. The left ovary, measuring 2.5x3.0x2.0 cm had a whitish capsule and the tertiary follicles with a diameter from 3 to 8 mm were visible through it. Rectouterine space was free. Other pathological masses in the true pelvis were not detected. Organs of the upper abdominal cavity were normal, the parietal and visceral peritoneum was smooth, the capsule of the liver and spleen was smooth, the greater omentum did not have any visible pathology, and the paraaortic lymph nodes were not enlarged. The lavage of the abdominal cavity was performed and hemostasis was monitored; hemostasis was defined as stable. The wound of the abdominal wall was sutured in layers. Intradermic suture was applied to the skin wound edges. Adhesive dressing was applied to the skin.
On the second day after the operation, the patient noted the appearance of menstrual discharge from the genital tract (on the 47th day from the previous menstruation). The discharge lasted 3.5 days and did not require hemostatic therapy. During the time the patient was in the hospital, she received complex antibacterial, infusion, anti-inflammatory and analgesic therapy, as well as preventive treatment for thromboembolic complications. The postoperative period proceeded without complications; surgical incisions healed by primary tension. The patient was discharged in a satisfactory condition. During the discharge, there was a decrease in body weight by 4 kg and a decrease in the size of the abdomen. The girl’s parents were given recommendations for repeated ultrasound examination of the pelvic organs 30 days after the operation; they were told about the need to monitor the menstrual cycle and visit a gynecologist with the data of the ultrasound examination of the pelvic organs. During the control visit, the pathology of the uterus and its adnexa was not detected, menstruation occurred 30 days after the previous one which was in the hospital after the operation.
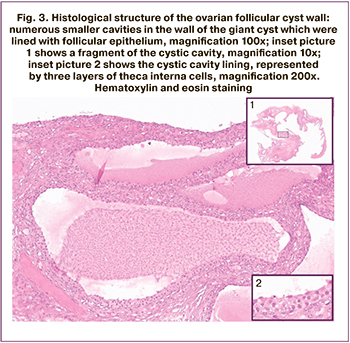 According to the results of a pathomorphological study, the capsule of the ovarian cyst was lined from the inside with a multilayered follicular epithelium with indistinct basal membrane between the follicular cells and adjacent layers of luteinized internal theca cells. In the loose stroma, one could see the lumen of capillaries and small blood vessels, and on the inner surface of the capsule there were numerous cavities that were similar to small vesicles. Each cavity of the vesicle was lined from the inside with a layer of small cells identical in structure to the follicular epithelium of the main cyst and contained a slightly colored secretion. Oocytes were not detected in any of the examined follicular cavities. This pattern was suggestive of a multifocal follicular cyst (Fig. 3).
According to the results of a pathomorphological study, the capsule of the ovarian cyst was lined from the inside with a multilayered follicular epithelium with indistinct basal membrane between the follicular cells and adjacent layers of luteinized internal theca cells. In the loose stroma, one could see the lumen of capillaries and small blood vessels, and on the inner surface of the capsule there were numerous cavities that were similar to small vesicles. Each cavity of the vesicle was lined from the inside with a layer of small cells identical in structure to the follicular epithelium of the main cyst and contained a slightly colored secretion. Oocytes were not detected in any of the examined follicular cavities. This pattern was suggestive of a multifocal follicular cyst (Fig. 3).
Discussion
Among tumor-like masses in adolescents, follicular cysts are the most common. They occur due to the imperfection of the ovulation process and/or the persistence of the follicle. According to the analysis of scientific literature, the average age of patients with giant benign ovarian tumors is 14.28±1.72 years; ovarian cysts in 57% of cases were represented by cystadenoma [5, 6–8, 9–11], teratoma in 29% [12–15], and follicular cyst in 7% [16] of cases. The left ovary is affected more often [7, 9, 11, 13, 14,16, 17]. Usually such cysts have a diameter of 2 to 3 cm and regress in the second half of the menstrual cycle. If ovulation does not occur, as a rule follicular cysts can grow in diameter to a maximum of 8–10 cm. Giant follicular cysts, as in the presented case, are described in occasional scientific articles. The average size of the described neoplasms was 31.07±7.51 x 22.79±5.9 x 22.91±7.79 cm, and the volume of evacuated contents corresponded to 6.66 ± 3.21 L. When analyzing international reference databases («PubMed»,
«Scopus», «Elibrary») on the issues of clinic, diagnosis and treatment of the giant ovarian cysts of different types in adolescents, published over the past five years, it was revealed that such neoplasms are still found in countries with different levels of medical development: Russia [8, 10–12], India [16], Pakistan [6], Turkey [7], Qatar [8], Japan [9, 14], Italy [10, 11], and Egypt [15]. It seems that there is no adequate level of public awareness about possible types of gynecological diseases in children and adolescents, their etiology and consequences. Therefore, the demonstrated clinical case should be of interest to specialists.
An obvious clinical sign of the giant ovarian cysts is a sharp increase in the size of the abdomen [1, 3, 10], which can be accompanied by pain over the uterus or in the iliac areas [4, 12] with nausea and vomiting [4, 5]. The painless course of the disease is also possible [8]. Abdominal pain can be caused by one or more factors: stretching of the mesenterium, the albumen of the ovary, the ligamentous apparatus of the uterine adnexa, as well as the pressure of cysts on adjacent organs. In some cases, there was a description of the clinic of partial intestinal obstruction and blood supply disorders in the neoplasm due to the torsion of the cyst pedicle [4]. The patients also complained of menstrual irregular cycle [6, 7, 9, 16], shortness of breath [6, 12], and constipation [6, 7, 10, 14], discomfort during urination [11], which may be associated not only with compression of the bladder, but also with hydronephrosis, and expansion of the ureter [16]. On palpation of the enlarged abdomen, a symptom of fluctuation can be noted [6, 8, 12].
Despite the advanced technologies of instrumental research, sometimes it is difficult to determine the location of the cyst [7]. Therefore, such preliminary diagnoses as ascites [8,12] and intestinal disorders [11] are made. An incorrect diagnosis can lead to erroneous treatment tactics, such as recommendations to control the caloric content of the diet in order to reduce body weight [5].
In most cases, the laboratory parameters correspond to physiological standards, but this does not exclude the importance of a comprehensive examination of the patient. Nowadays, the identification of cancer markers is an available method of examination [5, 9, 12, 14, 16], which absolutely changes the strategy for further management and treatment.
According to the literature, the average duration of the presence of a noticeable or disproportionate increase in the size of the abdomen before seeking medical help is from 4.7±5.67 to a maximum of 18 months [8]. In the clinical observation presented in this article, the girl noticed a significant increase in the abdomen about 3 months ago, but the pain and menstrual disorders first appeared 9 months ago, for which she was administered a long-term hormone treatment in the local clinic. Pain in the lower abdomen, dizziness and nausea caused urgent hospitalization. Also, an increase in the abdomen to the size of a full-term pregnancy and pain syndrome were accompanied by dysuria. The difficulty at the preoperative stage was in the differential diagnosis of benign and malignant ovarian neoplasms. The signs of suspected torsion of the uterine adnexa required emergency surgical management tactics; satisfactory laboratory results were suggestive of the presence of a benign tumor or a tumor-like process.
Care for the ovarian reserve of women of early reproductive age involves the most careful cystectomy for the purpose of rational preservation of ovarian tissue. Despite this, surgical intervention in the giant cysts should involve oncological alertness and urgent histological examination of a part or whole of the cyst for the final choice of extent of the surgery.
The use of endoscopic and open access in the treatment of giant ovarian cysts is controversial. Anatomical and topographical characteristics of children can limit the surgical field and present difficulties for manipulation, therefore laparoscopic access is still a preferable one. Reducing postoperative pain and wound infection, improving cosmetic results and postoperative rehabilitation in fewer hospital days are some of the most noticeable advantages of endoscopic surgery, which defines it as the standard in the treatment of benign ovarian cysts. However, the size of ovarian neoplasm and the clinical picture are the circumstances that should not be ignored when choosing open surgical access by laparotomy. According to the literature, open access was used in 79% of girls including lower midline laparotomy in 43% [5, 6, 8, 13, 15, 17] or laparotomy by Pfanenstiel in 36% of cases [9, 11, 14, 16]. The laparoscopic method was used only in 21% of young patients [7, 10, 12]. Regardless of the operative technique, affected ovarian tissue could not be preserved in half of the cases [ 5, 9, 11, 12, 15, 17].
The presented clinical observation is a clear demonstration of a rare tumor-like mass (giant follicular cyst) of the ovary in an adolescent girl. Due to the increasing size of the abdomen, children are more often taken to see pediatricians; the primary task of each doctor is to exclude intra-abdominal tumor growth originating from the genitals. The neoplasm revealed by the ultrasound examination of the pelvic organs requires a consultation and dynamic observation by a gynecologist. Moreover, the presented clinical observation demonstrated the necessity of proper management of the girl by a gynecologist, which enables to avoid irrational treatment with hormonal drugs and to send a girl with ovarian neoplasm to a hospital for operative organ-sparing treatment.
Conclusion
The presented clinical case proves the necessity of preventive examinations of adolescent girls in order to diagnose early ovarian growths and preserve fertility in women of early reproductive age. In case of timely surgical treatment, the possible risks and complications will be minimal.
References
- Савельева Г.М., Сухих Г.Т., Серов В.Н., Радзинский В.Е., Манухин И.Б., ред. Гинекология. Национальное руководство. М.: ГЭОТАР-Медиа; 2019: 345-61, 973-8. [Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E., Manukhin I.B., ed. Gynecology: national guideline. GEOTAR-Media; 2019: 345–61, 973–8. (in Russian)].
- Гуркин Ю.А., Рухляда Н.Н. Гинекология детского и подросткового возраста. Руководство для врачей. М.: МИА; 2019: 239-47. [Gurkin Yu.A., Rukhlyada N.N. Pediatric and Adolescent Gynecology: A Guide for Physicians. Moscow: Medical Information Agency LLC; 2019: 239-47. (in Russian)].
- Уварова Е.В. Детская и подростковая гинекология. Руководство для врачей. М.: Литтерра; 2009: 375-83. [Uvarova E.V. Pediatric and adolescent gynecology: a guide for doctors. Moscow: Litterra; 2009: 375–83. (in Russian)].
- Адамян Л.В., Поддубный И.В., Глыбина Т.М., Федорова Е.В. Лапароскопия при кистах яичника и брюшной полости у девочек. М.: ГЭОТАР-Медиа; 2007. 104 с. [Adamyan L.V. et al. Laparoscopy for ovarian and abdominal cysts in girls. Moscow: GEOTAR-Media, 2007.104 p. (in Russian)].
- Соломатина А.А., Караченцова И.В., Волкова П., Мызин А.В., Логачева Т.М. Клинический случай гигантской муцинозной цистаденомы у девочки-подростка. Репродуктивное здоровье детей и подростков. 2019; 15(3): 99-106. [Solomatina A.A., Karachentsova I.V. et al. A clinical case of giant mucinous cystadenoma in a teenage girl. Reproductive health of children and adolescents. 2019; 15(3): 99-106. (in Russian)].
- Mehboob M., Naz S., Zubair M., Kasi M.A. Giant ovarian cyst – an unusual finding. J. Ayub Med. Coll. Abbottabad. 2014; 26(2): 244-5.
- Kilincaslan H., Cipe G., Aydogdu I., Sarac F., Toprak H., Ari E. Pure laparoscopic management of a giant ovarian cyst in an adolescent. Am. J. Case Rep. 2014; 15: 4-6. https://dx.doi.org/10.12659/AJCR.889769.
- Mohammed Elhassan S.A., Khan S., El-Makki A. Giant ovarian cyst masquerading as massive ascites in an 11-year-old. Case Rep. Pediatr. 2015; 2015: 10.1155/2015/878716. https://dx.doi.org/10.1155/2015/878716.
- Watanabe S., Nagashima S., Onagi C., Yamazaki N., Shimada S., Sakai M. et al. Treatment strategy for pediatric giant mucinous cystadenoma: A case report. Pediatr. Rep. 2019; 11(3): 8190. https://dx.doi.org/10.4081/pr.2019.8190.
- Corrias F., Pederiva F., Cozzi G., Ammar L., Cattaruzzi E., Lembo M.A., Barbi E. A giant ovarian cyst in an adolescent. J. Pediatr. 2018; 199: 279. https://dx.doi.org/10.1016/j.jpeds.2018.03.015.
- Persano G., Severi E., Cantone N., Incerti F., Ciardini E., Noccioli B. Surgical approach to giant ovarian masses in adolescents: Technical considerations. Pediatr. Rep. 2018; 10(3): 43-5. https://dx.doi.org/10.4081/pr.2018.7752.
- Спиридонов А.А. Лапароскопическая операция при гигантской тератоме яичника. Российский вестник детской хирургии, анестезиологии и реаниматологии. 2015; 5(3): 51-4. [Spiridonov A.A. Laparoscopic surgery for giant ovarian teratoma. Russian Bulletin of Pediatric Surgery, Anesthesiology and Resuscitation. 2015; 5(3): 51-4. (in Russian)].
- Цхай В.Б., Брехова И.С., Котова О.И., Андреева А.А., Домрачева М.Я., Коновалов В.Н., Ковтун Н.М. Клинический случай гигантской тератомы яичника у юной пациентки. Сибирское медицинское обозрение. 2015; 2: 95-8. [Tskhai V.B. et al. Clinical case of giant ovarian teratoma in a young patient. Siberian Medical Review. 2015. 2015; 2: 95-8. (in Russian)].
- Yasui T., Suzuki T., Hara F., Watanabe S., Tomishigeet H. et al. Minimal laparotomy management of a giant ovarian cystic teratoma in adolescence. JSLS. 2015; 3(6): 239-41.
- Abbas A.M., Gamal E., Talaat E., Sheha A.M. Torsion of huge dermoid cyst in adolescent girl: A case report. Middle East Fertil. Soc. J. 2017; 22(3): 236-9.
- Rajput D., Gedam J., Bhalerao M., Nadar P.A. Giant follicular cyst of ovary in an adolescent girl. J. Clin. Diagn. Res. 2014; 8(7): OD03-4. https://dx.doi.org/10.7860/JCDR/2014/8649.4542.
- Цхай В.Б., Андреева А.А., Блинова Е.Н., Ульянова И.О., Котова О.И., Журавлев С.В. Клинический случай гигантской гранулезоклеточной опухоли яичника. Сибирское медицинское обозрение. 2014; 2: 86-9. [Tskhai V.B. et al. Clinical case of a giant granulosa cell tumor of the ovary. Siberian Medical Review. 2014; 2: 86-9. (in Russian)].
Received 12.05.2020
Accepted 18.05.2020
About the Authors
Stanislav O. Kyurdzidi, postgraduate student of I.M. Sechenov First Moscow State Medical University (Sechenov University) Ministry of Healthcare of the Russian Federation. E-mail:dr.kyurdzidis@gmail.com. ORCID: 0000-0002-6316-1325. 2, Trubetskaya str., Moscow, 119991, Russia.Elena V. Uvarova, Doctor of Medical Sciences, Professor, Corresponding Members of the RAS, Head of 2nd Gynecological (child and adolescent) Department, National Medical Research Сenter for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov Ministry of Healthcare of the Russian Federation.
E-mail: elena-uvarova@yandex.ru. ORCID: 0000-0002-3105-5640. 4, Ac. Oparina str., Moscow, 117997, Russia.
Elena P. Khashchenko, PhD, Researcher of Gynecology of children and adolescents Department, National edical Research Сenter for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov Ministry of Healthcare of the Russian Federation. E-mail: khashchenko_elena@mail.ru ORCID: 0000-0002-3195-307X.
4, Ac. Oparina str., Moscow, 117997, Russia.
Vladimir D. Chuprynin, PhD, Head of General Surgery department, National edical Research Сenter for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov Ministry of Healthcare of the Russian Federation. E-mail: v_chuprynin@oparina4.ru. 4, Ac. Oparina str., Moscow, 117997, Russia.
Aleksandra V. Asaturova, PhD, Head of 1th Pathology Department, National edical Research Сenter for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov Ministry of Healthcare of the Russian Federation. E-mail: a_asaturova@oparina4.ru. ORCID: 0000-0001-8739-5209. 4, Ac. Oparina str., Moscow, 117997, Russia.
Anna V. Tregubova, junior scientific researcher, 1th Pathology department, National edical Research Сenter for Obstetrics, Gynecology and Perinatology
named after Academician V.I. Kulakov Ministry of Healthcare of the Russian Federation. E-mail: a_tregubova@oparina4.ru. ORCID: 0000-0003-4601-1330.
4, Ac. Oparina str., Moscow, 117997, Russia.
For citation: Kyurdzidi S.O., Khashchenko E.P., Uvarova E.V., Chuprynin V.D., Asaturova V.A., Tregubova A.V. Giant follicular cyst in a teenage girl.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2020; 8: 187-193 (in Russian).
https://dx.doi.org/10.18565/aig.2020.8.187-193